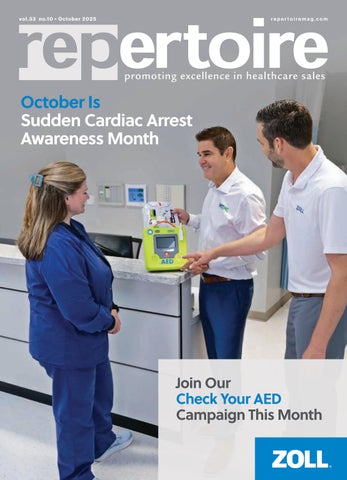
“May I Check Your AED?”
Join ZOLL and MTMC this October as we check as many AEDs and Defibrillators as possible for compliance and readiness. An AED is only reliable if it has in-date pads and ba eries.
ZOLL and MTMC have checked thousands of AEDs over the last five years, and we are looking for your help in 2026. Help us check your customers AEDs. That can make a direct impact on survival outcomes.
Contact your ZOLL or MTMC rep for help transitioning your customer to the ZOLL family.
SCA Awareness Month
Simple questions help get us in the door and could ultimately have lifesaving impact. ZOLL has resources for checking AEDs. Please reach out for our Quick Check Guide, Trade-in Coupon, and list of FDA-approved devices.

Who is ZOLL?
For more than 25 years, ZOLL has designed products that support first responders, medical personnel, and everyday rescuers in times of crisis. Every idea, design and innovation at ZOLL is guided by our singular focus: empowering people to act with confidence and to achieve the best possible outcome for victims. Enable your customers to ‘Grab the ZOLL!’


Who is MTMC?
As a nationwide manufacturer representative group, we work with our trusted partners to deliver a smarter, more efficient buying experience.
MTMC has built trusted connections between medical technology innovators and the healthcare providers who rely on them. With ZOLL we are able to deliver product demos, on-site in-services and product expertise.

Mark Hughes of MTMC and Kyle Pflugner of ZOLL Medical Check a ZOLL AED 3 and R Series for Readiness.
Behind the Scenes
Recognizing the unsung heroes of the U.S. healthcare supply chain.

Behind the Scenes
Scales
Your Teammates in the Field
Leverage manufacturer support to exceed your goals.

As we turn the corner into the fourth quarter, it’s a natural time to reflect on what it takes to finish the year strong. Last month, I wrote about the incredible value distribution salesforces bring to our industry. This month, I want to shine the spotlight on another critical piece of our healthcare supply chain – the manufacturers.
Medical supply manufacturers play a vital role in making sure clinicians, hospitals, surgery centers, and long-term care facilities have the products they need to deliver top-tier patient care. But their value doesn’t stop at production. Manufacturers invest in training, education, and marketing tools designed not only to promote their products but to help you, the distribution rep, be more effective. Those that do this through Repertoire, RepConnect, and the Dail-eNews are the ones who value you most.
Think about how often you rely on a manufacturer rep when closing a deal, answering technical questions, or providing a demonstration that shows exactly how a product improves outcomes. These partners are more than vendors – they’re teammates. As you focus on closing out 2025 strong, leaning on them could be the difference between meeting your number and surpassing it.
Repertoire Magazine is proud to serve as the bridge between you and those partners. The companies that advertise in these pages, sponsor educational modules, and invest in your growth do so because they value you. They see distribution reps as the heartbeat of the healthcare supply chain – connecting innovation to practice. When you see their ads or engage with their training, know they’re putting real dollars behind their commitment to your success.
As year-end approaches, I encourage you to engage with the manufacturers you work with. Bring them into the sales process, ask for their insights, and lean on their expertise. Their product knowledge and willingness to support you in the field can help close tough accounts or strengthen relationships.
Our industry thrives on partnerships. The bond between distributors and manufacturers ensures clinicians have the right products at the right time. Together, you form the strongest link in healthcare’s supply chain.
So, as you push through the fourth quarter (or third for some of you), remember: you don’t have to do it alone. Engage your manufacturer partners. Rely on their support. And let’s finish the year with momentum that carries us into 2026.
Thank you, as always, for the work you do every day.
Dedicated to the industry, R. Scott Adams
editorial staff
editor Graham Garrison ggarrison@sharemovingmedia.com
editor-in-chief, Dail-eNews Jenna Hughes jhughes@sharemovingmedia.com
content creator Pete Mercer pmercer@sharemovingmedia.com
art director Brent Cashman bcashman@sharemovingmedia.com
circulation Laura Gantert lgantert@sharemovingmedia.com
sales executive Aili Casey acasey@sharemovingmedia.com (404) 625-9156
publisher Scott Adams sadams@sharemovingmedia.com (800) 536.5312 x5256
founder Brian Taylor btaylor@sharemovingmedia.com
Subscriptions www.repertoiremag.com/subscribe or (800) 536-5312 x5259
Repertoire is published monthly by Share Moving Media 350 Town Center Ave, Ste 201 Suwanee, GA 30024-6914 Phone: (800) 536-5312, FAX: (770) 709-5432; e-mail: info@sharemovingmedia.com; www.sharemovingmedia.com


What’s Old and New in Lipid Testing
Why it’s time to reignite conversations around lipid tests.
 We have been talking about lipid testing for what seems like a lifetime now. Why on earth are we talking about it again? Sadly, because no matter how much we talk about it and the benefits routine lipid screening have on reducing heart disease, heart disease continues to win.

By Jim Poggi
We have lipid tests, statins and even newer cholesterol drugs, but apparent indifference by a large portion of the U.S. population to practice better health habits is holding back progress. Heart disease remains the number one leading cause of death in the United States, and the latest data published by the National Center for Health Statistics shows an increase in mortality from heart disease from 2019 to 2020.
The tried-and-true lipid assays, used in combination with statins, diet and exercise routine have comprised the routine medical practice for management of lipid levels and are intended to reduce the risk of cardiac events including heart attack and also stroke.

There are good reasons for the use of lipid profile tests and whether your customers are using waived bench top systems or testing for conventional lipid tests (Total cholesterol, HDL cholesterol, LDL cholesterol and triglycerides) on larger non-waived systems, the data is there to support use of these tests. The United States Preventive Task Force assigns an “A” rating to screening in men over 35 years of age and for women over 45 years of age irrespective of known risk factors. They assign a “B” rating for lipid testing for men in the 20-35 age group if they are at increased risk of coronary heart disease and the same rating and recommendation for women in the 20-45 years of age group.
The supporting evidence for lipid testing is overwhelming and includes data and recommendations by CDC, NIH, AMA and multiple well respected teaching hospitals. The MR-FIT study ran from 1972 to 1998 and enrolled over 12,000 participants and proved conclusively that exercise, diet and reduction in cholesterol was associated with a reduction in heart attack and coronary events in general. As additional rationale, elevated lipid levels are directly associated with three of the ten leading causes of death: heart disease, stroke and kidney disease.
In addition, in combination with other factors, lipid levels are also associated with diabetes. In total, they account for diseases associated with 40% of all the leading causes of morbidity and mortality in the U.S. today. Is it any wonder that diagnosis and
and lifestyle or are these opportunities being missed? The best primary care practices today are combining traditional guidelines for lipid measurement with newer recommendations to engage in personalized medicine for patients with additional risk factors. What are these risk factors? Smoking, obesity and uncontrolled blood pressure raise the risk of cardiovascular disease and these are logical patients for more aggressive treatment including more frequent lipid measurements. While smoking has decreased, the other two risk factors have not.
Forty percent of the U.S. adult population is classified as obese and the rate of obesity in children is rising. Furthermore, over 75% of the adults in the U.S. with hypertension are classified as “uncontrolled.” That’s just about 100 million American adults.
Smoking, obesity and uncontrolled blood pressure raise the risk of cardiovascular disease and these are logical patients for more aggressive treatment including more frequent lipid measurements.
treatment of patients with elevated lipids is a major focus for primary care health practices across the U.S.? I am confident that the majority of your customers are prescribing statins and even newer agents including ezetimibe that lowers cholesterol by a different mechanism than statins.
But, are they providing lipid measurements at the point of care where they can provide immediate counseling on diet
What are you and your trusted lab manufacturers doing to create a holistic approach to the control of heart disease risk factors? There are antihypertensive drugs that effectively control hypertension, multiple lipid lowering agents including statins and ezetimibe and the new generation of drugs intended to lower hemoglobin A1c that also assist in weight reduction, GLP-1 agonists. If you haven’t heard one or more
commercials on the television for these agents and do not have an ear wig for the song of one of them, be grateful.
The point is, a holistic program of identifying at-risk patients, using the medications as needed to control their risk factors and providing lipid testing at proper intervals can make a difference in your community and ultimately across the entire U.S. health system.
Have you started your discussions with key customers? Have you engaged in discussions with customers who have benchtop lipid systems but have stopped using them? It’s worth your time to develop a program with your key lab manufacturers and present it to your most forward-thinking customers as a thoughtful and trusted consultant. They know this information but many of even the best practices are not engaging in a systematic approach to controlling cardiovascular risk. Many others are not using the tools they have at hand.
If you carefully research your key customer base, unfortunately, you should find plenty of prospects. In my experience, there are many waived bench top systems in place but not being used. A simple discussion centered around the current approach to testing for lipids and a thoughtful discussion around the rationale to test should get a productive conversation going.
For example, “I was recently reading about the incidence of cardiac risk factors as well as the United States Preventive Services Task Force lipid testing recommendations, and I learned a lot. May I share a few facts with you?”
That’s not a bad ice breaker, but, working with your trusted lab manufacturers, I am sure you can customize your initial statement to be interesting and provocative. You will need a sound attention getter to open the conversation.
My assessment is that many of the practices that have stopped in-office lipid testing got exhausted and frustrated when they did not see patient progress. Some may be convincible if you can get them excited again. I would specifically ask if they suspended testing due to lack of patient progress. Check with your key lab manufacturer to see if they have patient education information to supplement counseling by the practice. This extra help may be the incentive they need to give in-office lipid testing another try.
What, exactly, are these old but new to many of us lipoproteins? First, they have been around in the literature since the 1990s and have gained adherents in Europe. Both complement Cholesterol, HDL and LDL. Lipoprotein (a) (Lp(a) is a variant of LDL cholesterol. Elevated levels of Lp(a) are associated with increased risk of cardiovascular disease.
In addition to the typical lipids we measure, Lp(a) is considered an independent risk factor for cardiovascular disease. Lp(a) is known to be responsible for the formation of arterial atherosclerotic plaques. ApoB is a name given to an assortment of lipoproteins including very low-density lipoprotein and lowdensity lipoprotein, also known as LDL. ApoB is the lipoprotein that actually makes up the structure of
A simple discussion centered around the current approach to testing for lipids and a thoughtful discussion around the rationale to test should get a productive conversation going.
What’s old but under used?
While “new” lipid tests have been around for over 30 years and have significant supporting evidence, the use of assays for Lp(a) and ApoB have been exceptionally slow to catch on in the United States. However, the combination of personalized health initiatives, new medications which target lowering LDL specifically and the rapidly increasing use of GLP-1 agonists point to a change in lipid profiling.
plaques. So Lp(a) and ApoB are independent entities and each has a role to play in the development of atherosclerosis.
Although few lab companies today offer these assays, making it unlikely that your customers are asking you for them, why am I mentioning them? Because they are important to know in the overall story of lipid testing and lipid medications.
Despite the fact that these two assays are rarely performed,
ID NOW™ PLATFORM
ONE SWAB THREE RESULTS
THE ID NOW™ PLATFORM GIVES CLINICIANS THE FLEXIBILITY TO TEST FOR COVID-19 AND EASILY ADD ON FLU A & B BASED ON CLINICAL NECESSITYWITHOUT THE NEED FOR COLLECTING AN ADDITIONAL SWAB.*
With the ID NOW™ Platform, the clinicians have the power to decide which tests to run based on patient presentation, circulating prevalence and seasonality. By reducing unnecessary testing, clinicians can save time and resources, allowing for rapid diagnosis and improved patient workflow.

the good news is that some are coming to market. Will they become mainstream assays? Probably not. It is more likely that they will be used selectively in patients with poor responses to conventional lipid lowering agents or those with a family history suggesting abnormal lipid metabolism.
There are several CPT codes listed in the Clinical Lab Fee Schedule, with the most pertinent being 83695, “Lipoprotein A level”. It is a national CPT code, and it pays $14.32. Some manufacturers are beginning to develop and commercialize these assays and your best bet for more information is to touch base with your trusted lab manufacturers that offer non-waived assays and ask them for more information.
What makes sense to do?
If I had a territory, I would check in with a cross section of my customers with waived bench top systems that either are not used at all or have limited use. Your sales reports should easily provide you with this information.
As always, start with the questions:
` “What caused you to acquire this system?”
` “How has it performed for you?”
` “I see you are not using it. Can you tell me why?”
With that information, I would make sure their practice demographic is similar to when they acquired the system and I would suggest: “I can bring in an expert on this system who can address your concerns and help
Your specific job with this customer group is to learn what caused them to become discouraged (that’s why they stopped testing in-house) and to bring that excitement and confidence that they can make a difference with this patient group back.
From my perspective, it is difficult to predict the future of these assays. Unless there is a drug that comes along specifically targeted to them, I believe they are likely to be confined to IDN core labs and reference labs. But stranger things have happened, and it is worth your time to check in with a manufacturer or two of large non-waived chemistry systems to get their take on these assays and their future.
make this system productive for you and your patients. May we make an appointment for this discussion? If we can find ways to address and resolve these issues, would you consider re-instituting testing on it?”
If they say no, ask why and if you cannot address their concerns effectively, move on and think about finding a different way to address their issues at another time.
If they say yes, make sure you ask to have customer technical personnel and decision makers in the meeting.
And ask for a range of dates. Work out the best date with your lab manufacturer and firm up the date as soon as possible. It is in the interests of your customer, their patients, you and your lab manufacturer to make sure that lipid testing becomes a routine part of their daily work as soon as possible. Your job with these customers is for them to become excited again and to feel that they can make a difference. Any new manufacturer support literature will be helpful here.
We all experience headwinds in our territories. How we address them determines our success and the value we bring to our customers and the importance they associate to their relationship with us. Re-activating a system that once seemed to have value but has fallen out of use is a strong way to help establish the concern you have for your customer and their success. Your specific job with this customer group is to learn what caused them to become discouraged (that’s why they stopped testing in-house) and to bring that excitement and confidence that they can make a difference with this patient group back.
Essentially, you will act as a cheer leader. While this column discussed how to work to reestablish lipid testing, the principles we have discussed apply far more broadly. Use them successfully and you will earn your customers’ respect.



