MY MOST DIFFICULT CASE
IN THIS ISSUE:
Medical society launches strategy to renew public trust in physicians
CMS Annual Meeting preview: Join us Sept. 19-20 in Keystone
Celebrating CMS Foundation student scholars
AMA President on federal prior authorization reforms

MY MOST DIFFICULT CASE
Jack Berry, MD, a former CMS president and rural family physician, tells the story of caring for a patient through the heartbreaking loss of her first child and then guiding her through an obstetrical emergency with no assisting physician. It is the quintessential example of a physician who is a compassionate and empathetic healer dedicated to delivering the very best care.



8 REGISTER TODAY FOR THE CMS ANNUAL MEETING
Join us Sept. 19-20 in Keystone for the Colorado Medical Society Annual Meeting — a powerful and timely gathering designed to help physicians navigate the turbulence of today’s health care system. With seismic shifts in policy, changing patient expectations, and blurring of physicians’ professional identity, this year’s conference offers clarity, connection, and practical tools.
9 PRIVATE EQUITY – IMPACT ON OUR HEALTH
CPHP Medical Director Scott Humphreys, MD, discusses the impact of business on medicine and how that has led to loss of control for some physicians, which in turn greatly harms physician wellbeing. CPHP is here to help anyone experiencing work-related stress or burnout, though the Doc2Doc Wellbeing Consulting program or their full services.
24 FINAL WORD: NATION CAN LEARN FROM COLORADO’S PROGRESS ON PRIOR AUTHORIZATION REFORM
AMA President Bobby Mukkamala, MD, writes about how Colorado can serve as a model to the nation on prior authorization reform, and previews the next ask in reducing this administrative burden in the state and beyond.
Hear Dr. Mukkamala speak at the CMS Annual Meeting, Sept. 19-20 in Keystone.
In her last column as CMS president, Kim Warner, MD, shares why she became a physician and a touching example of how building trust in the moment can lead to the best quality care for patients.
Your elected delegation to the American Medical Association attended the June AMA Annual Meeting in Chicago, advancing in national leadership and making a difference in policy discussions. Delegates successfully passed two policies on neurorights and mRNA vaccines.
The CMS Foundation awarded 2025 scholarships to Colorado medical students. The Rural Track scholarship recognizes excellence in first- or second-year students in a rural track program, and the Gilchrist Student Leader Scholarship recognizes services to organized medicine in third- or fourth-year students.
COLORADO MEDICAL SOCIETY
OFFICERS, BOARD MEMBERS, AMA DELEGATES, and STAFF
2024-2025 OFFICERS
Kim Warner, MD
President
Brigitta Robinson, MD
President-elect
Omar Mubarak, MD, MBA
Immediate Past President
Hap Young, MD
Treasurer
Dean Holzkamp
Chief Executive Officer
BOARD OF DIRECTORS
Brittany Carver, DO
Kamran Dastoury, MD
Renee Dreher, MSC
Amy Duckro, DO, MPH
Rachelle M. Klammer, MD
Marc Labovich, MD
Justin McCoy, DO
Michael Moore, MD
Rhonda Parker, DO
Lynn Parry, MD
Sean Pauzauskie, MD
Leto Quarles, MD
Darlene Tad-y, MD, MBA
Hap Young, MD
COLORADO MEDICAL SOCIETY STAFF
Dean Holzkamp
Chief Executive Officer
Dean_Holzkamp@cms.org
Kate Alfano
Director of Communications and Marketing
Kate_Alfano@cms.org
Jen Atchison, BHA, MSDA
Director of Continuing Medical Education and Recognized Accreditor Programs
Jen_Atchison@cms.org
Virginia "Ginny" Castleberry
Executive Director
Denver Medical Society
Virginia_Castleberry@cms.org
Cecilia Comerford-Ames
Executive Director, Colorado Society of Eye Physicians and Surgeons Communications and Marketing Manager
Cecilia_Comerford@cms.org
Dorcia Dunn
Program Manager, Membership Dorcia_Dunn@cms.org
Crystal Goodman
Executive Director, Northern Colorado Medical Society
Crystal_Goodman@cms.org
Mihal Sabar
Director of Accounting
Mihal_Sabar@cms.org
Holzkamp, Executive Editor, and Kate Alfano, Managing Editor.
AMA DELEGATION
David Downs, MD, FACP
Amy Duckro, DO, MPH
Carolynn Francavilla, MD
Mark Johnson, MD, MPH
Jan Kief, MD
Rachelle Klammer, MD
A. “Lee” Morgan, MD
Tamaan Osbourne-Roberts, MD
Lynn Parry, MD
Brigitta J. Robinson, MD
Michael Volz, MD
Patricia Weber, MD
AMA PAST PRESIDENT
Jeremy A. Lazarus, MD
Chet Seward
Chief Strategy Officer Chet_Seward@cms.org
Debra Will Director of Business Development
Debra_Will@cms.org
Your Care is at our Core highlights the sacred bond
between patients and physicians
Kim Warner, MD, CMS President


This will be my last President’s letter as my term ends in September. It has truly been an honor to serve my fellow physicians over the past year, which has gone entirely too quickly. I recall just a few short months ago during my inauguration speech I talked about the magic of being a physician. In times of need, people trust us with their lives. I can’t imagine a greater gift. For the opportunity to be a physician and to have had this role in CMS, I am beyond grateful.
I knew very early on that I wanted to be a physician, and then it became clear that I was meant to care for girls and women. It was my calling, my mission and my duty; being a part of deliveries is impactful. You get to experience one of the most important and sacred moments in families’ lives and ensure health for moms and babies. Sometimes it is not a joyous occasion, such as the early loss of a precious and wanted pregnancy, and I have the privilege of sharing in that journey and guiding families through that care and challenging experience.
Health care is not just about providing medical treatment when someone is sick, but also about promoting overall health and wellbeing to prevent diseases and improve quality of life.
I remember a lovely 68-year-old woman who had not come to the gynecologist in a very long time. She came in very nervous, reserved, shy and withdrawn. We talked for a while about her career as a teacher, her children and life in general. She began to open up. She said she wanted some lab tests, which I ordered. She wanted a breast exam, which she had not had in a while. She wanted me to look at her old

In times of need, people trust us with their lives. I can’t imagine a greater gift.
cesarean section scar, to make sure it was okay. I could tell she was trying to work up to something else she was concerned about, using minor issues maybe to gain trust in me.
Finally, when I felt like she was finished asking me questions, she asked me to take a look at a “spot” on her vulva. It had been there for “years,” but she thought it was fine. I took a look at it, knowing it was probably a cancer, biopsied it, and when it returned a vulvar malignancy, got her the treatment she needed. Because it was an early stage, she has done well for years. I don’t think she would have opened up to me if not for the initial time we spent at the beginning of the visit building trust and rapport.
Regardless of specialty, physicians universally entered the profession to help people live longer, healthier lives. This dedication to patients is at the heart of what it means to be a physician and is central to the new communications effort the Colorado Medical Society is launching with the American Medical Association: Your Care is at our Core
This new communications strategy aims to highlight the sacred bond between physicians and patients. Many Colorado physicians have experienced troubling trends ignited by battles over the Covid-19 pandemic, science and evidence-based care, and the prevalence of mis- and disinformation. These factors have distracted from what matters most – the connection between physicians and their patients.
This strategy is also in line with CMS’s new strategic plan, which includes a goal to increase public trust and understanding of health care. We know that the patient-physician relationship is the foundation of quality care. The multi-media Your Care is at our Core strategy reminds the public that physicians are compassionate and empathetic healers dedicated to delivering the very best care to their patients. Like my patient above, health care can be a vulnerable space, and establishing a meaningful patient-physician relationship is necessary to build trust and provide the most effective care and treatment.
Your Care is at our Core highlights that physicians are patients’ strongest allies in the pursuit of improved health. We hope we can remind the public of “who” physicians are and rebuild an awareness of physicians’ dedication to their patients –all to strengthen the profession, your practices, and our advocacy on your behalf. ■
DO YOU WANT TO HELP IN THESE EFFORTS?
Scan the QR code or email membership@cms.org to share a story of great patient care.

MY MOST DIFFICULT CASE
Jack L. Berry, MD
In the end, it’s all about people’s lives.
In the end, it’s all about people’s lives. How to make them live better, how to make them live longer, and sometimes it’s about how to save them even though in doing so one can’t make their lives better.
It had been the toughest night of my medical career when I came home at 6:30 a.m. and my wife greeted me with the question, “What happened that could have taken all night?” She had lived through many nights of my rural practice when I had been called back to the hospital to deal with problems that might take an hour or two. But this was one of the few nights that I was gone all night, with no other calls, and not returning home at all.
I remember clearly the day I first thought being a doctor might be a good idea. I was 5 years old and a really nice and gentle man, Dr. Thorpe, had just stuck a really painful and seemingly very long needle into my arm. He had been so kind and careful when helping me hold my mouth open to look at my pus-covered tonsils, and very quick to hold and comfort me afterward. Even at my young age, such a caring and compassionate act by a large man who was both helping and hurting me made an indelible mark.
Through my years of primary and secondary education, that memory

grew into the realization that being able to help while sometimes having to hurt could provide the challenge that I was looking for in life. Being a doctor could be a special way to make a good living for my family. One may not find it hard to believe that indelible memory came to me again that exhausted early morning when Maribeth met me with her question. At the same time, I was asking myself, “Why did you ever get yourself into this?” The answer is straightforward but complex as well.
K was a delightfully pleasant and positively dispositioned young woman near the end of her first uncomplicated pregnancy, an obstetrical patient of my partner who had left town a few days
earlier for a vacation. K was in excellent health after following an active and nutritious lifestyle. There had been no reason to anticipate any complication of pregnancy, but near term, she came to my office distraught, not having felt movement for two days. Sadly, on examination I could feel no movement and could hear no heartbeat.
This was 40 years ago and in those days, no ultrasound was available in our small genuinely rural hospital, so K had to travel 90 miles to the closest next larger hospital to prove the fetus not viable. When she returned with the report confirming our worst fears, we cried together and called her husband to come help us decide what to do.


A phone consultation with an ob-gyn friend in Denver helped define our limited options: to induce labor as soon as possible to avoid maternal complications at our rural hospital, or to travel 140 miles to the nearest obstetrician to accomplish the same sad outcome –delivery of a stillborn infant. One must have experienced it to understand the rural physician-patient trusting relationship that led this wonderful couple to choose to stay in our rural town to endure this extraordinarily traumatic experience. And it didn’t get better for them.
Induction of labor, never comfortable, fortunately progressed very quickly, and with terrific maternal effort, she delivered an otherwise normal appearing stillborn infant without difficulty. There, the relatively good fortune ended. As the infant was wrapped in a blanket and placed in their mother’s arms for her to say goodbye, the placenta delivered followed by a gush of blood that filled the gallon basin at my feet. Her uterus would not contract to stop the bleeding despite massage, nor all the medicines that are supposed to do so. Only by heavily sedating the patient and packing her uterus with sponges was I able to slow the bleeding and buy time for the nurse to frantically call our physician assistant and other available nurses to come start another I.V. and call walking donors to give blood for immediate transfusion (this was before modern blood safety practices).
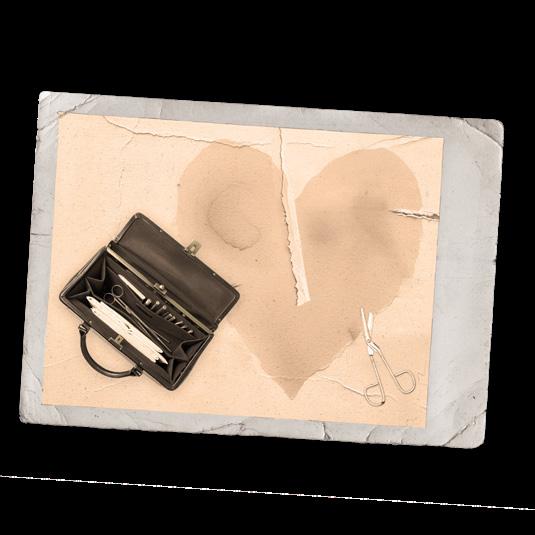
Jack Berry, MD, a CMS past president and past CMS Foundation president, practiced rural medicine in Okarche, Okla., a town of 800, for seven years; Greeley, Colo., for 7 years; and Wray, Colo., for 11 years. He moved to Wray when there was just one doctor and one physician assistant, and through his hard work and mentorship, there are now four family doctors, a general surgeon and many support personnel.
Deeply committed to rural medicine, he ran for CMS president on a platform of improving rural health care and access
to care. Of his many accomplishments, he and his wife, Maribeth, were instrumental in launching a CMS scholarship benefiting students who want to practice in rural areas of Colorado, and a board-certified Family Medicine Rural Track residency – the second in the country.
The Berrys met when Dr. Berry was 17 and Maribeth was 16 at a church rally in his hometown in Oklahoma. He says, “we’re a team; it’s the whole way.”
The couple will celebrate 62 years of marriage in September 2025.
Get to it, doc, and do the best you can ’cause I love her.
Another, this time desperate, phone consultation made it clear that we had tried everything possible and there was no option but hysterectomy. My God! I had just delivered her first pregnancy,
a stillborn infant! I had never before felt this alone as a physician, 140 miles away from the nearest ob-gyn, even though I was trained and experienced in surgical obstetrics. I was going to have to

Sometimes you must first hurt someone to save them. Do it with compassion and they will thank you for it.
irreversibly damage this young woman’s life in order to save her!
K was still heavily sedated, so I turned to her husband to get permission for what we were about to do. This discussion was more trying for me than many of the times that I had to tell families that their loved ones were dying. He responded by doing his best to encourage me, as a rancher who had delivered many calves would, saying “Get to it, doc, and do the best you can ’cause I love her.”
Our “circuit riding” nurse anesthetist was 35 minutes away via his airplane, so while he was on his way and my best nurse carefully monitored the patient, we moved her ASAP to the operating room. I had to do the spinal anesthetic myself, as time was critical. The post-pregnant uterus immediately after delivery is the size of a football and the veins and arteries supplying it are enlarged up to the diameter of a small hose. Though I had seen those blood vessels many times during cesarean sections, fear best describes my feeling as I clamped and cut across them and then sutured without another physician assisting.
To everyone’s relief the patient remained stable until the nurse anesthetist arrived, my first post-delivery hysterectomy went well, and K recovered well. During her recovery, she and her husband seemed determined to assuage the anxiety of my inept attempts to support them at the loss of their childbearing capacity after losing their first infant.
Instead, they reinforced the lesson my first physician had given me by his example: sometimes you must first hurt someone to save them. Do it with compassion and they will thank you for it.
And there was no greater reward than that I received the day that K and her husband brought their first adopted daughter to me for her first well-child exam. ■
Your Care is at our Core: Share your story with CMS
Physicians and patients agree that the doctor-patient relationship is essential to make the best health care decisions. Health care can be an especially vulnerable space for patients, and physicians know compassion and establishing a meaningful relationship are necessary to build trust and provide the most effective care and treatment. Physicians understand that quality time spent listening to, responding to, and treating patients is essential to quality medical care.
voters value the doctor-patient relationship
A recent AMA poll found that 84% of national voters agree that their physician values the doctor-patient relationship and helps them make informed decisions about their health.
79% 83%
voters agree that insurance company bureaucracy makes it harder
79% of national voters agree that insurance company bureaucracy makes it harder for physicians to provide the best care for their patients.
voters agree doctors got into the profession because they wanted to treat patients
83% of national voters agree that doctors got into the profession because they wanted to treat patients: to understand their health care needs, to take the time to understand how to best help them, and then provide the care they need to get better.
That's why doctors are working to change the system–to get back to the way it should be, so that patients and doctors have the time together to make the best health care decisions. 84%
The Colorado Medical Society (CMS) is proud to launch Your Care is at our Core, in partnership with the American Medical Association (AMA). This new communications strategy highlights the sacred bond between physicians and patients, especially following challenging years during which there has been an erosion of trust in science and medical institutions that can spill into the exam room.
To support this new effort, we are asking physicians to share stories that illustrate your strong patient-physician relationships and how they helped you deliver the best care. Visit the CMS website by scanning the QR code for question prompts to get you started.