The Rise of the Double Threat Rep
Why the ones who show up and follow up are winning.
By Brian Sullivan
 We’ve spent the last five years automating everything. Emails? Automated. Sequences? Scheduled. Follow-ups? Scripted, tracked, color-coded and blessed by AI.
But here’s the thing nobody wants to say out loud: while your competition is perfecting their sixth-step email cadence, someone else just walked into the building and booked the deal.
That’s the rise of the Double Threat Rep – someone who knows when to click and when to knock. And in 2025? That rep is getting the meetings faster, gathering the intel earlier and closing the deals you thought were “going dark.”
Being present
Let me say this right up front: this is not a knock on inside sales. Some of the most productive reps I know never leave their desk, and my own 15 cold calling SDRs at PRECISE prove daily that you can book pipeline from a laptop with the right coaching and conviction.
But this article is for the rep who has access to the field and has stopped using it.
Maybe you think it’s too crowded. Maybe you haven’t been trained to drop in without a meeting. Or maybe no one told you the truth: In-person isn’t dead. It’s just underused.
And that’s your edge.
Field gravity still closes deals
Double Threat Reps understand you don’t need a scheduled meeting to matter. Sometimes, just showing up – intentionally, respectfully, and consistently –puts you back on the radar.
That nurse you used to bump into near the elevator? She’s now the one whispering in the decisionmaker’s ear. That purchasing manager who always said no? They’ve retired, and you’d only know if you walked past the front desk and asked.
You don’t learn that over Zoom.
You learn it when you’re there.
That’s field gravity. The more you’re seen, the more you’re trusted. And the more you’re trusted, the faster things move.
What makes a rep a “double threat”?
Being a Double Threat Rep doesn’t mean you’re on the road 24/7. It means you’re dangerous because you know how to move between the inbox and the front desk without missing a beat.
Here’s what they do differently:
` They prep using CRM data, then show up in person to fill the context gaps
` They follow up digitally after an in-person interaction, so they’re remembered twice
` They walk the halls with purpose, not just presence
` They bring something that makes the prospect smarter or happier – a relevant article, a quick case study, a branded Sharpie, or just a solid idea that helps solve a real problem
` They combine value with visibility – and they get deals moving because of it
It’s not about being everywhere. It’s about being intentional, memorable, and worth talking to – online and off.
From invisible to in-demand
One of the reps I worked with –we’ll call her Alex – was hitting every number except revenue. Her activities looked great. Her call notes were beautiful. Her sequences were on-brand. The problem? Nobody in her territory remembered her name. We made one change. She started time-blocking field time into every day – even just an hour. Her calendar now had set blocks for planning, phone prospecting, admin, and purposeful visits. Not random pop-ins. Each stop was intentional: bringing something useful, solving a problem, or sharing an insight that made the customer smarter – or happier.
By week three, people were calling her.
By week five, her win rate started climbing.
And by month two? She was the name they remembered.
That’s Double Threat selling.
What if you don’t have field access?
Double Threat isn’t about geography – it’s about awareness.
Even if your role is fully remote, you can still:
In a world of noise, sameness, and templated outreach, the most dangerous thing you can be is … memorable.
Want to be one?
Try this weekly rhythm
Here’s a practical cadence that balances screen time with street time:
` Monday: Review accounts and flag ones with recent digital touches but no physical follow-up
` Tuesday/Wednesday: Stack meetings and schedule smart visits before or after each one
` Thursday: Pick a hospital café or clinic lobby and work there for 90 minutes – yes, with your laptop
` Friday: Follow up on in-person conversations with short, personalized emails or voicemails
“Great chatting near imaging – following up with what we discussed…”
Do it consistently, and you’ll stop being the rep who “pops in once a quarter,” and become the one they expect to hear from.
` Call a staff member directly instead of always emailing
` Ask a local team member to hand-deliver a piece for you
` Send a video referencing something hyper-local
` Set up a Zoom with a gatekeeper – not to pitch, but just to make their day
It’s not just about being in the building. It’s about being top-of-mind.
Be the rep they remember
In a world of noise, sameness, and templated outreach, the most dangerous thing you can be is … memorable.
And here’s the truth: CRMs don’t close deals. Connections do. Double Threat Reps know this. They click when it makes sense. They call when it counts. And when it’s time to get the meeting, they walk in, smile and say: “Thought of you. Got something I think you’ll want to see.”
Brian Sullivan, CSP, is the Founder of PRECISE Selling and a leading voice in B2B sales strategy. He helps companies master the art of prospecting, presenting, and negotiating – while also building elite outsourced sales teams through his PRECISE Performers division. A nationally recognized speaker and author of 20 Days to the Top, Brian’s mission is simple: turn salespeople into champions. Learn more at www.preciseselling.com
The Power of Partnerships

Jack Moran of MTMC receives 25 year partnership award from ZOLL's Jonathan Bowman.

In the competitive world of medical sales, few partnerships have had the staying power – or the impact – of ZOLL and MTMC. Their 25-year collaboration began with a bold idea: bringing defibrillators into non-acute care settings like physician offices. At the time, AEDs were rarely used outside hospitals, making education and market adoption a major hurdle. But that shared challenge became the foundation for a lasting, results-driven alliance.
On a recent Repertoire podcast, Scott Adams spoke with Jonathan Bowman of ZOLL and Jack Moran of MTMC about the origins of their partnership and what’s fueled its longevity. It all started when James Saltzman approached MTMC to represent ZOLL AEDs in the primary care market. As care delivery shifted to urgent care centers, freestanding ERs, and outpatient surgery centers, ZOLL and MTMC evolved their strategy, launching a successful cold-calling campaign to target these new sites.
Regulatory changes, like the FDA’s move to pre-market approval (PMA) for defibrillators, added new challenges –and opportunities. Through it all, ZOLL remained committed to its distribution model. “This is a very competitive space, but ZOLL has never wavered in their commitment to us or to distribution,” said Moran. “That consistency has been key.”
Equally important has been stable leadership. In 25 years, MTMC has worked with just two leaders at ZOLL: Saltzman and Bowman.

“We’ve never had to reeducate a new team,” said Moran. “That continuity helps us move faster and stay aligned.”
Bowman credited ZOLL’s adoption of the 95% Share Marketing training introduced in the early 2000s as another driver of success. ZOLL embedded the training into its culture and extended it to MTMC reps, reinforcing shared values and sales discipline.
Two pivotal moments shaped their recent growth: First, after COVID, the FDA’s AED policy shift prompted ZOLL and MTMC to launch the “Check Your AED” campaign. Reps visited facilities to inspect aging AEDs, creating new business while offering value to customers. Second, after NFL player Damar Hamlin’s life was saved by a ZOLL device, national awareness of AEDs surged, boosting demand and visibility.
Leveraging a Powerful Partnership
Bowman and Moran also shared insights for today’s reps. Moran urged reps to open conversations with questions like, “How old is your AED?” He stressed confidence in representing ZOLL, especially as corporate buyers dominate purchasing.
Bowman advised reps to treat MTMC as allies, not competitors, and warned against “quote and hope” selling. Face-to-face demos build trust and often lead to larger deals – like one that started with a distributor call and ended with a 50-location group order. “When we demo, we win,” he said.

Scan the QR Code to listen to the podcast.
Leading a Customer Service Revolution
John DiJulius on elevating experience in 2025.
By Pete Mercer
 If you were to purchase something from your company, are you certain that you would be satisfied with the whole experience? From the first interaction to the final purchase, every touchpoint that your customers engage with in the purchasing journey is part of the whole customer experience –and that experience matters.
Repertoire Magazine sat down with John DiJulius, chief revolution officer of The DiJulius Group, to discuss the state of the customer experience in 2025. As an employee and customer experience consulting firm, The DiJulius Group’s mission is to change the world by creating a customer service revolution.
From the salon to the stage DiJulius and his wife opened a salon in Ohio in 1993, where he began to stretch his customer service muscles. Because of the customer service reputation they had built, people started asking DiJulius to come and speak at events.
“I thought it would be a good marketing opportunity, but I didn’t think it was ever going to turn into a career,” he said. “But every time I spoke, two or three business leaders would come up and ask me to speak to their company. By 2003, I released my first book, which took me from being a salon owner that spoke a little bit to a speaker that owns salons.”
From there, The DiJulius Group has worked with clients

like Chick-fil-a, Starbucks, Nestlé, Marriott, and Lexus. With brands like this, you would be forgiven for assuming there’s a strategic

approach to these partnerships, but DiJulius says that he’s never done outreach.
All their partnerships are formed based on the client being familiar with his work – by seeing him speak or reading one of his books – and reaching out to start a conversation with him. Because of his experience owning and operating a successful chain of salons in Ohio, DiJulius has been able to build a customer experience methodology that speaks for itself.
Building a methodology
Part of what sets DiJulius’ approach apart from others in his field is his methodology, The
John DiJulius
Cepheid’s high-performing molecular test, Xpert® Xpress CoV-2 plus, with up to 99% PPA leaves no room for doubt.
Experience diagnostic confidence Visit cepheid.com
Cepheid’s high-performing molecular test, Xpert® Xpress CoV-2 plus, with up to 99% PPA leaves no room for doubt.
© 2025 Cepheid. IVD. In Vitro Diagnostic Medical Device. May not be available in all countries.
*Smith-Jeffcoat SE, Mellis AM, Grijalva CG, et al. SARS-CoV-2 Viral Shedding and R apid Antigen Test Performance — Respiratory Virus Transmission Network, November 2022–May 2023. MMWR Morb Mortal Wkly Rep 2024;73:365–371. DOI: http://dx.doi.org/10.15585/mmwr.mm7316a2 ^ Xpert Xpress CoV-2 plus is 99.3% for anterior nasal swab specimen for PPA

© 2025 Cepheid. IVD. In Vitro
*Smith-Jeffcoat SE, Mellis AM, Grijalva CG, et al. SARS-CoV-2 Viral Shedding and R apid Antigen Test Performance —
Virus Transmission Network, November 2022–May 2023. MMWR Morb Mortal Wkly Rep 2024;73:365–371. DOI: http://dx.doi.org/10.15585/mmwr.mm7316a2 ^ Xpert Xpress CoV-2 plus is 99.3%
X-Commandment Methodology. This is a ten-step process that takes a deeper look at how brands and companies can elevate their approach to the customer and employee experience. This is an overview of what DiJulius’ framework looks like:
1 Igniting the CX revolution –This is where you get a better idea of your company’s customer experience and develop a strategy to improve engagement at each touchpoint.
2 Creating your signature experiences – Part of what sets you apart from your competition is a unique and memorable experience, which will turn your customers into your advocates.
3 Zero risk – A zero-risk approach identifies and removes the biggest risk factors in what you offer, allowing you to put your best foot forward.
4 Creating an above-andbeyond culture – In an above-andbeyond culture, your team should be empowered and equipped to exceed customer expectations.
5 Recruiting experience –You need an all-star team, so it’s important to find and attract the top talent to take care of the customer experience at your company.
6 Onboarding experience –Once you have hired the all-star team, it’s time to set them up for success with an excellent onboarding experience.
7 Employee experience –To create a positive employee experience, it’s important to create a work environment where they feel valued.
8 Tearing down silos by building collaboration across departments – By removing silos and
encouraging collaboration, you will build a company culture that promotes teamwork.
9 Building and developing leaders – Everything falls on the leadership, so it’s important to cultivate strong and compassionate leaders who are looking to achieve more.
10 Training and implementation – Ensure that your teams have the resources and tools that they need through a consistent training process.
This framework was built while DiJulius and his wife were primarily focused on providing an excellent experience in the hair salon. Their goal was to create the best experience of the customer’s day – not just the best hair salon. Most people go a couple of months without getting a haircut, so it was important to create an experience that would stand out from the rest of the day.
“Even if we were the best in the salon industry, it’s irrelevant. You’re not going to our competitor unless we do something really horrible. We wanted to be the best experience compared to the rest of your daily routine. Ideally, you’d walk into the doctor’s office and say something like, ‘Why don’t they greet me like they did at the hair salon?’”
As DiJulius continued to work out a solution, he started to study world-class companies. After he started working with some of these companies, it helped him to develop his own methodology based on what had worked for them. The X-Commandment Methodology was built from things that all these world-class companies – Chick-fil-A, Starbucks, Marriott,
etc. – offered as a signature experience for their customers.
The modern-day customer experience
Defining the customer experience in 2025 can be challenging. While we have all these tools at our disposal to improve efficiency and optimize the experience, customer service is suffering as a whole. DiJulius said, “We have been in a customer service recession for five years now. Customer service is at an all-time low according to the American Customer Satisfaction Index, which measures every industry.”
DiJulius described how ‘experience gaps’, wherein there is a disparity between what the customer expects from a brand and what they actually experience, contribute to the customer service recession. Between things like shrinkflation (fewer Doritos in the bag than there used to be) or tipflation (increase in tip requests at point-of-sale, specifically where there were none before), being a consumer is becoming more challenging than it used to be. Prices have increased, but that doesn’t mean that quality improves as well. Finding ways to navigate those experience gaps is really where companies are going to shine the brightest, especially when they make a mistake. DiJulius described a concept called the service recovery paradox: when something goes wrong, your team takes that extra step to fix it. The idea is that if you send the wrong order to someone, you would then overcorrect by doing something like sending an extra case for the inconvenience. This is an opportunity to be a hero when you drop the ball.



























Behind the Scenes
Recognizing the unsung heroes of the U.S. healthcare supply chain.
When we think of healthcare heroes, our minds often turn to physicians, nurses, and the caregivers on the frontlines of patient care. And rightfully so. But behind every successful surgery, every stocked hospital shelf, and every life-saving treatment delivered on time, there is another group of heroes working tirelessly – often unnoticed.
These are the professionals who keep America’s healthcare supply chain moving.
From navigating global trade regulations to ensuring trucks roll out ahead of a hurricane, to building resilient systems that deliver millions of critical products every year, their work is essential to keeping patients safe and care uninterrupted. They are problem solvers, innovators, and leaders who thrive in the background but whose impact is felt in every hospital, clinic, and exam room across the country.
In the October and November issues of Repertoire Magazine, we will highlight several of those unsung heroes whose expertise, resilience, and passion ensure that healthcare never skips a beat.
Caring for Others, and Each Other
How two Wilburn Medical Supply team members turned adversity into impact.
Behind every smooth-running supply chain are people whose dedication and skill keep essential products moving where they’re needed most. At Wilburn Medical Supply, employees like Maria Mabe and Todd Aitken exemplify that commitment, serving customers with unwavering focus even while facing their own personal health battles. Their determination ensured that hospitals, clinics, and physician offices had the critical supplies to care for patients, proving that for them, this work is not just a job, but a mission to support the medical community and save lives.

Maria Mabe has been with Wilburn Medical as Purchasing Manager/Accounts Payable and Customer Service for nearly five and a half years.
“I stay busy all day every day,” said Mabe. “I’m on the phone with customers and vendors, entering purchase orders, entering bills to be paid and processing sales orders.”
Todd Aitken, Customer Specialist & Key Product Manager, has been with Wilburn Medical for more than five years.
“I have a base of customers to support and also work as product manager for a couple of products,” said Aitken. “Each day, I may be helping my current customers get the supplies they need or working to help bring a product to the attention of a market we can serve.”
Both Mabe and Aitken describe their roles at Wilburn Medical as being more than jobs, but a way to support patients, physicians and the medical community by providing them with critical medical products.
“I feel like what we do really makes a difference in the world by supplying medical professionals the tests and equipment they need to improve patient health and, in some cases, saves lives,” said Mabe.
“Being a part of our team allows us to positively impact lives both through the products we distribute, and through our ‘Wilburn Cares’ program, which gives back to great programs both locally
Better Health Better Future




and across the world that help people who need help the most,” said Aitken.
Life changes
Life can change in an instant, yet personal resilience, reinforced by daily routines, can provide the
strength to face both personal and professional challenges.
In February 2022, Mabe scheduled a routine mammogram. A 0.5cm lump was discovered, biopsied, and found to be cancer.
“I scheduled a mammogram partly because of a survivor who
“ I made sure to keep a positive attitude through both treatment journeys and I am proud that I did not give up. I found strength within myself I did not know that I had. I am continually facing big fears by getting all my health screenings on time.”

spoke at work a few months before my diagnosis, and to satisfy my doctor at an upcoming physical,” said Mabe. “I then met my medical team, and we decided to move forward with a lumpectomy and 20 treatments of radiation.”
Just months later, in March 2023, Mabe went for her first post-cancer mammogram, and two larger lumps were found in the same breast.
“I had felt them and was not surprised; however, I thought they were probably some sort of scar tissue,” said Mabe. “Once again, the spots were biopsied and came back as cancer. My surgeon and I immediately decided that I would have a mastectomy, so surgery was scheduled.”
Thankfully, the margins came back clear after Mabe’s mastectomy, so she did not have to go through any additional treatments. Throughout her entire diagnosis and treatment, Mabe continued to work at her job at Wilburn Medical.
“I could not just shut down; I am not made that way,” said Mabe. “I needed as much normalcy as possible and that meant returning to work as soon as possible. I was out for three days with my lumpectomy and only two weeks with my mastectomy.”
Mabe courageously managed the balance between treatment, recovery and responsibilities at work, often scheduling her radiation treatments after work hours.
“I brought food every day and worked through lunch, so I did not miss as much time at work,” said Mabe. “Everyone at work was very understanding and offered assistance any way they could.”
Despite being more tired than normal due to the radiation
treatments, Mabe says she overcame physical, emotional, and professional challenges by taking the journey of treatment and healing one step at a time.
“In the very beginning I struggled emotionally, but I realized very quickly that I could not give up,” said Mabe. “I focused myself on trusting that God had given me the exact medical team that I needed.”
Overcoming fear
In late 2020, Aitken had been feeling exhausted and sick. His wife and coworkers encouraged him to go to his family doctor’s office to get checked out.
From there, he was referred to a specialist, who ordered a CT scan. The CT scan found that Aitken had a large renal (kidney) mass, consistent with renal cell carcinoma.
“I went to a restaurant immediately after the CT scan and had just started eating lunch when my phone alerted me to read my diagnosis,” said Aitken. “A doctor called withing minutes to recommend I have surgery.”
Aitken’s wife, who also works in the medical field, was integral in his process of diagnosis and treatment, immediately calling on her connections and contacts in the industry for guidance.
Shortly after his diagnosis, Aitken received a call from a highly recommended surgeon’s office to schedule surgery to remove the tumor.
“There was a very brief period where fear was a problem, mostly pre-diagnosis when I knew something was seriously wrong and the symptoms and test results looked like cancer, and immediately after diagnosis when google searches showed

“ My Wilburn family, friends and my family were so supportive and positive through both of my battles. They immediately came together as a group and had prayer with me, gave me hugs and well wishes. They loved me through the entire process of treatment and diagnosis.”
a 17% survival rate (never trust internet searches),” said Aitken. “The fear then turned inside out, and I felt like I was prepared to deal with whatever pain was involved. I was excited and thankful for the surgery to have
the tumor removed and had the realization that cancer feeds on fear and I was not going to participate in fueling it.”
Even while navigating treatment, Aitken also continued to work at Wilburn Medical, drawing
strength from routine and the support of colleagues.
“Other than taking a few weeks off to recover from surgery after removing my kidney, I never felt that I was physically unable to do most of the things that I normally do,” said Aitken. “The management team at Wilburn Medical was very
supportive. They made it very clear that treatment and recovery should be my number one concern and continue to help me work around my appointments.”
The power of support
To get through the difficult process of cancer treatment, Mabe

and Aitken relied on their faith, family, friends, and coworkers.
“First and foremost, I relied on God through prayer,” said Mabe. “My Wilburn family, friends and my family were so supportive and positive through both of my battles. They immediately came together as a group and had prayer with me, gave me hugs and well wishes. They loved me through the entire process of treatment and diagnosis.”
“My family was incredibly supportive and encouraging,” said Aitken. “To see God move these people to do what they did was amazing and any fear and uncertainty about the future disappeared quickly.”
Mabe’s coworkers ensured they would help her in every way possible by pooling money and sharing it with her when she was going back and forth to radiation treatments to help her with the cost of gas.
While Aitken was preparing for and recovering from surgery, his friends, coworkers, neighbors, and church members surrounded him in prayer, arranged prayer services for his well-being, cooked homemade meals, did household repairs, and provided his family with gift cards to purchase any food they needed.
“On the day I was diagnosed, I called work to let them know the results. I immediately received a call back from Rick Wilburn who was already in his car driving to find me wherever I was, just to give me a hug and encouragement,” said Aitken.
“When I went to work the day after my initial appointment at the surgeon, Rick Wilburn
popped out of a meeting and grabbed me in the hallway and said, ‘Don’t worry about this, we’ve got you,’” said Aitken. “A few minutes later, he called me into his office to explain that my job was secure regardless of the length of my absence.”
Before his diagnosis, Aitken’s coworker Maria had also noticed that he looked and seemed unwell and was persistent in encouraging him to seek medical attention.
“Between Maria and my wife, I was being told day and night to see a doctor, and I’m so grateful that I did and before it was too late,” said Aitken.
Moving forward
Facing cancer is never easy, but the unwavering support of loved ones and colleagues can make all the difference.
Mabe says she is most proud of maintaining a positive attitude throughout her cancer treatment and recovery. She stayed determined to face each challenge with resilience and optimism.
“I made sure to keep a positive attitude through both treatment journeys and I am proud that I did not give up,” said Mabe. “I found strength within myself I did not know that I had. I am continually facing big fears by getting all my health screenings on time.”
ULTRASOUND & IMAGING TABLES
Looking back, Aitken also reflects on his own diagnosis, saying he has no pride in the way he handled the diagnosis and surgery.
“I never really looked at my diagnosis as ‘life-changing,’ at least not in a negative way,” said Aitken. “I felt so blessed to have so many people reaching out to support me and wanted them to know that I was going to be okay.”
“I’m just thankful that I got a little peek behind the curtain to see how God operates. It is amazing to see His work through family, friends, co-workers, doctors and others,” said Aitken. “I feel like I am just along for the ride on this journey of life.”



Cavo Side Chair
From Expediter to Strategist
Heather Kolenik’s 30-year journey at Henry Schein.
When people think of healthcare, they often picture doctors, nurses, and frontline caregivers. But behind every patient interaction is an unseen network of supply chain professionals ensuring critical products are there when they’re needed most. For Heather Kolenik, Senior Manager of Inventory Management and Large Customer Supply Strategy at Henry Schein, that behind-thescenes work is her passion – and her purpose.
Kolenik’s journey began 30 years ago, when she joined Henry Schein as an expediter on the Inventory Management team. At the time, healthcare largely centered on supporting small-office practitioners. “I’ve held many roles within Inventory Management over the years, and as the industry shifted from small-office practitioners to the IDN space, I recognized the critical need for strategic support – one that my background uniquely positioned me to fulfill,” she said. Today, Kolenik leads the strategy that ensures Henry Schein delivers optimal fill rates for large customers. Her days are anything but typical. One moment, she’s collaborating with sales teams to understand unique inventory demands. The next, she’s preparing inventory levels for a major customer implementation, or analyzing opportunities to improve fill rates for critical accounts. Kolenik balances the technical with the human, never losing sight of the

weather conditions, and unforeseen crises can disrupt supply in an instant. Preventing those disruptions demands a 24/7 commitment, with teams working tirelessly to safeguard the flow of critical products. COVID-19 revealed the fragility of these systems to the broader healthcare community, but for Kolenik, it only reinforced the importance of proactive planning and collaboration.
At the heart of her leadership philosophy is teamwork. To
“ Creative, outside-the-box thinking is crucial so the team can develop innovative solutions that drive the best results for our customers.”
patients who depend on the products her team helps deliver.
That connection to patient care became crystal clear during Hurricane Helene. The storm’s devastation severely disrupted the national supply of IV solutions – a resource many patients rely on for survival. “Our team responded quickly, delivering critical products to affected areas and partnering closely with our largest customers to ensure uninterrupted access for patients relying on these life-sustaining treatments,” she said.
Moments like these underscore the critical importance of supply chain professionals in healthcare. Kolenik is quick to point out that global events,
Heather, successful supply chain operations hinge on strong interdepartmental partnerships. “In a large organization, effective coordination across teams is crucial to delivering optimal solutions for our customer base,” Kolenik said. “In this role, it is imperative that we make sure we fully understand every issue before acting. Creative, outside-the-box thinking is crucial so the team can develop innovative solutions that drive the best results for our customers.”
Ultimately, the greatest challenges arise from the unknown. “By fostering open communication with our customers, we can anticipate their needs and implement solutions that reliably meet them.”
Heather Kolenik





Winter can be full of fun and games
Until you get hit with a respiratory infection. Accurately diagnosing our friends Flora, Spike, Sniff and Streppy here can be a challenge as clinical symptoms overlap, which is why rapid tests have many advantages. Getting the correct diagnosis and treatment to patients in minutes lets them get back to the fun.
Save money with our unique QC Inside® feature; two extra tests for external QC at no charge.
Be prepared with the OSOM® Flu SARS-CoV-2 Combo, OSOM® COVID-19 Antigen, OSOM® Ultra Plus Flu A&B and OSOM® Strep A Tests.


Sniff
Streppy
Spike
Flora
Behind the Scenes of Healthcare Delivery
How
Eric Robinson and CME Corp. keep the system moving.
By Pete Mercer
In the world of healthcare, patients and providers rely on medical equipment to be where it needs to be – functioning, installed, and ready to save lives. But behind every delivery is an intricate web of planning, coordination, and execution that often goes unnoticed.
At the center of CME Corp.’s delivery service is Eric Robinson, Executive Vice President of Operations. With more than three decades at the company, Robinson has helped transform CME from a 12-person operation into a national logistics powerhouse with over 350 employees. In this interview with Repertoire Magazine , Robinson shares insights into the complexity of healthcare equipment distribution, the challenges of navigating evolving industry demands, and the importance of building teams that can deliver – literally – on the company’s promises.
Navigating industry shifts
Over his 32-year career with CME, Robinson has seen the size and scope of the industry change right before his eyes. Through the years, CME has grown from an operation with 12 employees to a well-oiled machine that employs more than 350 people across the country. He said, “The sheer size
of the business has changed, and technology has changed in a way that now enables us to do things that we never would have dreamed of in the past, like providing visibility for product movement and allowing us to forecast.”