The Colorado Medical Society invites you to the 2025 CMS Annual Meeting
SEPT. 19-20 IN KEYSTONE, COLORADO!
Cecilia Comerford-Ames, CMS Communications and Marketing Manager

This year’s meeting offers outstanding educational sessions, thought-provoking discussions, and valuable networking with fellow physicians. It’s also a chance to step away from the daily grind, recharge in the stunning Colorado mountains, and spend meaningful time with colleagues – friends, family, and your loved ones – before the busy fall season kicks into gear. All events will be held at our host hotel, Keystone Lodge. Get preferred pricing for lodging through our group rate, available until Aug. 26 or as space allows.
The signature event of the weekend is Saturday evening’s Presidential Gala, featuring the passing of the gavel from outgoing CMS President Kim Warner, MD, to incoming president Brigitta Robinson, MD. This year's theme is Prom: Black Tie; White Coats. Gaudy tuxes and tulle welcome, but optional! We will get ready for the big event by selecting our CMS Prom Court during the opening reception on Friday night.
Whether you come to learn, connect, or have some fun, there is something for you and we cannot wait to welcome you!
AGENDA
FRIDAY:
• The CMS Board of Directors meets Friday afternoon. This is the final quarterly meeting of the CMS Board of Directors in 2025, and will be offered as a hybrid meeting for in-person or virtual participation. All meetings are open to all CMS members to attend.
• Welcome Reception! Join us Friday evening for networking and socializing. Also, participate and a friendly game of trivia to win prizes and maybe a spot on the CMS Prom Court.
• All CMS members, especially medical students and residents, are invited to display your research in three categories – primary research, case report and evidence-based review –starting Friday evening. Posters will be judged Saturday and winners will be announced. Register for the poster competition when you register for the meeting. More information is available on the event webpage, or email membership@cms.org.
SATURDAY:
• Join us for breakfast, starting at 7 a.m.
• Educational sessions start at 8 a.m. and will include hot topics such as impacts of federal legislation on Colorado, rebuilding public trust in physicians, reputation management, ethics in advocacy, and more. We will have great speakers all day that include Carolynn Francavilla-Brown, MD, FOMA, Kamran Dastoury, MD, and Matthew Wynia, MD, MPH.
• We are especially pleased to welcome American Medical Association President Bobby Mukkamala, MD, as our featured presenter.
• The COMPAC lunch highlights our Defender of Medicine award recipients.
• Get ready for CMS prom at the President’s Reception and Gala! This glamorous themed event features a buffet dinner, decadent dessert spread, DJ and dancing, and time with peers.
Childcare will be provided on Saturday from 8 a.m. to 1 p.m. and Saturday from 5-8 p.m. In the morning there will be an organized outside activity for children. Make sure to sign your kids up when you register so they can enjoy time with peers. Do you need additional care? Contact membership@cms.org for options.
THINGS TO DO IN KEYSTONE
HIKE: There are several trails that start from the Keystone Gulch Trailhead –including a seven-mile hike with over 1,000 feet of elevation change and a 1.6-mile loop around the lake right outside of the Keystone Lodge. If you want to wake up and grind, Grays and Torreys peak is only a 40-minute drive away. This is a great way to get two 14ers in only one hike. Note: while it is only a class 1, these are still difficult hikes at 14,000 feet, so come prepared!
BIKE: Keystone Bike Park is open for extended hours Sept. 19-21 before closing for the season. Professionally maintained, progression-focused terrain welcomes riders of all abilities, from the progression park to technical rock gardens, drops, and high-speed features. Purchase of a one-day lift ticket is required.
GOLF: Keystone Ranch Golf Course is a great place to play 9 or 18 holes.
LAKE ACTIVITIES: Enjoy kayaking, paddleboarding, and more on Keystone Lake.
RELAX: Explore offerings from Alpenglow Spa at Keystone Resort: massage therapies, facials, foot soaks, body treatments or the sensory deprivation float tank.
Visit our event webpage, CMS.org/events/CMS-Annual-Meeting for more details and to register. ■

Private equity –impact on our health
Scott Humphreys, MD

Historically, medicine and business were purposefully separated. The physician fulfilled their obligation to ethics and their community, and a fair reimbursement was expected. Advertising was not necessary – everyone knew where to find their local doctor or hospital. Much of medicine was supportive rather than curative and patients, for the most part, understood this.
But in recent times medicine has become potent and curative. Now, a procedure or physician’s judgment can routinely make the difference between life and death. Medicine offers other ways to cheat death by lengthening our lifespans in a way not previously possible. The promise of a lengthened vigorous life makes people desperate. Desperate people are willing to pay.
Pharmaceutical companies, insurance carriers, hospital systems, and a myriad of affiliated services like electronic medical records soon found that not only were there fortunes to be made in medicine, they would perish if not actively participating in this arms race. Capitation through managed care, billion-dollar endowments, and maneuvers like “upcoding” became the norm. Many of our doctor colleagues decided this was a good time to retire. Somehow, those of us who stuck around found our way. We did not like the ever-increasing bureaucratic demands but in general, our relationships with our patients were
preserved and we were treated as the leaders we are.
Over the past ten years at the Colorado Physician Health Program (CPHP), we have heard a term more and more: “private equity.” The heaviness with which the phrase is delivered is immediately noticeable.
Basically, medicine’s successes have not gone unnoticed by the business world. If classic business-school practices can be applied to pharmaceutical, medical equipment, and insurance, why can’t they be applied to the doctor-patient delivery of health care? So, they started buying our practices. Literally overnight, a physician can go from being in charge of their clinic – medical decisions, staffing, patient flow, etc. – to no longer having control of any of that. Studies, lab work, and consultations are all scrutinized through the optics of the financial bottom line.
It has long been determined that the stress of any job is the ratio of responsibility to control. In the distant past, medicine was not considered a stressful profession. Over the past couple generations of physicians, we have gradually traded lifestyle for control. Not a terrible trade if we maintained an adequate amount of control. Through my experi -
Medicine’s successes have not gone unnoticed by the business world.

ence at CPHP, it appears private equity can disrupt this balance in a way which the physician cannot compensate. We are seeing many previously level-headed physicians referred for disruptive behavior with “a change in practice ownership” being one of the chief complaints.
I don’t pretend to have a sweeping solution for these challenges. But I think it is important for all of us to have an awareness of how a change in practice ownership can not only affect our practice environment but our health itself. If you have recently gone through a similar transition or anticipate one, please recognize that CPHP is here to help you. ■
The Colorado Physician Health Program (CPHP) and the Colorado Medical Society partner to provide Doc2Doc Wellbeing Consulting, a peer-to-peer program that supplements CPHP’s extensive services with pre-clinical support without lengthy documentation or an extensive evaluation. Any Colorado physician or medical student can call 720-810-9131 24/7 to speak to a masters-level licensed clinician and schedule a confidential appointment with a physician trained in psychiatry (in person, video or phone call, depending on preference). Discuss any concern — stress, burnout, relationship issue, or poor outcome.
Learn more at cphp.org.
You have a voice in the American Medical Association
REPORT FROM THE JUNE 2025 AMA ANNUAL MEETING
Rachelle Klammer,
MD

Your elected delegation of Colorado physicians traveled to Chicago in June to represent you at the American Medical Association House of Delegates meeting and conduct other business on your behalf. We are grateful to these volunteer physician leaders for their time and dedication to organized medicine.
COLORADANS ARE ACTIVE IN NATIONAL LEADERSHIP
• Jan Kief, MD, became chair of the Council on Long Range Planning & Development after a term as the council’s vice chair.
• Tamaan Osbourne-Roberts, MD, was elected chair-elect of the Council on Science and Public Health.
• Carolynn Francavilla-Brown, MD , completed her term as chair of the AMA Private Practice Section.
• Jeremy Lazarus, MD, a past president of CMS and the AMA, completed his term as chair of the AMA Council of Ethical & Judicial Affairs.
• Dr. Lazarus and I serve on the AMA Foundation Board of Directors. Dr. Lazarus has been elected president-elect of the Foundation Board and I have been elected Secretary.
• Jacob Altholz, MD , completed his term as Speaker of the Resident and Fellow Section (RFS) and was newly appointed to the AMA Council on Legislation.
• A. Lee Morgan, MD, completed her term as District Councilor for PacWest, our region within the AMA, and I was elected to the position.
• Two new residents joined our Delegation this year, Joshua Bilello, MD, and
Lavanya Easwaran, MD, MPH
• Medical student Pritika Parmar attended the AMA House of Delegates as a regional delegate for the Medical Student Section.
COLORADO IS CHANGING NATIONAL POLICY
Three resolutions brought by Colorado physicians were passed by the AMA House of Delegates
• Resolution 503, “Safeguarding Neural Data Collected by Neurotechnologies,” codifies physicians’ strong support for legislative and regulatory efforts to protect neurotechnology users from potential harm, and it formalizes a specific definition of neural data as “information obtained by measuring the activity of a person’s central or peripheral nervous system through
Attendees at the AMA Inaugural Dinner, Clockwise from left: Dave Downs, MD, Debra Parsons, MD, and Trish Weber, MD. Rachelle Klammer, MD, and Kim Warner, MD. Tamaan Osbourne-Roberts, MD, and Jeremy Lazarus, MD.