CME operates as a fullservice solution that supplies the healthcare equipment their customers need, as well as turnkey delivery service and biomedical service that provides support after the healthcare equipment has been installed.
“One of our big value propositions is that we offer delivery and installation services for the equipment that we sell,” Robinson said. “As an equipment
distributor, we source equipment from a variety of manufacturers and as a value-add service, we can aggregate the product at our warehouses across the country until delivery. From there, we work with the customer to schedule the delivery and installation of that product.”
Robinson said that ‘dance,’ of coordinating all those functions, is the most challenging part of the job. It’s all about timing the shipment of the product to CME’s staging facilities at the right time so it is available for delivery when the customer needs it, while mitigating the added cost of long-term storage. That process is one of those invisible aspects of the healthcare supply chain that Robinson wished more people could see.
He said, “I just don’t know if everyone understands everything that goes into delivering healthcare equipment. It begins with account managers acutely understanding the needs of their customers and recommending the best equipment for needs and budget, to preparing the quote and receiving a purchase order, scheduling receipt of the product(s) to the CME warehouse, managing the logistics of warehousing and staging, and finally delivering and installing the equipment
Eric Robinson
to its service location, when it is convenient for the customer.
Healthcare equipment acquisition is a finely tuned, overarching process that is dependent on multiple departments continuously communicating and flexibly coordinating with each other so at the end of the day the customer can deliver care to their patients without interruption.”
During the pandemic, Robinson and his team at CME navigated the greater supply chain disruptions that were creating problems for industries across the board. Thanks to a good bit of creativity and their resources as a distributor, they were able to meet the needs of their customers. These days, tariffs are creating uncertainty around budgetary issues for everyone, which means that many of CME’s customers are ordering larger quantities of equipment to avoid future tariff impacted purchases. This is a new thing for Robinson and his team, so they’ve developed a plan that allows customers to lock in their budgets by placing orders now for delivery of healthcare equipment in the future.
“That’s created the challenge of developing solutions to procure and store the equipment for them,” he said. “Because we aren’t a bank, we have developed a mutually advantageous fee for storage service that answers the customer’s need to order and store quantities of equipment as well as covers the associated expenses. The dynamic nature of the healthcare industry forces us to evolve the service options we’re offering our customers, and refine the discussion points we have with them.”
Building effective teams
For Robinson, an effective team is the foundation of CME’s success and the fulfilling career that he’s had at CME. Three directors report directly to Robinson, managing the departments that he oversees – Dan Chevrette, Director, Service Solutions; Kelli Bugbee, Corporate Director, Customer Service & Purchasing; and Wade Oliveira, Corporate Director, Distribution Operations. In addition to managing their departments, these directors work directly with the project managers who are responsible for communicating with customers
customers, the installation teams can spend days and occasionally weeks away from families, especially on large installation projects.
During the interview, Robinson talked about a recent project in the Rio Grande Valley, the very southern tip of Texas. This is an eight-hour trek from the nearest warehouse, which meant that there was a rotation of half a dozen team members routinely making visits to that site for more than a month. Additionally, they’re working in the Texas heat in July, which can further complicate a job like this. While the work isn’t easy,
The installation teams operate out of more than 25 warehouses scattered throughout the country, receiving, preparing, and delivering the products that CME sells to its customers. In order to fully service these customers, the installation teams can spend days and occasionally weeks away from families, especially on large installation projects.
to coordinate the delivery of medical products into CME’s warehouses and scheduling delivery of the medical equipment to the customer around staff and patient needs.
According to Robinson, the project managers and installation teams are the ones who often go unnoticed. The installation teams operate out of more than 25 warehouses scattered throughout the country, receiving, preparing, and delivering the products that CME sells to its customers. In order to fully service these
Robinson says that his team understands the vital role they play in the overall customer experience.
“Those team members are the last people our customers see, so they have a lot riding on their shoulders – and they come through with shining colors,” he said. “I admire those guys and gals for being able to do what they do. It is because of them and the people behind the scenes working in tandem with one another that our delivery and installation value proposition has been so successful.”
Meet the Leaders Driving Cardinal Health’s Supply Chain Success
Whether it’s ensuring a critical medical product arrives in time, navigating the ever-evolving landscape of global trade or running a distribution center that supports hospitals across multiple states, Cardinal Health’s success hinges on its frontline leaders.
The following leaders – Guy Antoine, Kacie Coker, and Mary Ann Tindall – represent the diverse expertise and commitment that powers Cardinal Health’s supply chain and operational excellence. From coast-to-coast transportation, to international trade compliance, to hands-on distribution leadership, each plays a unique role in making sure essential products get where they’re needed, when they’re needed.
Guy Antoine: Logistics
That Saves Lives
Guy Antoine and his team cover a lot of ground for Cardinal Health. As Senior Director of U.S. Transportation at Cardinal Health, Antoine oversees U.S. transportation, facilitating the reliable and efficient movement of products across Cardinal Health’s supply chain network.
That network supports more than 50 medical manufacturing plants and distribution centers, with more than 8 million deliveries annually to hospitals, distribution centers and non-acute care locations. It’s a vast and dynamic operation that includes a mix of Cardinal Health fleet and commercial carriers.
“My team plays a critical role in ensuring every shipment supports the continuity of patient care,” Antoine said.
To achieve this, it is essential that the supply chain accounts for the complexities of transportation to provide outstanding experiences for Cardinal Health’s customers. “Through my role, I work to ensure we have a team of exceptional people supporting transportation and helping advance our strategic planning.”

Across a large team like this one, Antoine said success shows up in many forms. “Ultimately, it is delivering on our service commitments no matter what the week throws at us,” he said. “We’re actively engaged with our cross-functional partners –some including sales, marketing, IT, distribution operations and
others – to perform at our best and proactively manage any issues. Success also means we effectively manage our day-to-day responsibilities, whether by executing standard processes or deploying contingency plans to overcome the week’s challenges.”
Maintaining a transportation network that ensures timely and reliable delivery of critical medical products starts by working backward from the promise Cardinal Health makes to its customers to deliver the critical products and solutions they need – when and where they need them. “Those commitments shape how we invest in our infrastructure and how we execute our operational work,” Antoine said. “That’s why we’ve made significant investments in our systems – building our own Transportation Management System (TMS) and logistics platform tailored to the unique needs of our business.”
In healthcare, hospitals must remain operational – even during crises like natural disasters. That can be incredibly challenging, especially when facing events like hurricanes. “Typically, when a storm is approaching, we track its path closely and take proactive steps to mitigate risk. If one of our distribution centers is in the storm’s path, we reposition our fleet, develop alternate fulfillment plans, secure fuel trucks and even arrange hotel accommodations for our drivers and their families,” Antoine
Guy Antoine
SAVE on Surface Disinfection with CaviWipes ™ HP & CaviCide ™ HP

Efficient Disinfection
Efficient Disinfection
Hydrogen peroxide-based 1-step cleaning/disinfection2 and 1-minute contact time for all listed pathogens ensures efficient disinfection.
Hydrogen peroxide-based 1-step cleaning/disinfection2 and 1-minute contact time for all listed pathogens ensures efficient disinfection.
Broad Spectrum Efficacy
Broad Spectrum Efficacy
Effective disinfection against over 60 pathogens1 including MDRO’s (Multidrug Resistant Organisms) while qualifying for the EPA’s rigorous Emerging Viral Pathogen Claim3, protects you against future pathogens as well.
Effective disinfection against over 60 pathogens1 including MDRO’s (Multidrug Resistant Organisms) while qualifying for the EPA’s rigorous Emerging Viral Pathogen Claim3, protects you against future pathogens as well.
Ease of Use
Ease of Use
Pre-saturated wipes and ready-to-use liquids require no mixing or dilution simplifying the disinfection process, reducing the risk of errors, saving time, and improving compliance.
Pre-saturated wipes and ready-to-use liquids require no mixing or dilution simplifying the disinfection process, reducing the risk of errors, saving time, and improving compliance.
Lowest Toxicity Level
Lowest Toxicity Level
US EPA Toxicity Category IV products minimize exposure to harmful cleaning chemicals. The use of gloves is not required.2
US EPA Toxicity Category IV products minimize exposure to harmful cleaning chemicals. The use of gloves is not required.2


1. 67 pathogens for CaviWipes HP and 70 pathogens for CaviCide HP
2. Follow Product Label for special precleaning and PPE instructions
3. CaviCide HP and CaviWipes HP qualify for the EPA Emerging Viral Pathogen program against all virus tiers (enveloped, small and large non-enveloped)
Emerging Viral Pathogen program against all virus tiers (enveloped, small and large non-enveloped)
said. “All of this ensures that the moment our customers are ready to receive shipments again, we’re there and ready to deliver. In this field, logistics isn’t just about moving boxes – it’s about being there when it matters most.”
Cardinal Health also invests in its people. “By keeping our control tower – a hub similar to an air traffic control tower that analyzes and directs operations – within Cardinal Health, we maintain visibility and control over our operations,” Antoine said. This is essential for responsiveness and reliability.
“Our carrier network is equally important,” he said. “At Cardinal Health, we partner with a select group of strategic carriers whose values and culture align with ours. Their management teams and drivers understand the critical nature of healthcare deliveries, and that shared commitment makes a real difference in getting products to customers on time.”
Kacie Coker: Managing the Nuances of Global Trade
For Kacie Coker, no day is ever the same. As Director of Global Trade Strategy & Productivity for Cardinal Health’s Global Medical Products and Distribution business, Coker serves as a subject matter expert on existing and new global trade regulations and guides the business on strategic projects to navigate those regulations, helping the organization stay both compliant and costcompetitive. She collaborates with Cardinal Health’s sourcing and manufacturing teams to provide guidance and understanding of duty savings programs, like the Nairobi Protocol and Free Trade
Agreements, to help enhance the organization’s supply chain efficiency. She also works closely with the Government Relations team to look for opportunities to advocate for trade legislation that will improve Cardinal Health’s ability to deliver medical products to customers on time and at a reasonable cost.
“Lately, much of my time is spent diving into the nuances of new trade regulations to understand how they might impact our business, then communicating and educating our team on how they can respond to these changes,” she said.
Importing and exporting play a pivotal role in the execution phase of the supply chain. This is even more important when you are importing and exporting materials and products that are critical to healthcare, Coker said. A delay at any point in the process can mean the difference between a surgery operating on schedule or being delayed weeks or even months. “Every step we take toward making our products more cost effective and move
more efficiently through the supply chain has a direct connection to a patient and their story,” she said. “That perspective helps us stay focused on striving to improve our processes every day.”
Working in a multinational company means encountering situations where countries interpret regulations differently and may even conflict with one another. It’s helpful to have systems and data infrastructure that are flexible enough to allow for these differences in interpretations and able to manage the trade data accordingly, Coker said.
“There is no ‘one size fits all’ approach to trade compliance,” she said. “To manage global trade regulations well, your systems, data and people must be nimble and flexible enough to manage these nuances.”
Spending her entire career in global trade, Coker said she has been fortunate to develop an amazing network of fellow trade compliance “nerds” who are highly knowledgeable and passionate about this line of work. “As regulations evolve, it is mutually beneficial to stay connected with my network to discuss the implications of these changes, and brainstorm ideas on how to manage them.”
Coker believes that trade compliance, when done well, can absolutely be a competitive advantage for a company rather than a hurdle. It’s important for trade compliance as a function to not become so siloed that you lose sight of the goals and initiatives of the business you are supporting. In any compliance function, there will absolutely be situations where you must say no. “However, I strive to use those as
Kacie Coker
MedPro is a contracted medical sales organization serving leading manufacturers across every major care setting.
Our clinically trained, HIDA AMS-accredited sales professionals are strategically located throughout the country, delivering expert, in-person support to providers and streamlined execution for manufacturers and distributors alike.
Scan the QR Code to Connect with Us.
opportunities to say ‘No, but…’ and then offer solutions that will allow the business to meet their objectives while still maintaining compliance with the necessary regulations,” she said.
Mary Ann Tindall: Operational Excellence at Cardinal Health Detroit
At the helm of Cardinal Health’s Detroit medical products distribution center, Mary Ann Tindall, Director of Operations, is a driving force behind one of the company’s most innovative and high-performing facilities. With a strategic mind and a deeply rooted commitment to both people and process, Tindall leads her team with a clear vision: exceed expectations in serving healthcare providers while fostering a culture of continuous improvement and empowered leadership.
Tindall’s role encompasses far more than logistics. She oversees daily operations with a sharp focus on operational efficiency, employee engagement, regulatory compliance, and strategic growth. Her leadership philosophy is built around harmonizing disciplined execution with adaptability –essential qualities in an industry where every delivery can impact patient care.
The Detroit distribution center serves an important role in Cardinal Health’s North American network. Covering customers in Michigan, Northern Ohio, and Northern Indiana – with flexibility to ship nationwide – the facility is not just a distribution center but a model of adaptability and innovation. “Our team also provides critical support to other facilities during extreme weather or major logistical transitions,

“ We embrace a growth mindset –persistently tackling challenges, learning from our mistakes and continuously seeking ways to improve our processes.”
such as new site launches,” she said. “Our team is committed to operational excellence, backed by strong, experienced leadership and has a reputation for developing future leaders.”
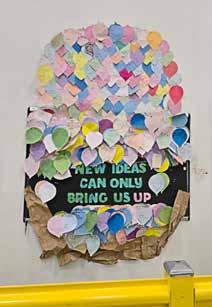
At the core of the center’s success is its people. Tindall proudly describes her team as highly engaged and inclusive, with a strong culture of accountability and ownership. Her leadership has helped foster a growth mindset across the workforce, where employees are encouraged to challenge the status quo, explore new ideas, and learn from both successes and setbacks. “We embrace a growth mindset – persistently tackling challenges, learning from our mistakes and continuously seeking ways to improve our processes.”
A standout example of this engagement is the facility’s 100% associate-led safety program, which emphasizes weekly safety tasks completed by employees themselves. This initiative strengthens the safety culture by making each team member a stakeholder in the workplace environment. Another creative approach is the “Balloon Board,” a playful yet impactful idea-sharing platform where employee suggestions take flight – literally – when implemented. “If an idea is implemented, we ‘fly’ the balloon; if it’s not feasible or is not adapted, we ‘pop’ it and ‘falls’ in a basket,” she said. “Together, these balloons form a large hot air balloon display, symbolizing our collective innovation.”
Over seven years, the initiative has created a rich database of tracked ideas, demonstrating the
Mary Ann Tindall
team’s long-standing commitment to improvement.
Daily operations are structured around core principles: precision in receiving, speed and accuracy in outbound execution, and unwavering responsiveness to customer needs. Automation tools, including visual verification systems and robotic assistance, support consistent order fulfillment while improving safety and reducing physical strain.
Tindall attributes much of the center’s success to the disciplined use of Lean Six Sigma practices, particularly Leader Standard Work. This framework ensures operational consistency while
allowing time for innovation and project-based improvements. Her team’s mindset is grounded in purpose: they recognize the realworld impact of their work, especially in a healthcare landscape where every shipment matters.
One of Tindall’s proudest recent achievements is the national recognition of her Quality Inventory Control team. Their work has earned them top performance status across all U.S. Cardinal Health distribution centers – a testament to their precision, dedication, and alignment with the organization’s high standards.
“This small but mighty group handles all customer inventory concerns, identifies and resolves
employee errors, and addresses product and packaging issues,” Tindall said. Team members work with exceptional diligence – even on weekends if needed – to ensure inventory transactions are executed flawlessly and investigations are completed thoroughly. Their efforts result in high inventory accuracy and reliability. Though their work is often behind the scenes, it plays a critical role in driving overall warehouse performance and enhancing customer satisfaction.
“Their commitment, precision and ownership exemplify the high standards we strive for every day,” she said.
Marketlab unites specialty healthcare products across nine trusted brands—to support the work of care, every day.

Sustainable Care Starts Here
Henry Schein’s strategy to make the healthcare supply chain greener.
 Jennifer Kim Field knows what it takes for the U.S. healthcare supply chain to forge a more sustainable future. The healthcare sector contributes approximately 8.5% of total U.S.-based greenhouse gas emissions (GHG) and 4% of total global GHG. Thinking big picture, if the healthcare sector were a country, it’d be the world’s fifth-largest emitter of greenhouse gases.
Addressing healthcare emissions could make a significant dent in climate efforts. Initiatives include reducing single-use plastics, decarbonizing energy use, reprocessing devices, and switching to greener anesthetic gases. But those are tasks no one company can undertake on its own. “It’s going to take all of us collectively to make that greater impact,” said Field, Vice President and Chief Sustainability Officer for Henry Schein, Inc. and Interim President for the Henry Schein Cares Foundation.
Indeed, Henry Schein’s Chairman and CEO Stanley Bergman often quotes the African proverb, “If you want to go fast, go alone, but if you want to go far, go together.”
A “BOLD” plan
Sustainability is part of Henry Schein’s culture and values, particularly through the “Three Cs”: Community, Caring, and Career. It’s also embedded in the company’s corporate strategic plan known as BOLD+1:
` B – Build complementary software, specialty, and services businesses
` O – Operationalize a unified distribution model
` L – Leverage all businesses to deepen customer relationships
` D – Drive digital transformation
` +1 – Create shared value for all stakeholders (customers, Team Schein Members, suppliers, shareholders, and society)
Henry Schein’s BOLD+1 strategic plan is guided by a detailed blueprint composed of key pillars, each backed by specific goals and commitments. Field said stakeholder engagement is key in shaping these priorities.
A central focus of the plan is the well-being of Team Schein Members (TSMs), who are seen as vital to the company’s success. Efforts to support Team Schein include wellness initiatives, professional development programs, and community involvement opportunities such as the Company’s flagship “Back to School” and “Holiday Cheer” volunteer programs. These initiatives enhance the TSM experience and contribute to broader community health.
Field outlined two additional core components of the strategy: good governance and environmental stewardship. Henry Schein encourages its supplier partners to align with the company’s global supplier code of conduct that outlines clear expectations of environmental practices, labor conditions, and ethical standards. “Having those key policies in place builds the foundation for everything else,” Field said.
On the environmental front, Henry Schein is committed to building a sustainable and resilient supply chain. Earlier this year, the Science Based Targets initiative (SBTi) approved the
by 2030 and achieve net-zero emissions by 2050.
On the supplier side, the company works with business partners to help identify sustainable product alternatives and find ways to reduce packaging waste like single-use plastic (a top question of customers). Henry Schein also works with its partners to help lower emissions throughout the value chain.
In 2023, Henry Schein launched its global Practice Green initiative to empower the healthcare sector (both medical and dental) with ways to reduce their environmental footprint while still providing
“ Whether it’s a big action or small, anything makes a difference. You just need to start – take a step now toward promoting a healthier planet and healthier people.”

company’s near-term and longterm science-based emissions reduction targets, reflecting Henry Schein’s commitment to significantly cut carbon emissions
high quality patient care. The initiative provides customers and suppliers with product solutions that are reusable, made from recycled materials, are recyclable or biodegradable, and are sourced sustainably.
The program includes more than just eco-friendly items –it offers educational content, guidance, and services (such as waste management partnerships) to support sustainability while ensuring top-quality patient care and regulatory compliance.
Practice Green also helps practices monitor savings and environmental improvements, tracking waste reduction and cost savings, from cutting disposable supplies to using energy
Jennifer Kim Field
efficient alternatives. A portfolio of partnerships (e.g., recycling services, specialty consultants) further supports responsible practice operations.
Clean horizons
Field said of all the recent technological innovations, she is most excited about the potential of AI in advancing sustainability efforts. AI is already helping to streamline data consolidation and analysis, which can significantly improve strategic decision
biggest goals the industry must work toward over the next five to ten years. She emphasized that while sustainability is now a baseline expectation in the business world, implementing it at scale – especially across a global, complex supply chain – is extremely difficult. Maintaining product quality, affordability, and accessibility while adapting to evolving global regulations and stakeholder demands adds to this complexity. However, she remains optimistic, seeing
Henry Schein’s Practice Green:
` Offers a globally launched, eco-focused framework tailored to healthcare settings
` Simplifies sustainability through a vetted green product portfolio
` Provides holistic support – from education to services
` Encourages accountability through tracking and partnerships
making. Within Henry Schein, AI is also being used in innovative ways. For example, Henry Schein One’s Dentrix ® Detect AI, powered and manufactured by VideaHealth, is an AI-enabled X-ray analysis tool that provides real-time clinical decision support to dentists.
“There’s a power to AI that we’re just now unlocking,” she said, “but we need to do it in a careful, methodical and intentional way. I appreciate that we, as a company, have an AI committee. We have rules and reviews that are key.”
As far as improvements, Field identified the need to break down silos and foster greater collaboration as two of the
significant potential for innovation and meaningful impact if businesses and governments work together and stay committed.
Field also stressed the importance of action over perfection. “You have to start somewhere,” she said. “Don’t let perfection be the enemy of the good.”
She encouraged companies to start somewhere, however small, and to use their collective influence to advocate for change. Despite the complexities and pressures, she points to advancements in AI, renewable energy, digital tools, and sustainable packaging as enablers of more efficient, lower-impact operations. “Whether it’s a big action or small, anything makes
a difference,” she said. “You just need to start – take a step now toward promoting a healthier planet and healthier people.”
Sustainability at the individual level – particularly sales representatives engaging directly with physician offices – can take many forms. Field said one impactful approach for TSMs is community involvement, such as participating in local cleanups alongside customers. These activities, often organized through the Company’s “Green Team Schein,” initiative serve not only to benefit the environment but also to strengthen customer relationships in a meaningful, values-driven way. “Green Team Schein” is the Company’s global employee volunteering efforts, such as beach clean-ups and planting gardens and trees.
Another way individuals can make a difference is by integrating sustainability into everyday business conversations, particularly through the Practice Green initiative. Team Schein Members can educate customers on sustainable product alternatives, offer resources such as sustainability checklists, and help health care professionals make more sustainable purchasing decisions. For example, TSMs can review inventory and order history to recommend shipment consolidation.
“So, rather than one or two shipments of one or two boxes going out per day, could customers wait two or three days, get that collectively – and not only have cost savings, but also have emissions savings,” Field said. These small, practical changes collectively support both environmental and business goals.
Protecting Patients from Hidden Harm
Hospitals Confront Toxic Chemicals in IV Therapy
All patients face some risk with IV therapy, but the neonate and pediatric population, the elderly, and oncology patients are especially vulnerable due to their immunocompromised status.
A key concern is exposure to DEHP, a chemical found in some IV products that acts as an endocrine disruptor. Despite being banned from children’s toys, DEHP is still present in medical devices, raising concern particularly for pediatric and breast cancer patients due to its hormonal impact, said Anita Zado, Vice President Clinical Services with Capstone Health Alliance.
“It has been proven time and time again that DEHP increases the risk around these patients,” she said.
During a recent podcast with The Journal of Healthcare Contracting, the sister publication of Repertoire Magazine, Zado and several other clinical supply chain leaders from hospitals and health systems said that hospitals must engage multiple departments to manage risks, communicate changes, and ensure safe product use. These leaders discussed patient safety and environmental sustainability, as well as how they were assessing new patient safety legislation in

California, the Toxic Free Medical Device Act or AB 2300, and its potential impact on the IV therapy products they utilize at their facilities. The panelists were:
` Angelique Vuilleumier, Senior Director, Supply Chain Legacy Health
` Anita Zado, Vice President Clinical Services with Capstone Health Alliance
` Grace Kistner, Project and Policy Analyst
` Lobel Lurie, Manager, Clinical Value Analysis, Strategic Sourcing with Cone Health
` Jennifer Browne, Corporate Director, Value Analysis with LifeBridge Health
Chemicals of concern
DEHP is LifeBridge Health’s primary chemical of concern due to its well-documented health risks, Browne noted. In addition to DEHP, her health system also aims to minimize exposure to mercury, other phthalates, latex, and even anesthetic gases – especially when these pose risks to vulnerable patient populations.
She said that while some chemical effects, like latexinduced anaphylaxis, are immediate and well-known, others may have long-term or hidden impacts on the body. This uncertainty reinforces the importance of educating healthcare providers and staff to understand what chemicals are in the products they use and to make informed, cautious choices when those chemicals can’t be completely avoided.
Vuilleumier shared that her health system is focused on reducing exposure to a broad range of chemicals of concern, including antimicrobials, BPA, anesthetic gases, and chemicals used in labs,
cleaning, disinfection, and sterilization. Their goal is to protect patients, staff, and the environment from health risks such as cancer, reproductive harm, and respiratory issues, while also supporting sustainability efforts.
Legacy Health collaborates with Practice Greenhealth and participates in their chemical reporting programs. They also work closely with their GPO, sitting on its sustainability committee to exchange strategies with other health systems. Their GPO helps identify contracts that involve chemicals of concern, allowing Legacy to consider alternative suppliers through RFPs (Requests for Proposals).
AB 2300
Kistner, a registered nurse and policy analyst in California, shared her strong support for AB 2300, a bill addressing the use of toxic chemicals – specifically DEHP– in medical products. She explained that these chemicals, commonly found in IV and respiratory tubing, can leach into patients’ bodies, posing serious health risks such as cancer, reproductive harm, and neurological issues. Most nurses are unaware of these risks, despite being directly exposed themselves.
Kistner also highlighted the environmental impact of plastic waste in healthcare, noting that incinerating medical plastics releases toxic dioxins into the environment.
“It’s also in our broader environment,” she said. “This is a community and population health issue. It goes beyond the bedside.”
Lurie believes AB 2300 has the potential to support patient safety initiatives, but its success depends on strong partnerships
with industry. She stressed the importance of transparency from manufacturers, particularly in clearly communicating their efforts to eliminate or reduce DEHP in medical products.
When suppliers clearly label products as not made with DEHP and share their action plans, it builds confidence and reduces the burden on healthcare systems to verify safety – ultimately protecting patients more effectively. Lurie concluded that holding industry partners accountable and communicative is essential for the law to truly advance patient safety across health systems.
The importance of
supporting sustainability initiatives Zado acknowledged the current challenges in supply chain – such as product shortages and tariff impacts – but emphasized that health systems with well-structured Environmentally Preferable Purchasing (EPP) programs are leading the way in sustainability. She highlighted that integrating clinical and supply chain teams can promote safer products, reduce waste, and improve ethical procurement, contributing to better patient outcomes, cost savings, and environmental health. She noted that the future lies in valuebased supply strategies that align cost control with sustainability.
Kistner reinforced this by stressing that health systems can act proactively – they don’t need to wait for legislation like AB 2300 to make sustainable changes. She pointed to California healthcare leaders who eliminated toxic chemicals like DEHP before being required to, achieving both better patient outcomes and financial savings. She advocated
for aligning sustainability with the Quadruple Aim – improving care, outcomes, provider well-being, and cost – through collaborative, informed decision-making.
Commitment to safer products
Panelists praised B. Braun for its early and sustained leadership in removing DEHP and PVC from many of their IV therapy products, emphasizing the positive clinical, financial, and sustainability impacts on their health systems.
Vuilleumier said Legacy has used B. Braun’s IV products not made with DEHP and PVC for years. In a recent 2024 RFP, B. Braun was again selected due to their alignment with governance priorities like environmental sustainability, patient safety, and costeffectiveness. Zado has worked with B. Braun since 2010 and commended their long-standing commitment to safer products without added cost. Lurie said B. Braun products were successfully introduced during an IV shortage caused by a hurricane, leading to strong clinical acceptance and familiarity. Browne appreciates B. Braun’s leadership in removing DEHP, noting it is a differentiator in the marketplace.
Indeed, as healthcare systems work to safeguard vulnerable patients, reduce harmful chemical exposure, and meet evolving legislative standards, collaboration across clinical, supply chain, and industry partners is more essential than ever. With leaders embracing transparency, sustainability, and innovation, the path forward points to a future where patient safety and environmental responsibility go hand in hand.





















































































