the use of neurotechnologies,” not including “data inferred from non-neural information.” Read more about this policy in the sidebar.
• Resolution 411 , “Protecting Access to mRNA Vaccines,” directs the AMA to actively lobby for protections for the use, research and development of mRNA vaccines for infectious diseases and cancer treatment; and to develop state-level model legislation to promote state-level protections for use, research and development of mRNA vaccines, with a report back at the AMA Interim Meeting in November.
Fun fact
Within the AMA, Colorado is part of the PacWest Conference. PacWest also comprises the following states: Alaska, Arizona, California, Guam, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington and Wyoming.
Colorado physicians successfully pass national resolution protecting patients’ neural data
The American Medical Association (AMA) House of Delegates unanimously adopted a new policy at their 2025 Annual Meeting in Chicago on June 11 to protect patients’ neural data.
The resolution was brought forth by Lynn Parry, MD, MSc., a private practice neurologist in Littleton, and member of the Colorado Delegation to the AMA. The resolution is based on a first-in-the-nation law passed in Colorado in 2024 that was championed by Sean Pauzauskie, MD, a hospital-based neurologist with UCHealth in Fort Collins, and then-Rep. Cathy Kipp.
Resolution 503, “Safeguarding Neural Data Collected by Neurotechnologies,”

codifies physicians’ strong support for legislative and regulatory efforts to protect neurotechnology users from potential harm. Additionally, it formalizes a specific definition of neural data as “information obtained by measuring the activity of a person’s central or peripheral nervous system through the use of neurotechnologies,” not including “data inferred from non-neural information.”
Reflecting on the effort to pass the historic policy, Dr. Parry said: “It was due to the extraordinary efforts of Dr. Sean Pauzauskie and the Neurorights Foundation that the Colorado Medical Society not only had a policy on defining and protecting personal neural data but also succeeded in advocating for the state of Colorado to become the first in the nation to extend its state consumer data privacy law, the Colorado Privacy Act, to protect neural data. It was, therefore, a great privilege for the Colorado Delegation to the AMA House of Delegates to drive the adoption of this critical resolution that, with the support of the American
IN THE NATION TO PROTECT NEURAL DATA
Academy of Neurology, has now become a new policy of the American Medical Association.”
Dr. Pauzauskie, who also serves as medical director of the Neurorights Foundation, said: “The AMA’s new policy represents a defining moment for the protection of patient and consumer neural data – in addition to its clear language on what does and does not constitute neural data, paving the way for further state and federal efforts, it also opens the next frontiers of fair access to and freedom from bias from neurotechnologies. We applaud the AMA’s leadership in so clearly focusing global attention on these critical questions.”
CMS President Kim Warner, MD, was recognized on stage at the AMA Inaugural Dinner with other state society presidents.
• Emergency Resolution 1001, “Advisory Committee on Immunization Practices,” brought by the Colorado Chapter of the American College of Physicians, directs the AMA to advocate in support of the ACIP, immediately calling for the Secretary of Health and Human Services to reverse the dismissal of the former ACIP representatives; calling for the Senate Committee on Health, Education, Labor and Pensions (HELP) to investigate the actions of the Secretary regarding his administration of the Centers for Disease Control and Prevention and ACIP; and identifying and evaluating alternative evidence-based vaccine advisory structures to invest resources in such initiatives.
AMA LEADERSHIP UPDATES
• Bobby Mukkamala, MD, an otolaryngologist from Flint, Mich. was sworn in as the 180th President of the AMA.
He will be the keynote speaker at the 2025 CMS Annual Meeting in Keystone Sept. 19-20.
• John Whyte, MD, MPH , is the AMA’s new CEO/EVP, taking over for James Madara, MD, as of July 1. A board-certified internal medicine physician for nearly 30 years, Dr. Whyte served as chief medical officer of WebMD and in various roles at the Centers for Disease Control and Prevention, the Centers for Medicare and Medicaid Services, and the Department of Health and Human Services.
• Outgoing AMA President Bruce Scott, MD, an otolaryngologist from Kentucky, gave a fiery speech during which he listed his frustrations with a health care system that is failing physicians and, more importantly, patients. The recording of his speech can be viewed on the AMA’s website.
Colorado’s Delegation is highly respected within our district and region of the PacWest. We have very good leadership in the Councils and our early career physicians, residents, fellows and medical students are very active and engaged. We may not be the largest Delegation with six Delegates and six Alternate Delegates, but we continue to make an impact.
Truly, everyone has a voice at the AMA. There is a misconception that the orga -

CMS incoming president Brigitta Robinson, MD, poses with her AMA campaign poster.
nization serves only retired physicians, or only physicians who lean left or right politically. Decisions are made by those who show up. So please, if you're not an AMA member, I urge you to join. Not convinced? Reach out to any of us on the Delegation about why your membership matters. View the list of your Colorado Delegation on page 2 of this issue and be sure to vote to affirm your elected representatives during the CMS leadership election in August.
There is much more coverage of the AMA Annual Meeting, including recordings of inspirational speeches, on the AMA’s website, www.ama-assn.org. ■
Left to right : Colorado Delegate to the AMA, Lynn Parry, MD, advocates on behalf of a resolution she brought to the AMA, “Safeguarding Neural Data Collected by Neurotechnologies,” that was based on a law passed in Colorado in 2024. First-year resident Dakota Hitchcock, MD, testifies before the AMA House of Delegates. Many guests embraced tradition and celebration at the AMA Inaugural Dinner and Dance, donning formal Indian attire at the invitation of the incoming AMA President Bobby Mukkamala, MD, who shared this meaningful expression of his heritage.








Investing in the future of medicine: CMS Foundation scholarships for medical students
Cecilia Comerford-Ames, CMS Communications and Marketing Manager
Every year, the Colorado Medical Society Foundation (CMSF) proudly awards scholarships to promising future physicians. CMSF offers two distinguished scholarships: the Rural Track Scholarship and the Gilchrist Student Leadership Scholarship.
The Rural Track Scholarship financially supports students in good academic standing who are completing their first or second year in a rural medicine track program at a Colorado medical school. This scholarship aims to encourage and assist those committed to serving rural communities.
The Gilchrist Student Leader Scholarship provides financial assistance to third- and fourth-year medical students who have made significant leadership contributions to organized medicine. This scholarship recognizes their dedication and outstanding achievements.
Below are the 2025 scholarship awardees who have already made incredible contributions to benefit their communities and show great promise for the future of health care.

Growing up in Estes Park, future doctor Dumont witnessed firsthand the challenges of rural medicine – from hearing about the helicopter evacuations during the 2013 flood to the recent loss of key local health services. Now a medical student, he is committed to returning to rural Colorado as a primary care physician. His future research will focus on cancer detection tools adaptable to low-resource settings, and he advocates nationally for rural health policy. From representing rural voices at the AMA’s advocacy conference to studying gaps in care during his rural hospital immersion, he is dedicated to ensuring small communities like his have access to the care they deserve.
A small-town Oregon native, future doctor Wavrin chose RVU in part for its Rural and Wilderness Medicine Track, drawn to the opportunity to serve communities like the one that raised her. Now preparing for clinical rotations in Grand Junction, she envisions a future practicing rural medicine in Colorado – ideally owning a clinic, offering house calls, and even bartering for services when needed. Passionate about building lasting patient relationships and integrating into rural life, she is especially attuned to the needs of rural areas. With deep roots already forming in Colorado, she is committed to advancing accessible, compassionate care in the state’s rural communities.