Medical Gaslighting
A disparity of trust between clinicians and patients.
By Pete Mercer
 In healthcare, one size does not fit all. Each patient has a unique and dynamic health background that often requires a tailored approach to addressing their health concerns. While there is an overall foundational approach to treatment options, it needs to be a good fit for the patient. Otherwise, they might be getting treatments that are not necessary, effective, or even worse, could cause further harm to the patient.
A recent report published by the ECRI found that “dismissing patient and caregiver concerns” is at the top of the list of the most significant threats to patient safety in 2025. In a media release regarding the report, ECRI says that “time and resource constraints make it increasingly difficult for some clinicians to provide empathetic care that addresses patient and caregiver concerns, potentially leading to missed and delayed diagnoses.”
This is indicative of a larger problem – a lack of trust between clinicians and patients. ECRI is referring to this phenomenon as medical gaslighting, a term that the American Journal of Medicine has defined as “an act that invalidates a patient’s genuine clinical concern without proper medical evaluation.”
To get a better understanding of what medical gaslighting is and how it impacts clinicians and patients alike, Repertoire Magazine spoke with Shannon Davila, MSN, RN, CPPS, CIC, CPHQ, FAPIC, executive director of total systems safety at ECRI, and Marcus Schabacker, MD, PhD, president and CEO of ECRI.
What is medical gaslighting?
An important thing to understand about medical gaslighting is that the traditional definition of gaslighting (i.e. manipulating someone in such a way that they begin to question their own sanity) does not apply to medical gaslighting. In a medical gaslighting case, patients feel that their health concerns are not being validated or addressed by their clinicians. It is also important to understand that this is not a new experience. For years, patients have complained about feeling
dismissed or not heard when it comes to their own health concerns. In recent years, there have been a couple of high-profile cases where celebrities have experienced medical gaslighting. After Serena Williams had a baby in 2017, she experienced shortness of breath and alerted medical staff to the issue. They did not believe her at first, but a CT scan revealed pulmonary embolism.
Sharon Stone has also recently been more candid about her experience with a ruptured vertebral artery in 2001. In her case, the doctors missed it on the first scan, so they assumed there
was nothing wrong with her. After getting a second opinion, Stone had to undergo a procedure to get it fixed.
In both cases, the situation could have resulted in more serious injury or even possible death if they had not advocated for themselves over and over again. Celebrity cases like these go a long way in raising awareness for this issue. In the Hippocratic Oath, young and upcoming doctors swear to “do no harm” – the reality is that most healthcare professionals take that creed very seriously.
Davila said, “We wanted to be sensitive when we brought
this issue up because healthcare is such a complex environment –doctors, nurses, and others are being asked to do so much with limited resources every day. Most people, the majority of healthcare workers, do not go to work saying, ‘I’m going to ignore or disregard a patient.’ No one has that intent. They always want to do the best for their patients.”
So, what is happening here? Without a doubt, healthcare workers face an enormous amount of pressure on a daily basis. They can only commit a certain amount of time to each
Offering
Sterile Water and 0.9% Sodium Chloride Solutions for Injection and Inhalation made in North America
AMSure® Sterile Water and Saline products are important for infection prevention, hydration, drug delivery, humidification, suctioning, inhalation, irrigation, inflation, and many more healthcare applications.
• Hanging Spikeable Bottle for Inhalation – Intended to reduce solution mixups with traditional IV bags
• Unit-Dose Vials in both Sterile Water and Saline
• Pre-Filled Humidifiers
• Manufactured in Illinois, USA
Praxiject™ Pre-Filled 0.9% Saline Syringes are secure, reliable, and accurate.
• Available in Sterile Path and Sterile Field ready configurations
• Complies with PICC and INS Standards
• Manufactured in Canada

our team or visit







patient, which creates this tension between caring for each patient and maintaining productivity goals. Additionally, cognitive bias can also lead to patients feeling as though they are being dismissed. The ECRI report found that, whether they know it or not, many clinicians have “biases that reflexively attribute symptoms to issues like mental illness, age, or weight,” which can greatly influence diagnostic decisions.
The patient-clinician relationship
Inevitably, this scenario will have an impact on the patientclinician relationship. The most significant casualty in this medical gaslighting scenario is trust. Overcoming that barrier of distrust in the patient-clinician relationship is very difficult when the patient feels like they have been dismissed. With all of the health issues that many adults in
“ We know nobody wants to be perceived as dismissing patient’s concerns. We saw an opportunity to educate health providers, but this was not just about education – we also wanted to acknowledge the patients and families.”
As an example for what this can look like, Davila said that if a clinician in an emergency department at a hospital sees five patients and they are all diagnosed with the flu, the sixth patient that comes in with a fever and a cough, it’s possible that that patient would be diagnosed with the flu as well.
Whether they know it or not, providers walk into each interaction with a patient with some sort of bias that is informed by circumstances that may or may not be related to the specific patient they are seeing. “You have to really think independently for each patient. Cognitive bias might be different than medical gaslighting, but it’s still not processing the information in a really critical and thoughtful way so that you can make the right diagnosis,” Davila said.
America are facing right now, it’s really important to have a clear and open dialogue about what the patient is experiencing. If the patient does not feel comfortable sharing that information, it’s detrimental to the entire healthcare ecosystem.
Davila said, “A patient only has to feel like they have been dismissed once by someone. If you are having a conversation with anyone and you feel like they are being disrespectful or not hearing you, you are probably not going to feel comfortable communicating with that person.”
Once this starts to impact the patient-clinician relationship, it can become quite difficult to rebuild that trust. At some point, the patient could begin to withhold important information about their symptoms or their overall health. From there, any diagnosis
that the clinician is going to give might be looked at with some measure of skepticism. If they do not feel that they can trust the clinicians, why would they trust the diagnosis?
That’s even assuming that the diagnosis is correct – if the clinician is given the full scope of health or they are not listening to the concerns of the patient, it becomes much easier and much more common to misdiagnose.
“From a clinical standpoint, it really opens up the opportunity for diagnostic errors,” Davila said. “If patients do not feel comfortable sharing about things like depression and anxiety – or in the case of Serena Williams, a physical chest pain – then you are going start seeing that the providers are not getting the information that they need to adequately make those diagnoses.”
Davila and her team found that by putting medical gaslighting as a top safety concern, they had multiple people share that they had also experienced medical gaslighting at some point. While they knew it was important to use this as an opportunity to educate providers about this issue, it was not the only goal of the report.
“We know nobody wants to be perceived as dismissing patient’s concerns. We saw an opportunity to educate health providers, but this was not just about education – we also wanted to acknowledge the patients and families. We know this is happening and we really wanted to help their voices be heard,” Davila said.
What can be done?
With a clearer picture of the scope of medical gaslighting, how
can healthcare organizations put structures in place to fix this?
ECRI president and CEO Marcus Schabacker said that the first step to rectifying any of the systemic flaws that perpetuate adverse events like medical gaslighting and cognitive bias is to create an environment where the staff feel safe to report errors, near misses, and system vulnerabilities. He calls this a ‘just culture.’
“Just culture is a model of accountability – one that applies not only to individuals, but also to the organization itself,” he said. “It recognizes that while individuals are responsible for their choices, the organization
is responsible for shaping those choices. In a just culture, clinicians are held responsible for their actions. At the same time, the organization is accountable for designing systems that support safe, effective care and for responding to failures with learning, not punishment.”
When staff members feel safe to report any issues, it will help healthcare organizations to build robust data that gives a better picture of any vulnerabilities and risks. From there, the data can be analyzed to identify the challenges and create proactive prevention measures to mitigate those challenges.
According to Schabacker, leaders have to model transparency, reinforce safety as a core value, and ensure that policies and workflows reflect the realities of the clinical practice to reinforce the accountability between clinical staff and clinical leadership. If it’s going to work, leadership has to set the tone for the rest of the organization.
On the other side of the equation, frontline clinicians need to know that speaking up about risks or mistakes is not just safe, but an expectation. “Together, this dual accountability creates the foundation for total systems safety: a healthcare



environment where safety is embedded, trust is reinforced, and learning is continuous.”
Improving patient safety through a unified, systems-based solution
Ensuring the safety of the patient is paramount to improving the quality of the clinician-patient relationship and eradicating medical gaslighting. Developing a systems approach is essential for healthcare organizations that are aiming to achieve safe, high performing, and efficient patient care, rooted in the understanding that healthcare is a complex, adaptive, sociotechnical system.
“Outcomes are shaped not just by individual actions, but by the design of the system itself: its physical environment, tasks and processes, tools and technologies, organization, and people, as well as the external environments,” Schabacker said. “A systems-based approach seeks to identify and redesign the system components that influence outcomes in a manner that facilitates safe, effective, and efficient care.”
Improving patient safety protocols requires an all-handson-deck, uniform approach to overcome these challenges. According to Schabacker, shifting towards an integrated, systemwide strategy is the most effective way to improve patient safety, like embedding safety deep into the organizational culture, aligning incentives, and using shared frameworks to guide improvement at each stage of the journey.
Building a strong safety culture is a big step towards improving patient safety, simply by making it a priority across the

By leveraging unification and standardization, healthcare leaders are able to establish a firm foundation of safety that reflects the goals and vision of the entire organization, making it easier to create meaningful change.
board. He said, “A strong safety culture is one where safety is not just a priority, but a core value embedded in every decision and process. Cultivating this culture requires more than training, slogans, or frameworks. It involves redesigning systems to support safe behaviors, aligning policies with values, and modeling safety leadership at every level.” Implementing a culture that’s focused on safety will also require a unified front to ensure that everyone is aligned with the mission and vision of the leadership team. Without that unified approach, these strategies often result in greater fragmentation, which is another significant barrier to patient safety. If your organization is implementing siloed safety measures, it is much more difficult to scale these operations or align them with other departments in the organization.
Obviously, this does not create a sustainable, system-wide change
for providers. By leveraging unification and standardization, healthcare leaders are able to establish a firm foundation of safety that reflects the goals and vision of the entire organization, making it easier to create meaningful change. However, the main caveat here is that leadership needs to be willing to accept the hard truth about the state of patient safety today.
As organizations like ECRI continue to shed light on these issues, it will continue to bring awareness to things like medical gaslighting. But it requires the leadership teams to make challenging decisions in order for anything to change. “As long as boards, CEOs and senior executives continue to accept the alarmingly high rates of preventable harm in healthcare today as collateral damage, things will not change. We also need patients and the general public to become more aware and more vocal about the need to make healthcare safer.”


Breakthrough isn’t just about shattering barriers—it’s about transforming challenges into opportunities for growth. At the 2026 PWH® Leadership Summit, we’ll explore how resilience and transformation shape true leadership, embracing setbacks as stepping stones to becoming stronger, more impactful, and more valuable. Together, we’ll celebrate the beauty in imperfection and reframe breakthroughs—not simply as moments of breaking through, but as experiences of mending, evolving, and emerging better than before.
Having the opportunity to attend the PWH Leadership Summit pushed me beyond comfort zone levels. I was able to connect with so many women. I learned a lot and left the summit feeling a new sense of purpose in my leadership career. I look forward to spreading the word about the experience and encouraging others, especially my team, about participating in all PWH has to offer in the future!

Join Us To Be Inspired, Empowered, and Equipped To Create Your Own Breakthrough Open to women & men from all career levels – Aspiring Leaders to C-Suite Executives. Gain actionable takeaways through our PWH Leadership Insights (TED-style talks), empowering keynote speakers, engaging panel discussions, workshops & breakout sessions that cover a host of topics around pressing leadership issues.
Register today to attend the industry’s only conference completely dedicated to inclusive leadership development.
Registration now open at mypwh.org

The State of Rural Healthcare
The challenges facing rural healthcare and potential policy solutions.
By Jenna Hughes

 Nearly 46 million people in the U.S. live in rural areas, and roughly 77% of rural counties in the U.S. are considered healthcare deserts, or geographic regions where residents face significant barriers to healthcare access, according to the National Rural Health Association (NRHA).
There are numerous ways to define rural health. The federal government designates more than 70 different ways of defining rural health across various agencies.
NRHA, a national membership organization that represents more than 90% of the nation’s rural hospitals, rural health clinics, and rural community health centers, strongly recommends that definitions of rural be specific to the purposes of the programs in which they are used, and that they are referred to as programmatic designations and not as definitions.

“At NRHA, we define rural America as a place where those most in need of healthcare services often have the fewest options available to access that care,” said Alan Morgan, Chief Executive Officer of NRHA. As CEO, Morgan oversees the organization’s educational, program and policy activities.
NRHA aims to address rural health challenges by identifying best practices, sharing those best practices for replication and working through legislation and regulation to remove barriers to expanding them.
“NRHA has stayed true to the same mission for more than 40 years – promoting leadership and developing healthy rural communities both for the health system and for healthcare delivery,” said Morgan.
Barriers to healthcare access
There are underlying similarities in healthcare access challenges among those living in rural America, regardless of location. These include workforce shortages, greater distances for patients to be able to seek care between access points, and significant health disparities.
“It is not unusual to have a life expectancy among rural populations that are 20 years less than their urban counterparts,” said Morgan. “It is unacceptable
that an individual’s length and quality of life is determined simply on where they live.”
Another issue is distance. Rural residents tend to travel farther to access care than urban residents.
“Where we find the greatest disparities among urban and rural populations is within behavioral health, maternity care, pharmacy access, long-term care, and more,” said Morgan. “This is due to fewer providers available, a culture that doesn’t always embrace behavioral health, distance from care, and higher rates of economic and community pressures than in urban areas.”
“Maternity deserts found in rural America are also substantial, and if a community lacks access to proper maternity care, young families will not be able to move there,” said Morgan.
Women in rural areas experience markedly higher rates of maternal morbidity and mortality due to lack of access to consistent maternity care, reproductive services, and postpartum support, according to the Rural Health Information Hub.
Rural community pharmacies also face many challenges to staying open, including low volume purchasing, slim profit margins,
“ It is not unusual to have a life expectancy among rural populations that are 20 years less than their urban counterparts. It is unacceptable that an individual’s length and quality of life is determined simply on where they live.”
Access issues

About 77% of rural U.S. counties are healthcare deserts, facing severe challenges like workforce shortages, long travel distances for care, and lack of access to services such as maternity care, behavioral health, and pharmacy support. These disparities often result in significantly lower life expectancy for rural residents compared to urban populations.
unfavorable insurance practices, and a limited pharmacy workforce.
“Over the last 15 years, more than 1,000 rural pharmacies have closed across the U.S., and more than 500 rural nursing homes have closed over the past decade,” said Morgan.
The loss of vital health services in these locations results in reduced access to care, increased healthcare costs, and significant economic strain withing rural communities.
The impact of hospital closures
Another challenge facing rural America is the widespread closure of hospitals and emergency rooms, a trend that threatens not only access to essential medical services but also the overall stability of rural communities – impacting emergency care response times to local economies and population health outcomes.
Since 2010, nearly 190 rural hospitals have shut their doors or discontinued inpatient services, according to NRHA. Nationally, nearly 50% of rural hospitals are operating with negative margins and are therefore vulnerable to closure.
“Rural hospitals are closing not because of low patient volumes or because people are moving out of rural America,” said Morgan. “Small rural hospitals are closing today because they have a disproportionate share of patients with high health needs and the inability to pay for that care, and bad debt is the reason these hospitals are closing across the U.S.”
When a rural hospital closes, not only does the community lose access to accessible health care, but a major employer and community
cornerstone ends, affecting the community at large.
“The problem when you lose a rural hospital is that you lose an anchor institution, a point of care, and in many cases the largest employer in the county,” said Morgan. “When a rural hospital closes, often the community follows. You lose the direct jobs in the hospital; you lose the indirect jobs that support healthcare. It is tough to quantify the loss of individuals that leave or do not move to the community because they don’t have access to 24/7 emergency room service care.”
Facing the rural staffing crisis
Addressing the rural healthcare crisis requires a variety of tactics, including telehealth, incentivizing healthcare providers to work in rural areas, the use of artificial intelligence, and strengthening state and federal funding for rural healthcare facilities.
One of the major reasons for rural hospital staffing issues is a lack of incentives for recent graduates to move to rural areas for work.
“Fewer than 4% of the nation’s incoming medical students come from rural America. Upper income urban students are going to school in urban areas, being trained in urban areas, and do their residency in urban areas,” said Morgan.
Training physicians in rural areas through rural residency programs not only provides greater access to care for rural communities, but also increases the likelihood of physicians practicing in rural parts of the country, according to the Health Resources & Services Administration.
“Rural residency training programs serve to attract rural kids with academic instructors