Over the past year, future doctor Haley Hemstreet has lived and trained in Trinidad, Colo. From helping deliver a baby in Raton to following that child’s care in Trinidad, she has experienced the full spectrum of rural family medicine. Inspired by her grandparents’ struggles to access care in rural New Mexico, Hemstreet is committed to serving small towns like Trinidad. The kindness of the community, deep patient relationships, and hands-on learning have affirmed her decision to pursue family medicine. She looks forward to returning to Trinidad as a rural physician in the future.




AMANDA WINTER

Growing up in Buena Vista, future doctor Winter developed a deep connection to rural Colorado and the health care challenges its communities face. Her path to medicine began as an EMT in El Paso County and continued through work in a Level 1 trauma center and medical missions abroad. These experiences fueled her passion for rural medicine and her commitment to serving underserved populations. Now a student in RVU’s Rural and Wilderness Medicine Track, she plans to return to a community like Buena Vista – combining her love for the outdoors, strong patient relationships, and broad-scope care to help address the physician shortage in rural Colorado.
GILCHRIST SCHOLARS

Having recently completed medical school at Rocky Vista University, future doctor Bussard has distinguished himself as a passionate leader in organized medicine. As one of the student leaders of the Colorado Medical Society Council on Legislation, he played a role in passing Colorado’s prior authorization reform bill (HB24-1149), advocating directly with lawmakers and the media. He served as co-chair of the CMS Medical Student Component and president of the CMS RVU Chapter, where he launched public health fundraisers and student engagement initiatives. A recent inductee into Omega Beta Iota, he is committed to advancing health care policy, equity, and access through advocacy and service.
CONTRIBUTE TO THE FOUNDATION
From founding her university’s American Medical Women’s Association chapter to testifying on opioid legislation, future doctor Heister has long championed inclusion and advocacy in medicine. She co-led efforts to support underserved communities and underrepresented students while working to bridge gaps in health education. Her policy journey continued at the CU School of Medicine, where she co-led the CMS student chapter, joined the Northern Colorado Medical Society board, and advocated for payment reform at the AMA National Advocacy Conference. With deep roots in grassroots organizing and legislative action, she exemplifies the power of collaborative leadership in shaping a more equitable and responsive health care system.

On Feb. 25, 2025, future doctor Laughlin drove from Sterling to Denver to testify at the Capitol in support of a bill promoting physician wellbeing. A Colorado native and medical student passionate about advocacy, she’s previously testified at AMA national conferences and served in student leadership roles with the Colorado Medical Society. Now training in rural Sterling, she’s inspired by physicians delivering full-spectrum care and supporting her passion for policy change. That day at the Capitol, her advocacy came full circle as the bill passed – affirming her belief that engaged, well-supported physicians are key to strengthening care for patients across Colorado.
CMSF needs your support to support the future of medicine. Visit cms.org/contribute to contribute or add a donation to your annual dues when you receive your 2026 membership invoice in September.
Letter to the editor: The imperative to advocate for universal healthcare

As we sink deeper into the healthcare crisis and likely reduction of federal funding, Colorado solutions to providing healthcare to all becomes more critical than ever. We want to ensure that patient healthcare needs are protected and met in Colorado, even if the proposed deep cuts to Medicaid occur.
On reviewing the winter edition of Colorado Medicine, we see that the Colorado Medical Society is greatly concerned with reform of our healthcare system to benefit all Coloradans. As Dr./President Warner wrote in her article on advocacy in medicine, “Together, we can ensure that the needs of our patients drive the future of healthcare in Colorado.” As Dr. Kornas wrote in her essay, “There is no more important or more urgent priority than protecting the health of the people of Colorado.” And CMS’ mission statement is, “To champion healthcare issues that improve patient care…and create healthier communities in Colorado.”
In fact, CMS is very active and successful in helping Colorado physicians, as it should be. However, it is less active in advocating for better access to care and
What are we if we cannot dream of a more equal and healthy life together?
improvement of healthcare for all Coloradans. This is complicated by the shutdown of Central Line since July 2024, apparently due to website glitches. Grassroots advocacy is therefore stymied.
The passage of the SB25-045 legislation this session mandates that the Colorado School of Public Health will study the feasibility of a healthcare system to cover all Coloradans. The study will be paid for by donations and grants with the money to be raised in the next few months. Here is a link to the bill: https://leg.colorado.gov/ sites/default/files/documents/2025A/ bills/2025a_045_rer.pdf. We hope it will help to define a path forward.
Working to preserve and protect Medicaid is vitally important, but it is not enough. There are real threats to other beneficial programs including Medicare, CHIP, and VA care. We must advocate to improve our healthcare system and provide affordable access to care. As Dr. Warner states in her essay, “Advocacy is the backbone of our profession. It shapes policy, protects our ability to care for patients, and ensures that healthcare policy is heavily influenced by physicians.”
All of us yearn for connected lives that finally provide peace and meaning. Universal healthcare is such a connection. What are we if we cannot dream of a more equal and healthy life together?
Accordingly, we the undersigned CMS members ask CMS to up their game of advocating for healthcare justice and reform, including considering, discussing, and supporting such reform, and encouraging physician activism and advocacy.
We hope CMS agrees with the urgency of these issues.
Laird Cagan, MD
Greg Feinsinger, MD
Jonathan Ward, MD
Cliff Watts, MD
Les Reitman, MD
Michael McClellan, MD
Drew Updike, MD
Steven Thorson, MD
Brianna Anthony, DO
Phil Weber, MD
Keana Kast, medical student ■


Venipuncture
Marren Kirkpatrick

Marren Kirkpatrick is a rising OMSII at RVUCOM in Parker, Colo. A 23-yearold Colorado native originally from the Springs, she earned her bachelor’s in science at Creighton University as a criminal justice major. While she was there, she had the opportunity to work as a phlebotomist for two years at Children’s Nebraska and do four years of forensic psychology research. She is deeply passionate about stories in every form they take (film, video games, books, D&D, etc.). She has been writing poetry for her own mental health since late high school, and this is her first-ever published work. Should you find yourself in need of a haunted-house-loving poet building their medical knowledge, she can make herself available. She hopes her poetry speaks to you.

This piece comes from my time as a phlebotomist at a children’s hospital during undergrad. We did inpatient and outpatient draws, so I saw many different patients in many different conditions. This is my attempt to juxtapose the taught language of medicine with the unsaid traumas that come with it, and show some of the pain that comes with that juxtaposition. Drawing labs on a generic healthy adult patient is very different from critically ill, injured, or combative patients. It can be very emotionally challenging to even get that simple lab done. But at the same time, it’s Tuesday, other people need you. I’m simultaneously the human holding a kid’s hand as they go through a scary thing, and the scary thing they are trying to get away from. This piece tries to make sense of that contradiction for me and hopefully speaks to other providers.
I’m going to teach you to draw blood
First, you take your tourniquet (or big rubber band in peds)
You tie it tight against their bicep (measure their muscles, give their arm a hug)
You tell them this is the worst part (for some, this is true)
You feel for vulnerable veins (like a trampoline under your finger)
Second, you clean with alcohol (it can help cover smells)
You go quickly in circles around your point (take time to remove dirt if it’s there)
You wait for it to dry (this will be quick)
You watch the pumping of their heart (not the movement of their bones)
Then, you poke (just a quick pinch)
You take the cap off the needle and insert (move quickly to prevent injury to others)
You wait patiently to fill your tubes (promise it will be over soon)
You listen to them breathe (or scream)
Finally, you remove your needle (1-2-3, snap!)
You cover with gauze or cotton (they do not want to see their blood)
You apply pressure and a bandage (this will leave a bruise)
You smell the iron as you leave (move on to the next patient)
For capillary, warm the area with a hot pack (it is wise to get ready here)
You prepare your space (plushes should be moved to avoid mess)
You take their hand, palm to palm (or their heel, toes curling into your thumb)
You feel for the warmth in their touch (if they fight, that’s a good sign)
Then, take the lancet and press (the gauge is larger than an IV)
You wipe the first drop (make sure the drop is large enough)
You squeeze and collect in the container (don’t slow down, you may have to poke again)
You might taste it in the back of your throat (make sure you get enough)
Lastly, once collected place cotton or gauze (just a moment longer)
You apply pressure and a bandage (cover every mark, every blackened fingertip)
You label your specimens (ignore mom praying on her knees)
You’ll hear the signal for your next draw (thank yous as you slip out the door) ■