Closures threaten rural communities
Since 2010, nearly 190 rural hospitals have closed, primarily due to financial instability, not lack of demand. These closures remove vital access points for healthcare, eliminate key employers, and contribute to the economic decline and depopulation of rural communities.
that are passionate about healthcare in rural America, and these students are more likely to end up staying and practicing in rural areas,” said Morgan.
Addressing workforce shortages also requires the introduction of technological solutions
to ease patient load and administrative burdens on existing staff.
“Telehealth and telemedicine are also a great solution that’s successfully working within rural areas to address workforce shortages,” said Morgan. “Additionally, Artificial Intelligence (AI) technology
is increasingly being used for documentation, coding, and other administrative functions, freeing up staff time from nurses to clinicians to admin staff, and has had a real beneficial impact very quickly in rural communities”
Yet another obstacle facing rural Americans is patients needing to travel to receive healthcare. Often, residents in remote areas may have to travel significantly farther distances than those in urban communities to show up to in-person care.
Providers have increasingly relied on solutions like telehealth and AI to allow for more patient-facing time for rurally located, eliminating the burden of frequent travel for many residents with travel barriers.
“Telehealth is a great tool to expand primary care, but never a replacement for primary care,” said Morgan. “We must find the happy medium as to how we utilize technology to address workforce shortages without utilizing technology to eliminate any points of access to care that are currently there.”
Policy for change
Collaboration among healthcare providers, community organizations, government agencies and educational institutions is crucial to developing and
implementing policy changes that benefit communities facing location-based health disparities.
“Federal, state, and local policy leaders must be good partners with local healthcare because in many cases, they are the payors for this healthcare,” said Morgan.
public health wellness approach across communities helps both patients and providers, and is the first step to a healthier nation overall,” said Morgan.
The challenges associated with rural healthcare delivery often require physicians and health
NRHA’s advocacy policies include investing in a strong rural healthcare infrastructure, reducing rural healthcare workforce shortages, and building rural health opportunities.
“At NRHA, our partnerships with Group Purchasing Organizations (GPOs), technology companies, and medical device companies are incredibly valuable because they bring the real-world data from their customers and we’re able to make a strong policy case on the implications of adverse policies,” said Morgan.
NRHA’s advocacy policies include investing in a strong rural healthcare infrastructure, reducing rural healthcare workforce shortages, and building rural health opportunities.
“Promoting a policy approach that keeps Americans healthy and out of hospitals in the first place, and promoting a
Solutions
The National Rural Health Association (NRHA) promotes solutions such as rural medical training programs, telehealth, AI tools, and public policy reforms. Innovation is emerging from rural “healthcare hubs” that are finding creative ways to deliver care despite limited resources, helping shape the future of U.S. healthcare.
systems to find creative approaches to continue delivering patient care. Hundreds of towns across the U.S. are currently serving as ‘innovation hubs,’ or healthcare settings stretched thin that are consequently fostering collaboration and innovation; and these places are having a significant impact on the redesign of the nation’s healthcare system as a whole.
“All of the innovative, creative things that are happening within healthcare delivery and policy today are beginning in small towns across America,” said Morgan. “If you want to see what the healthcare system is going to look like 20 years from now, visit any small town today and you will see coordinated care, an emphasis on primary care, the use of community healthcare workers as a bridge between the community and providers, telehealth use, and AI technology solutions. The rural health system is stretched to the max with high health needs and low reimbursement, but through creative approaches these physicians are making it work.”
The Value of Print

In a recent survey, Repertoire readers expressed a strong preference for the print edition of the magazine due to several recurring themes:
Screen Fatigue and Desire for a Break
Many readers are on computers all day for work and appreciate the print edition as a way to disconnect from screens and avoid blue light, email distractions, and digital overload.
Accessibility and Availability
Print magazines are accessible at any time, don’t require internet or setup, and serve as visual reminders to read. They’re also often kept for future reference or shelf use.
Tangible and Convenient Experience
The physical format allows for easy flipping, bookmarking, and sharing. Readers enjoy the tactile, “hands-on” experience of holding the magazine, turning pages, and carrying it with them — whether to read during travel, in waiting areas, or at home.
Preference for Traditional Media
A number of readers describe themselves as “old school,” appreciating the familiarity and comfort of traditional printed materials in a digital world.
Reference Tool
The print edition of Repertoire Magazine is also used by many reps as a reference tool during customer visits and helps readers quickly scan for new products or industry updates without needing to navigate multiple websites.
Overall, readers expressed they value the print format for its ease of use, freedom from digital distraction, and lasting, physical presence.
“I want to thank you and your team for the work you do with Repertoire. I actually sold a Wolf X-Ray machine last month due to seeing their ad in the magazine. Repertoire is our connection to the industry, and a way to learn about new products. Keep up the good work!”
– Charlie Fricker McKesson Medical

Excellence in Long-Term and Post-Acute Care
Annual award recognizes facilities across the nation exhibiting excellence in the delivery of long-term and post-acute care.

 Post-acute, long-term and skilled nursing facilities play an essential role in the health care system by supporting patients as they recover and receive ongoing care beyond the hospital.
The American Health Care Association and National Center for Assisted Living (AHCA/NCAL) is an organization supporting longterm and post-acute care facilities across the nation in their mission to provide quality care solutions.
As a part of advocating for improved quality of care, AHCA/ NCAL’s National Quality Award Program announces awards in three categories annually: Bronze – Commitment to Quality; Silver –
Achievement in Quality; and Gold –Excellence in Quality.
Each award level requires an increasingly detailed demonstration of superior performance to earn national recognition, according to AHCA/NCAL. The Gold – Excellence in Quality Award, specifically, recognizes long-term and post-acute care facilities that meet rigorous standards of performance to further improve the lives of their residents.
Three skilled nursing care centers from Louisiana, Missouri and Kansas earned the most prestigious and esteemed Gold –Excellence in Quality Award level of AHCA/NCAL’s National Quality Award Program this year, including Garden Park Nursing & Rehabilitation Center, LLC in Shreveport, Louisiana, NHC HealthCare, Maryland Heights in Maryland Heights, Missouri and Nottingham Health and
Rehabilitation in Olathe, Kansas. These three facilities are among the best in the nation, according to AHCA/NCAL’s award criteria.
Striving for excellence
The Quality Award Program is based on the National Institute of Standards and Technology’s Baldrige Performance Excellence Program, a partnership dedicated to improving the performance and long-term success of U.S. businesses and other organizations in the areas of leadership, strategic planning, customer and workforce, operations and more.
“This award marks a significant milestone in our journey toward system-driven, innovative care. Guided by the Baldrigebased framework, we continuously refine our practices to align with our mission and strategic goals,” said Susan Taylor, Administrator of NHC HealthCare, Maryland Heights. “The recognition validates our focus on continuous improvement and organizational excellence, and it strengthens our resolve to lead with purpose and integrity.”
NHC is a comprehensive senior care facility offering longterm care, short-term rehabilitation and specialized memory care for individuals living with Alzheimer’s and other forms of dementia.
With a team of skilled professionals, the facility provides care plans designed to meet each resident’s unique needs.
Along with expert care, Silver and Gold Quality Award recipients have an 8% higher performance on hospital readmissions than the national average, and 9% lower registered nurse (RN) turnover than the rest of the nation, according to AHCA/NCAL.
Staff are the foundation of quality patient care and play a significant role in supporting patients to reduce readmissions, improve resident care plans and ensure patient safety.
“Receiving the Gold – Excellence in Quality Award is a tremendous honor that reflects the dedication of our entire team,” said Taylor. “It affirms our commitment to delivering compassionate, resident-centered care and reinforces the trust our residents and their families place in us. This recognition symbolizes our pursuit of safety, innovation, and excellence in every aspect of care.”
“Being named the first recipient in Louisiana of the AHCA/ NCAL 2025 Gold Excellence in Quality Award is more than a milestone, it’s a celebration of people,” said Jennifer Peters, Administrator of Garden Park Nursing & Rehabilitation. “For our team it means their passion, skills and relentless drive to improve lives have been recognized at the very highest level.”
Residents and families at each facility are equally grateful for the recognition, as it affirms their quality of care on a national level.
“For our residents, it’s a promise that every day, they will experience not just quality care,
“ Receiving the Gold – Excellence in Quality Award is a tremendous honor that reflects the dedication of our entire team. It affirms our commitment to delivering compassionate, resident-centered care and reinforces the trust our residents and their families place in us.”
Staff and resident impact
Key focus areas of the Quality Award Program include resident and family engagement and satisfaction, strong and effective leadership practices, a team-based approach, the use of data and feedback, proactive evaluation and improvement of processes and proven innovation across each facility.
Garden Park Nursing & Rehabilitation Center, another one of the 2025 Gold – Excellence in Quality Award recipients, is a 160-bed skilled nursing facility located on 26 acres just outside of Shreveport in Louisiana.
but the highest standard of comfort, service and compassion,” said Peters. “They are really proud to live somewhere that achieved a monumental victory, and they know that taking excellent care of them matters to us.”
“Our residents were proud to be part of this journey, actively contributing to meaningful changes and demonstrating that their voices matter,” said Taylor. “Families and community members recognize that while perfection may be elusive, our dedication to evolving and enhancing care is unwavering.”
Ultimately, the Gold – Excellence in Quality Award shapes a culture at each facility where residents feel valued and supported.
“For our residents and families, the Gold – Excellence in Quality Award is reassurance that they are receiving care from one of the best organizations in the nation – not just by the numbers, but because of the culture of compassion and excellence that they see every day,” said Breanna Gregory, Executive Director at Nottingham Health and Rehabilitation.
to be an Overall Five Star Center than facilities in the rest of the nation. To continue to achieve the highest quality care, each facility places a strong emphasis on continuous improvement, ensuring that care evolves with the residents it serves.
“We embed quality improvement goals into our daily routines, so they are never an afterthought but part of our culture. Leaders stay connected to the floor, listening to staff insights and removing barriers that stand in the way
“ This Award is a reminder that when your mission is rooted in heart and your values guide every decision that excellence is not just possible, it becomes the standard.”
Nottingham Health and Rehabilitation is a skilled nursing community serving a wide range of patients – from short-term rehabilitation after surgery or illness, to long-term residents who call Nottingham home.
“Our mission is Improving Lives, Exceeding Expectations (ILEE), and that extends across all levels of care,” said Gregory. “We provide private rooms for both Medicaid and private pay long-term care residents, along with specialty rehab services, in a homelike environment where clinical excellence and compassion go hand in hand.”
Quality improvement
The Gold Award recognizes facilities for their patient care driven by sustainable, systematic and effective practices.
In fact, Silver and Gold Award recipients are more likely
of better outcomes,” said Peters. “Most importantly, we tie every improvement back to our mission of ‘Improving Quality of Life’. When everyone understands the ‘why’ behind what we do, quality becomes more than a measure, but a shared purpose.”
A strong focus on continuous improvement has led facilities to see measurable improvements in their daily operations.
“One of our most impactful initiatives has been the creation of our Proactive Innovation Management System (PIMS). Unlike traditional improvement efforts that often react to problems, PIMS is a proactive system where we identify important processes – such as our engagement survey system – and ask how we can improve them, whether there are problems or not,” said Gregory. “For example, by applying PIMS to our employee
engagement survey process, we streamlined how feedback is collected, prioritized, acted upon, and communicated back to staff. The result has been higher participation, stronger trust in leadership, and better use of data to guide decisions.”
For NHC HealthCare, continuously striving to perform at a higher level has led to measurable enhancements in several key areas.
“Our pursuit of the Gold Award has led to increased focus on quality measures and data-driven analysis, increased long-term care census, reduction in antipsychotic use among short-term residents, restorative program reboot, strengthened advanced care planning for palliative care patients and much more,” said Taylor. “These outcomes reflect the power of a unified, quality-driven approach and demonstrate our commitment to sustainable change.”
Raising the bar
Ultimately, the vision of each facility once they have received this recognition is to continually strive for more for their postacute and long-term care facilities in the future.
“Our mission statement is ‘NHC Maryland Heights is committed to being the senior care leader in customer, partner and investor satisfaction,’” said Taylor. “This award is our team’s testament to our partners’ commitment to our mission statement.”
“Whether it’s adopting new care technologies, reimagining resident engagement programs, or discovering new approaches to support families, we know that the best care evolves with the needs of the people we
serve and those that serve them,” said Peters.
For Garden Park Nursing & Rehabilitation, The Gold – Excellence in Quality Award affirms that embracing new ideas and a commitment to person-centered care sets their organization apart.
“This Award is a reminder that when your mission is rooted in heart and your values guide every decision that excellence is not just possible, it becomes the standard,” said Peters.
AHCA/NCAL’s mission is to improve lives by delivering solutions for quality care, and
Facilities must go forward and continue to adapt to the changing healthcare industry, ensure that they are meeting resident’s evolving needs, and support their staff so they are able to perform at their best.
“Achieving Gold is a proud moment, but our journey doesn’t stop here. Our focus now is on sustaining excellence and sharing what we’ve learned with others. We want to continue building a workplace where staff thrive, expand partnerships in our community, and raise the bar for resident-centered outcomes,” said
long-term care – helping others on their journey to Bronze, Silver, and Gold. Excellence is never a destination; it’s a way of operating every day.”
Recipients of the 2025 Quality Awards will be recognized during the Elevating Excellence Awards Ceremony at Delivering Solutions 25, AHCA/NCAL’s Convention & Expo, in Las Vegas, Nevada, in October.
Scan the QR code to view the list of all the 2025 Quality Award recipients is available on the AHCA/NCAL
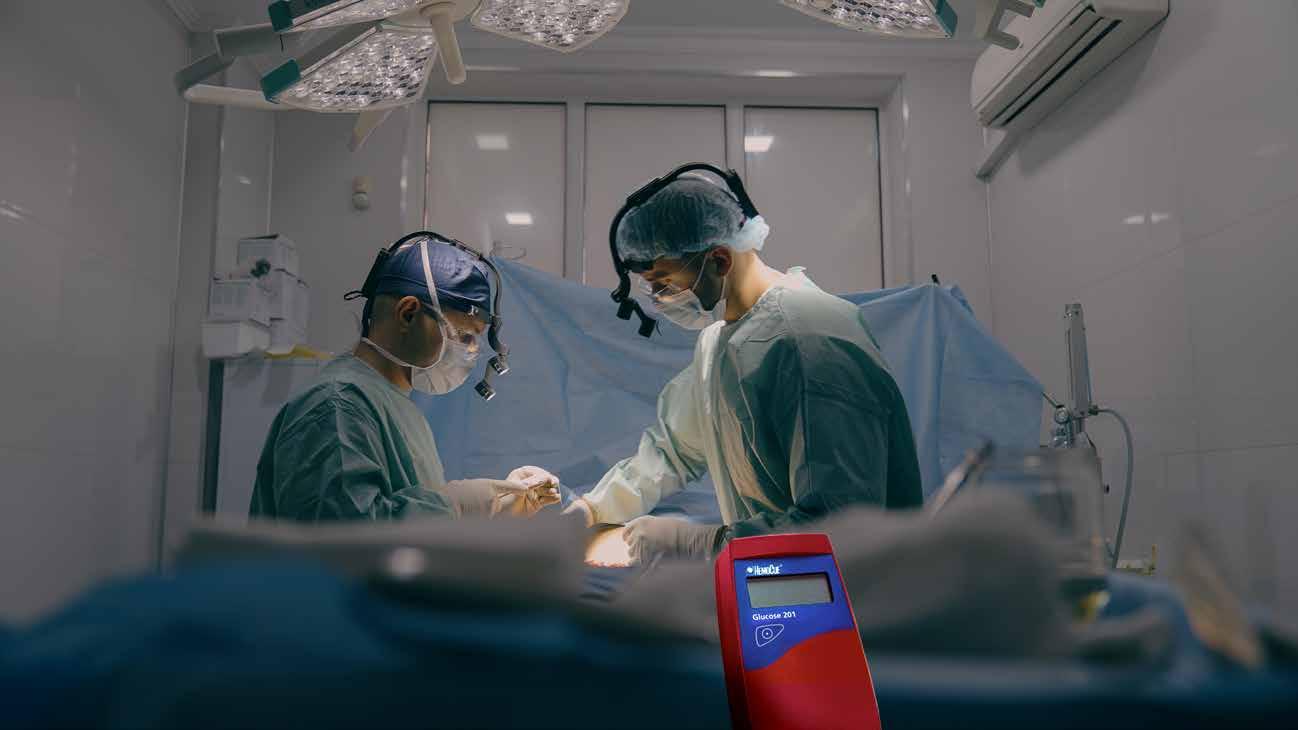
Infection control
for ambulatory surgery centers
The HemoCue® Glucose 201 System allows for blood collection separate from the analyzer, reducing exposure for bloodborne pathogens and risk of cross contamination
Addressing Staffing Shortages in ASCs
Burnout and changing workforce dynamics put pressure on ambulatory surgery centers.
By Pete Mercer
 Staffing shortages are one of the most prevalent challenges facing the healthcare industry, and ambulatory surgery centers are no exception. As ASCs continue to grow in popularity due to convenience and cost-effectiveness, so does the demand for skilled teams to take care of patients. Healthcare can be sort of a revolving door when it comes to employees, and it’s not easy to keep facilities staffed in those kinds of conditions.
Repertoire Magazine sat down with Erin Boers, VP, HR Services at MedHQ, and Mayte Rechani, Executive Director at MedHQ, to discuss navigating staffing challenges for ASCs, the toll of burnout in a healthcare environment and how to improve employee engagement. MedHQ is a provider of healthcare advisory and administrative solutions, including HR and staffing, to ASCs and other organization types.
Workforce dynamics in ASCs
Like every other healthcare setting, there have been numerous shifts for the ASC workforce in recent years. The world has changed so much since 2020, especially for healthcare workers. The pandemic alone created a seismic change in how the public viewed the healthcare industry, both positive and negative, and the fallout from that has completely transformed the landscape of the industry.
One of the most significant components of that fallout is the staffing shortage. The National
Library of Medicine published a study showing that more than one-third of nurses will reach retirement age in the next 10 to 15 years, while the National Council of State Boards of Nursing reported in 2023 that 100,000 nurses left the profession altogether during the pandemic due to stress, burnout, and retirement. There are very serious ramifications for these shifts, creating vacuums in patient care settings that are either being left open or filled by overworked employees, which further perpetuates the
issue. This also extends to ambulatory surgery centers. As more and more patients are migrating towards ASCs for safe, efficient and cost-effective care, the need for more staff becomes greater. “They are busier than ever, increasing the need for staff,” Rechani said. “Surgeons are transitioning their surgeries from the acute care setting to ASCs, where they have more autonomy and can help reduce costs.”
With the influx of new patients, employees at ASCs are seeking more stability within the
ASC system. While the traditional challenges of working in a hospital are largely absent in this environment, ASCs still come with their own issues. “There is an increased demand for flexibility,” Boers said. “Employees are seeking more predictable schedules, better work-life balance, and flexible benefits. There’s also a noticeable shortage of skilled nurses and surgical techs, driving up competition with hospitals and other healthcare facilities.”
Navigating burnout in an outpatient setting
Burnout is pervasive, no matter what kind of setting employees are working in. Burnout in a traditional hospital setting received lots of attention and recognition as a problem during the height of the pandemic, but healthcare workers have experienced burnout for years. This is what leads to employees leaving the healthcare industry in droves, further perpetuating the staffing shortages that are creating so many of these problems.
That’s no different for outpatient clinics. Staff at ASCs experience burnout in a different way, according to Rechani. “While they may not work weekends and normal workday schedules, they rarely have any time off due to the ASC staffing shortages. ASCs are looking at different alternatives to have shifts covered, but if they are not utilizing a good agency partner, they will not be covered. In these cases, procedures may be cancelled at the last minute.”
Even though the ASC setting allows for employees to work regular hours, these facilities are designed to be lean operations with high standards of performance
in a fast-paced environment. An environment like this is a perfect breeding ground for burnout, so it’s important to understand how to actively fight against the things that contribute to fatigue.
“At MedHQ, we work with ASC leadership to implement proactive measures, including regulator engagement and check-ins, mental health and EAP programs, workload management tools, and leadership training focused on empathetic management,” Boers said.
The importance of a healthy culture
Company culture plays a significant role in the retention of the
heart behind the work. This gives the incoming (or even existing) employees something concrete that they can grab onto.
“While ASCs’ branding is paramount to attracting top talent, ASCs are not always clear with their messaging,” Rechani said. “What exactly are they offering new talent? What is the culture at the ASC? Younger talent right now is looking for any employer to be a ‘good fit’ for them – they’re prioritizing their mental health over an easy work schedule, while the more seasoned talent is prioritizing work schedules and mental health.”
“ There is an increased demand for flexibility. Employees are seeking more predictable schedules, better work-life balance, and flexible benefits. There’s also a noticeable shortage of skilled nurses and surgical techs, driving up competition with hospitals and other healthcare facilities.”
workforce, keeping them engaged with their work and the mission and vision of the company. When the culture is aligned with the values of the organization, it’s easier to engage the team with their work. This is essential, because the comfort and safety of the patient is at stake. Engaged employees mean that patients are taken care of.
Part of the challenge is creating an attractive environment to new employees. Defining the culture, as well as the mission and values of the organization, helps to improve the messaging and showcase what drives the
It’s all about telling the story of why the organization was started, where it’s come from, and where it’s going in the future. Tapping into that story gives employees something to believe in for the important work that they’re doing.
Boers said, “Employer branding and culture are critical in today’s talent market. ASCs have a compelling story to tell: high-quality care, a focused specialty setting, less bureaucracy, and better work-life balance than many hospital environments. However, these advantages must be clearly communicated. A strong brand and culture not only attract talent – they help retain it.”
Supply Chain Leader Spotlight
Jason Moulding, Chief Supply Chain Officer, MultiCare
 Jason Moulding’s journey into healthcare supply chain was shaped by his family’s background – his father, a military dentist, and his mother, a nurse. While attending college, he needed a job and chose a position in medical records at a nearby hospital. This initial step kept him in the field, eventually leading to a role in the operating room at Overlake Hospital in Bellevue, Washington.
His strong negotiation skills soon caught the attention of the director of materials management, earning him a new role in contract management, a pivotal shift that uncovered his passion for analytics. Moulding continued advancing through positions at Overlake, Providence Health & Services, and later MultiCare Health System, where he has spent nearly nine years.
Although he considered other industries after earning his MBA, he remained in healthcare supply chain, saying, “I felt that healthcare was my calling.”
On what he’s keeping an eye on as a supply chain leader
Moulding: Supply Chain postCOVID is so much more complex. The biggest challenge I would say is there is no single overriding challenge. Tariffs are obviously an issue for now, and then the downstream effects not just from a pricing perspective, but what is that going to do to the global supply chain? Will there