Advocacy: A marathon fueled by hope
Nickole Moon, PhD


Nickole Moon is a fourth-year medical student in the Medical Scientist Training Program at the University of Colorado School of Medicine. She harnessed her passion for advocacy by co-founding the charitable organization, SeizingPsych, while completing her undergraduate degree at the University of Pennsylvania. She has completed her PhD and is now applying to psychiatry residency programs. She hopes to spend her career investigating the developmental mechanisms that underlie mental illnesses, while serving and advocating for a patient population close to her heart.
Government retribution has historically been a coercive force encouraging physician silence or active cooperation; yet history has shown what happens when physicians do not advocate against state efforts to harm patients and violate human rights.
When are health professionals ethically obligated to engage in public advocacy?
Commentary in The Lancet. 20251
Science and medicine are easy to take for granted – but they are not guaranteed. Today, both are under threat from political decisions that endanger the people they are meant to serve, including families like mine.
As an MD/PhD student in my clinical year at the University of Colorado School of Medicine, I expected long days, night shifts, and hours of exams. I expected to meet strangers I would care for, empathize, and connect with. This is the privilege of becoming a doctor. However, I did not expect to see health care jeopardized by government officials and legislators. I did not expect the policies that followed inauguration day.
In January, President Trump's executive orders told me, a medical student, to deny care to people with certain identities – and I feared for my patients 2. In February and March, I read orders to federal grant reviewers banning nearly 200 words, including “women,” “female,” and “underrepresented,” and statements from the Department of Education labeling diversity in education as a nebulous concept 3-5 . Such orders and statements indicated that as a woman from a disadvantaged background, my health and experiences are not valuable or worth
understanding – and I feared for myself and the future of medical education. In May and June, I advocated for families living with mental illness. They worried over legislation that could cut their children’s disability insurance, rendering them without access to medications that maintain their fragile connection to reality – and I feared for families6-8
I also fear because I am the sister of someone living with schizophrenia. Schizophrenia is a mental illness that causes delusions, hallucinations, and cognitive difficulties. Schizophrenia traded my brother’s college dorm for a room without shoelaces or wires, living in a mind he couldn’t trust, in fear of voices in his head. His recovery began at the National Institute of Mental Health, and his current psychiatrist works at a grantfunded institution. As I watch federal NIH, CDC, and other leaders removed and silenced, and observe as active grants are paused or retracted, I fear for my brother and the thousands like him 9-12 I fear because I know that their futures depend on federally funded programming. In 1900, JAMA’s editors warned us about a future without scientific studies or evidence-based practice; they called on physicians and scientists to make their voices heard in the communities in which
they live or else [we will] give them over to others less qualified, and only mischief can follow 13 . Given my experience, that mischief is best equated with greater suffering of the innocent and vulnerable.
Today, I advocate for scientific research because of schizophrenia, and because of families and patients like mine who deserve better answers, answers that require rigorous research. I advocate for scientific research because I watched helplessly as schizophrenia placed my brother on 24/7 suicide watches for weeks, while the voices told him they killed his family. They told him every day to kill himself. He asked, “Why me?”
I advocate because although my brother is now stable, he still lives with intractable OCD and anxiety. He wonders if he will die of the side effects of his medication for schizophrenia or from the schizophrenia itself. He asks, “When will there be better options?”
I advocate for scientific research in support of countless families whose loved ones are hospitalized, who try medication after medication, who find themselves on a “journey” through psychosis that holds their loved ones’ minds hostage, steals their children’s childhoods, and robs their
finances. And I ask, “How can we support families and relieve suffering?” The answers we all deserve require research.
While my family’s story is not unique – 20 percent of people experience mental illness – it is one of many reasons to advocate for science, as scientific innovations touch all lives, and provide hope in the darkest moments14. However, advocacy is not a sprint, it is a marathon. If we are to continue to lead the world in innovation and health care, advocacy efforts must persist. The first step to engaging in these efforts is to muster your hope, and realize your reason to fight for science, be it the environment, safe technology, your family’s health, or an infinite number of other needs yet to be met in the world.
Seasoned advocates cannot run this marathon alone, nor can today’s issues be dependent on the passion of upcoming and future generations. They need you to fight for your own future, lifesaving medications, safe neighborhoods, and discoveries we have yet to uncover. They need you to share how science impacts your life and your patients – why this marathon is worth running. They need you to run beside them, and this is no small ask. It means discussions with those who disagree with you. It means overcoming obstacles and deadlines when you have a hard time making time to write to your representatives. It means continuing to engage people when you aren’t sure what might come next. Spark curiosity. Stifle fear with hope. Share why research matters. It will be exhausting, but it is worth it because research impacts each of the 340 million people
living in the United States, including you. As a practitioner or scientist, your advocacy for rigorous research and evidence-based care not only upholds the principle of beneficence but stirs hope and emboldens voices that may otherwise be silent.
For me, I will be here running this marathon tomorrow, and the next day, and next year, because families like mine don’t have the option to stop running. They need research. They need a voice. They need hope. ■
Citations:
1 Wynia, M.K., M.E. Peek, and M. Heisler, When are health professionals ethically obligated to engage in public advocacy? The Lancet, in press.
2 Trump, D., Defending women from gender extremism and restoring biological truth to the federal government. 2025, The White House.
3 Lee, B.Y., These 197 terms may trigger review of your NIH, NSF grant proposals., in Forbes. 2025.
4 Trainor, C. 2025 February 18, 2025; Available from: https://www.ed.gov/ media/document/dear-colleague-let ter-sffa-v-harvard-109506.pdf.
5 Guerra, P., F. De Maio, and C.G. Streed, Facing political attacks on medical education — the future of Diversity, equity, and inclusion in medicine. New England Journal of Medicine, 2025. 391 (10): p. 941–944.
6 Anderson, J., Pennsylvania advocates warn of devastating impacts as federal Medicaid cuts loom , in Pittsburgh Post-Gazette. 2025.
7 Bartels, M., How massive Medicaid cuts will harm people’s health, in Scientific American. 2025.
8 Bimestefer, K. Understanding the Impact of Federal Funding Cuts to Medicaid. 2025; Available from: https:// hcpf.colorado.gov/impact-of-federalfunding-cuts-to-medicaid.
9 Kaiser, J. In further signs of NIH turmoil, top official suddenly retires ScienceInsider, 2025.
10 Stolberg, S., Top N.I.H. official abruptly resigns as Trump orders deep cuts, in New York Times. 2025.
11 Wadman, M., RFK Jr.'s purge of CDC vaccine advisers prompts outrage ScienceInsider, 2025.
12 Kaiser, J., Trump administration purges U.S. health agency leaders. ScienceInsider, 2025.
13 Keen, W., The ideal physician. JAMA, 1900. 34 (25): p. 1592–1594.
14 NIMH. Mental Illness . 2024; Available from: https://www.nimh.nih.gov/ health/statistics/mental-illness#:~: text=It%20is%20estimated%20 that%20more,of%20the%20U.S.%20 adult%20population).

Reflective writing is an important component of the University of Colorado School of Medicine curriculum. Beginning in the first semester, medical students write essays, stories or poetry that reflect what they have seen, heard and felt. The Reflections column was co-founded by Steven Lowenstein, MD, MPH, and Tess Jones, PhD. It is now co-edited by Dr. Lowenstein and Kathryn Rhine, PhD. It is dedicated to the memory of Henry Claman, MD, Distinguished Immunologist and Professor at the University of Colorado, and founder of the Arts and Humanities in Healthcare Program.
A glimpse inside Copic’s legislative advocacy work
Gerald Zarlengo, MD, Chairman & CEO Copic Insurance Company
Since the early years of Copic, we have recognized not only the importance of, but the need for legislative advocacy in medicine and health care delivery. It has become progressively harder to navigate the legislative process and the surrounding politics. These challenges elevate the need to bind closer to our partners, like the Colorado Medical Society, to raise awareness of the challenges confronting physicians, thoughtfully engage legislators, and use our position to champion ideas that improve health care.
Copic’s long-term investment in legislative advocacy is led by our Public Affairs team. They manage the resources and relationships that focus on key issues that align with our expertise such as professional review, licensing, new duties and requirements, liability, and so much more. As the political landscape changes, our commitment to this work remains a foundation for how Copic’s mission is put into action and used to protect and strengthen health care.
THE MANY FORMS OF ADVOCACY
Legislative advocacy requires complex coordination, relationship building, and a multi-faceted approach. A typical day can start with poring over the details of newly introduced legislation and then end with a presentation to physician leaders on policies that shape health care delivery. It is a year-round endeavor that moves at a rapid pace during the legislative session, but also entails consistent engagement during the months between.
Over the years, we have learned how critical engagement is for our success. This includes engaging our communities to build awareness about Copic, why we are dedicated to protecting access to quality care, preserving the physician-patient
relationship, and maintaining the ability to review and improve care and how legislation can impact any or all of these priorities. Engagement also takes the form of cultivating statewide relationships with key stakeholders (e.g., elected officials, advocacy partners, community organizations, etc.) to build trust and to share how their neighbors, citizens, or members are impacted by legislation. Last, and most importantly, engagement must include our insureds – the physicians providing preventative, specialized or emergency care. This may take the form of direct connections, virtual discussions, or direct communications to make sure our physicians are aware of how laws change and what it means for them.
MONITORING LEGISLATION
At the core of our legislative advocacy efforts is monitoring legislation. Every year, there are countless bills brought forth that have the potential to impact health care. Our Public Affairs team


along with Copic legal/medical experts review and analyze draft and proposed legislation. It’s an in-depth task that involves scrutinizing language, gathering research, considering intended (and unintended) consequences, and bringing in different perspectives. This involves working closely with partners, such as the Colorado Medical Society and Colorado Hospital Association, to represent the health care community, the medical providers on the frontlines, and the patients they serve.
Our work tracks alongside the progression of bills through the legislative process. As we monitor changes, we are weighing in with recommendations and having discussions with legislators and partner organizations to ensure that decisions about health care in Colorado are well-informed and consider the relevant perspectives.
Legislative advocacy requires complex coordination, relationship building, and a multi-faceted approach.
When explaining Copic’s legislative and other broader advocacy efforts, we often highlight “the 4 Cs” that guide our approach:
Convening is about how Copic serves as a catalyst to connect diverse stakeholders – from rural physicians and patient advocates to hospital administrators and insurance providers. Getting the right people in the room is often the biggest challenge. It is an essential step for examining an issue to better understand the different parts and recognizing how different interests can align or conflict with one another.
Collaborating focuses on how Copic can utilize the strengths and resources of those who come together to move the best ideas forward. This collective view generates insight and action beyond what occurs when individual organizations operate on their own. It also reinforces the value of looking past our own perspective by listening to others and the insight they offer.
Coordinating is about the alignment of people, resources, and ideas. For Copic, this includes connecting physicians and other medical professionals with their legislators and facilitating interactions that strengthen awareness on key issues. The Humanitarian Award, an annual award that we present with the Colorado Medical Society to a volunteer physician who is making a difference in their local community, is a great example of honoring amazing humans, lifting up the great work of physicians, and connecting them with their legislators.
Communicating refers to how we share our expertise and experience. Copic’s access to information, such as claims data and best practices, is valuable in identifying risks and allows us to develop programs or resources to address these. The knowledge we gain from legislative advocacy is disseminated across the health care community in actionable ways that support better outcomes.
Medical Transcription Services
Busy vs. Kinda Sorta Maybe Busy

Copic’s legislative advocacy efforts are a testament to our unwavering commitment to supporting the health care community. Through monitoring legislation, engaging with stakeholders, and utilizing the 4 Cs framework, we strive to protect and advance the interests of medical professionals and patients alike.
Eligible Colorado Medical Society (CMS) members can receive up to a 10% premium discount on Copic policies. Get more information on CMS membership by contacting membership@cms.org. ■
Few can contest physicians and healthcare providers when they say they’re busy. They truly are. They barely have seconds to scarf down vending machine chips for lunch, let alone transcribe their patients’ medical charts. By bringing Ditto Transcripts on board, time’s back on your side to juggle more administrative tasks and care for patients—the work that matters most to you. The way it should be.
For the medical field, Ditto Transcripts delivers:
• Experienced, U.S.-based medical transcriptionists skilled in EHR and EMR systems
• 99% accuracy for all transcription—guaranteed
• Access to speech recognition software editors
• Rapid turnaround and on time for fast access to medical records and reports 24/7
• Electronic file delivery in 24 hours or less
• Speech recognition software editing
• Secure, private, confidential and HIPAA compliant
• Adhere to AHDI/AAMT standards
• Unlimited customer support services
• No long-term contract required
• E-signature/digital signature available
When we say specific, we mean specific. We have deep medical transcription service expertise for cardiology, clinical, dermatology, emergency medicine, hematology/oncology, mental health, neurology, ophthalmology, orthopedic, pathology, podiatry, psychiatry, radiology, urology, among others.
Take us for a test drive. Enjoy 1,000 lines or 60 minutes free. No credit card needed—this trial’s on us. For pricing models and to learn more about our Free Trial, visit us at dittotranscripts.com








PARTNER IN MEDICINE SPOTLIGHT
Whole health, one team: Uniting medicine and dentistry for better patient care
Amisha Singh DDS, EdDl
Although all health care fields share a common goal of improving patient health, individual disciplines such as medicine, dentistry, and behavioral health have traditionally developed in isolation due to differences in education, licensing, reimbursement models, physical infrastructure, and more. As health care professionals, we naturally strive to cultivate our individual professional identities; however, we should always keep in mind that cohesive, coordinated care is invaluable and allows us to elevate patient outcomes and transform the health of communities.
The artificial stop signs that were previously baked into the health care system are disappearing as more schools opt for interprofessional education (IPE) and a curriculum that shows the connection between body systems. Today we stand at the forefront of a transformation that invites everyone across health care disciplines to embrace a more integrated view of our patients, seeing them not as a collection of systems, but as whole, interconnected individuals.
Despite this change in the culture of professional education, it’s unfortunate that many patients still receive dental and medical care in isolation. This disconnect can lead to missed diagnoses, delayed treatment, and fragmented management of chronic conditions. By fostering stronger connections and closer collaboration across disciplines we can create a more patient-centered model of care.
The mouth is not separate from the body; it’s a gateway to systemic health. As dental professionals, we are uniquely positioned to detect early signs of systemic disease and contribute meaningfully to a patient’s overall wellbeing. Yet, the full potential of this contribution is often unrealized due to fragmented care systems and siloed communication between providers.
THE CLINICAL CASE FOR COLLABORATION
The evidence linking oral health to systemic conditions is robust and growing. Periodontal disease, for instance, has
been associated with diabetes, cardiovascular disease, adverse pregnancy outcomes, and even cognitive decline. Systemic diseases can often manifest in the oral cavity first, providing an opportunity for cross-collaboration, referral, and a path to early diagnosis. For example, diabetes can present as slow wound healing intraorally, coupled with conditions such as candidiasis, xerostomia, and/or periodontal inflammation. During my time in clinical practice, I’ve had the responsibility and privilege of helping patients understand that they needed to re-engage with their primary care provider based on oral evaluations.
A patient — we’ll call him Harry — comes to mind. Harry had been living with HIV for more than a decade, but due to recent life changes, he had lost access to regular medical care. He came to our office seeking relief from tooth pain, and during the exam, I noticed a persistent oral ulcer that hadn’t healed. Recognizing it as a potential sign of immunosuppression, I referred him for medical evaluation. That referral ultimately led to the discovery that his viral load had significantly increased, an insight that allowed him to re-engage with care and begin managing his condition more effectively.
The University of Colorado Anschutz Medical Campus, where I was fortunate to have
received my dental education, currently includes interprofessional collaboration as a core part of the curriculum. Early exposure to other medical dependencies has helped me feel confident not only in recognizing when a referral is needed but also in being able to confidently engage with my medical counterparts.
PRACTICAL PATHWAYS TO INTEGRATION
To truly advance whole-person care, we must embrace practical, cross-disciplinary collaboration that breaks down barriers between fields. Continuing a movement to integrate electronic health records (EHR) between dental and medical practices enables real-time data sharing, allowing providers to coordinate care more effectively. For example, when a dentist identifies signs of uncontrolled diabetes, they can alert the patient’s primary care provider (PCP) for a timely evaluation. Routine dental visits also offer opportunities for basic health screenings and appropriate referrals, just as medical providers can flag oral health concerns during physical exams. Embedding dental professionals into primary care settings or bringing medical providers into dental practices through models like patient-centered medical homes or accountable care organizations, has already shown promise in improving outcomes and reducing fragmentation.
THE ROLE OF BENEFITS IN SUPPORTING INTEGRATION
While clinical collaboration is essential, it must be supported by systems that make it feasible. One often-overlooked enabler is the structure of dental benefits plans. At Delta Dental of Colorado, we recognize that benefits design can either support or hinder whole-person care.
Plans that emphasize and cover preventive services robustly, incentivize regular check-ups, and include coverage for medically necessary dental procedures (such as periodontal treatment for patients with special needs) can encourage patients to seek timely care. Moreover, benefits that allow for coordination between dental and medical providers can facilitate the kind of collaboration described above.
When we collaborate, we unlock a deeper potential to heal.
Though benefits design is not the centerpiece of clinical care, it plays a quiet but powerful role in shaping patient behavior and provider engagement. When aligned with clinical goals, it becomes a lever for better health.
LOOKING AHEAD
We have an extraordinary opportunity to reshape the future of health care, not by abandoning our distinct disciplines, but by weaving them together. As health care professionals, we each bring unique expertise to the table. But when we collaborate, when we listen, learn, and lead together, we unlock a deeper potential to heal. The silos that once defined our professions are giving way to bridges built on shared knowledge and a common commitment to our patients. Let’s continue to champion this evolution, not just in policy or education, but in our daily practice and our willingness to reach across disciplinary lines. Together, we can create a health care system that is not only more connected, but more compassionate, more effective, and more human. ■
About Dr. Singh: Amisha Singh, DDS, EdD, is the dental director for Delta Dental of Colorado (DDCO). She has oversight of the daily operations of DDCO’s clinical management functions including dental processing policies, clinical education to DDCO’s provider network, and mission-driven community engagement. She serves on the Colorado Dental Association (CDA) and American Dental Association (ADA) House of Delegates, the ADA Dental Wellbeing Advisory Committee, the ADA National Advisory Committee on Health Literacy in Dentistry, the ADA Women in Leadership Thinktank, and on the ADEA HURM Advisory Group.

1. https://nexusipe.org/informing/ about-national-center/news/ silos-and-timing-ipe
2. https://pmc.ncbi.nlm.nih.gov/articles/ PMC10923120/
3. https://pmc.ncbi.nlm.nih.gov/articles/ PMC6755758/
4. https://www.sciencedirect. com/science/article/pii/ S2319417018302634
5. https://pmc.ncbi.nlm.nih.gov/articles/ PMC3228943/
6. https://www.cuanschutz.edu/centers/ ipe/about-ipe/ipe-at-cu-anschutz
7. https://pmc.ncbi.nlm.nih.gov/articles/ PMC8902175/
8. https://pmc.ncbi.nlm.nih.gov/articles/ PMC4610051/
9. https://pmc.ncbi.nlm.nih.gov/articles/ PMC6618181/
10. https://journalofethics.ama-assn.org/article/ overcoming-historical-separation-between-oral-and-general-health-care-interprofessional/2016-09
11. https://www.kff.org/medicare/ issue-brief/policy-options-for-improving-dental-coverage-for-people-on-medicare/

Nation can learn from Colorado’s progress on prior authorization reform
Bobby Mukkamala, MD President, American Medical Association
Thanks to the persistent and highly effective advocacy work of the Colorado Medical Society (CMS), its partner specialty societies, and a CMS-led coalition of patient stakeholders, Colorado has enacted a prior authorization reform law that takes effect Jan. 1, 2026 that will rein in health plans’ use of this onerous cost-control measure that endangers patients, wastes resources and undermines the expertise of physicians.
The AMA was thrilled to support CMS in this three-year effort. Among the many impactful reforms in the new law, prior authorization approvals will be extended from 180 days to a full year (or the length of treatment), so patients’ continuity of care is protected, and physicians’ time is not wasted on repeat prior authorizations. There will be enhanced transparency of prior authorization requirements and improved prior authorization data reporting to allow for greater plan accountability.
Also, Colorado lawmakers aligned prior authorization automation efforts with those taking place at the federal level, to better streamline the process within the physician’s electronic health record (EHR) and not through the use of multiple portals and logins. And physicians will be able to count on prior authorization approvals for payment, without the fear of retroactive denials.
Achieving meaningful prior authorization reform in the Centennial State – and ensuring that more health care decision-making takes place between patients and physicians – was due in large part to the Health Can’t Wait Colorado campaign coordinated by CMS. This effort to collect firsthand prior authorization experiences from patients and physicians helped convince state lawmakers that real reform was needed now.
RIGHT-SIZING IS AN AMA PRIORITY
As the physician’s powerful ally in patient care, the AMA has been working closely with CMS and our other partners in the Federation of Medicine to streamline and simplify a process that has morphed from a rarely used tool intended to limit the use of expensive, newly introduced medications or treatments into a utilization management strategy that payers regularly invoke before patients can receive even the simplest generic medications or time-proven, evidence-based treatments.
Prior authorization hassles remain a source of endless frustration for me, my small staff and our patients in Flint, Mich. Hassles may be too mild a term. Just a few months ago, a member of my staff had to call an insurer over a prior authorization issue because “Mukkamala” wasn’t coming up as a provider in their system. Even though I have been practicing for a quarter-century, my name failed to appear on physician roster compiled by the largest insurer in my home state of Michigan.
This is an isolated example, to be sure, but also a symptom of an unsustainable process that must be changed. To fully gauge the depth of this problem and the reforms we need, you can see other physicians share some of their very worst experiences with prior authorization at https://tinyurl.com/ama-prior-auth.
Colorado’s new law protects continuity of care and cuts red tape for physicians.

NEW TECHNOLOGY WILL HELP
Electronic prior authorization (ePA) is on the horizon. New policies from the Centers for Medicare and Medicaid Services require health plans to accept, track and return PA decisions electronically, which will cut wait times and paperwork. Colorado physicians are lucky to have a state medical society leading the way in connecting state automation requirements with these new federal rules through state law, to ensure the most streamlined and least burdensome transition.
The AMA is ensuring the physician voice is front and center in ePA development. The goal is for EHR systems to fire off requests and receive instant responses, turning today’s fax-and-phone marathon into a seamless “electronic handshake.”
For medical practices, that future starts with a question: When will my EHR be ePA-ready? Ask your vendor for the upgrade timeline, pilot opportunities, and any training or interface costs. Early engagement lets you shape workflows, prepare staff, and position your practice to reap the efficiencies — and faster patient care — once payers flip the switch in 2027.
The AMA will continue to carefully monitor the implementation of the prior authorization reforms that health plans have pledged to implement nationwide, gauge their impact, and do everything in our power to see that good intentions become concrete reality. Insurers can and should do much more to improve patient care than giving lip service to prior authorization reform. It’s time to follow Colorado’s example and make prior authorization reform a reality nationwide. ■
Hear more from Dr. Mukkamala at the CMS Annual Meeting in Keystone. He will present a session on Saturday, Sept. 20. Register for the meeting on our website, www.cms.org.

COLORADO PHYSICIAN OR MEDICAL STUDENT CALLS 720-810-9131.
24/7 line answered by a Masters-Level Licensed Clinician (LCSW, LPC) to assess the clinical need of the caller, including life-threatening situations.
CONFIDENTIALITY IS REVIEWED AND PEER SUPPORT SERVICES ARE INITIATED.
Only in circumstances where an individual is a threat to self or others or as outlined in the Medical Practice Act would confidentiality be breached. Doc2Doc Wellbeing Consulting has the same reporting obligation as all licensed Colorado physicians.
PHYSICIAN CALLER RECEIVES WELLBEING SUPPORT FROM A PEER PHYSICIAN.
If Doc2Doc Wellbeing Consulting is the best fit based upon the caller’s presentation, a physician will return the physician’s call for the first of three free peer consultations.
If CPHP traditional comprehensive evaluation services are a best fit based upon caller’s presentation OR if more help is needed at the end of three free Doc2Doc Wellbeing Consulting sessions, CPHP’s process will commence to ensure client has appropriate treatment supports in place.