be shifts in manufacturing? Shifts in manufacturing countries? Will manufacturers exit the market?
A supply chain leader of today needs to have visibility a lot further upstream than ever before. Risk and resiliency are at the forefront, and it has been that way since COVID. We haven’t let our foot off the gas. Each year brings increasing complexity, with more factors that supply chain professionals must stay fluent in and closely monitor.
The impacts of global supply disruptions are happening more often every year – whether through natural disasters, geopolitical events, shifts in manufacturing, etc. Having a macro lens and then discerning how disruptions or opportunities impact your organization will keep supply chain relevant and essential.
On the skills and intangibles needed from supply chain teams
Moulding: Analytics/insights is a crucial skill, and I really like the business background versus maybe the purely healthcarefocused one. Having accounting knowledge and a finance background is part of that new language or skill set for today’s supply chain landscape. Beyond technical expertise, I value intellectual curiosity and a drive to be curious. Our CEO talks about three key components a leader or individual contributor needs to have: critical thinking, integrative thinking, and situational awareness. Integrative thinking involves connecting supply chain operations with clinical, financial, and operational stakeholders across both acute and non-acute sites. Situational awareness means understanding global trends and identifying what’s most relevant. Critical thinking, meanwhile, focuses on pinpointing priorities and addressing the most pressing challenges. These intangible qualities are always top of mind for me.
On being a go-to source for support and help
Moulding: Our Supply Chain vision statement is: Partnering to deliver the highest value to support the
Jason Moulding
vision of MultiCare. One of the achievements I’m most proud of in support of this vision is the transformation of our analytics division within MHS.
Since assuming responsibility for the platform in 2022, we’ve made significant progress. Initially, each MHS division preferred to manage its own analytics. However, through collaboration and by embedding our experts within business units, we’ve built strong partnerships. Since then, we have successfully insourced majority of analytics under our platform. Today, stakeholders actively seek our support, recognizing the value we bring.
Our analytics platform has evolved into a powerful, trusted tool across the health system. As owners and managers of the enterprise data warehouse (EDW), we integrate disparate data sources – including Epic, Workday, and various clinical programs – into dynamic Power BI dashboards. These dashboards, coupled with our analysts, serve decision-makers at every level, from the boardroom to individual leaders running daily operations.
Our dashboards operate at multiple levels, offering a macro view of system-wide procedures while diving deep into encounterlevel insights. We overlay cost data with reimbursement figures, payer
STRATEGIC SUPPLIER
mix, and essential quality metrics – readmission rates, surgical site infections, and more. This allows us to pinpoint key relationships: Does a particular intervention reduce length of stay? Does it accelerate patient transition to home?
With four to five years of datadriven decision-making behind us, we continue to refine our approach. The next phase is ensuring we engage the right stakeholders, helping them navigate trade-offs while integrating more clinical insights. The platform is a critical tool – one among many – that drive smarter healthcare strategies that ultimately improve the patient care to the communities we serve.
Join us for the Winter Summit December 2 – 4, 2025 at the Sheraton Music City in Nashville!
The 2025 NDC Winter Strategic Supplier Summit is the ultimate platform for suppliers to engage with the NDC Sales Team, exchange key insights, and develop strategies for the upcoming year. This unique event was designed specifically to foster collaboration, drive growth, and strengthen partnerships.
▪ One-on-One Strategy Meetings
▪ Exclusive Executive Leadership Insights
▪ Elite Networking Dinner Scan the QR code for additional details.
Supply Chain Leader Spotlight
Rachel Cunningham, Director of Operational Excellence, Piedmont Healthcare
 Supply chain is slightly removed from patient care. Because of this, Rachel Cunningham, Director of Operational Excellence, Piedmont Healthcare, wants to connect her team to the person or people at the end of all the decisions they make.
“I came up in manufacturing, transportation, and then moved into healthcare,” she said. “So that’s really a big difference between supply chain in healthcare and supply chain anywhere else -- there’s a human being at the end of all this.”
Working in the automotive industry, it was going to be annoying if supply chain didn’t get an engine out on time. But no one’s life was threatened in that scenario.
Healthcare is different. “So, I think that’s really the balance or the philosophy that my team has, is just keeping that human being at the center of everything that we do,” she said. “Understanding that not only the human being that benefits from making sure that we have the right price in the system and being charged the right price, but also the human being that has to clean up after our messes when we don’t do something right.”
Cunningham uses the Bullwhip Effect as an example. The Bullwhip Effect states that every small decision makes a larger impact the further down the line it goes. Cunningham and her team know that the people doing the work on
the ground -- those seeing patients, refilling pars, etc. -- will have to pay the biggest consequence when something goes wrong. “That’s our philosophy around keeping the cost efficiency and quality in tandem,” she said. “Don’t let perfection get in the way of progress, but keep in mind that somebody else is cleaning up your mistakes.”

Operational effectiveness at Piedmont Healthcare encompasses things like analytics work and new technology.
Cunningham and her team are the bridge between supply chain data and action within supply chain. She leads the business/ systems analytics team, which handles all of Piedmont’s ERP integration and all the vendor information. She also manages continuous improvement projects and any other projects that come our way. “So, any new fun stuff we want to roll out, that tends to roll through me.”
On the most pressing challenges in supply chain
Cunningham: First, the number of stakeholders that are involved in just about every decision we make now has grown. Silos are a luxury of the past. We can’t afford them anymore. Every decision must be made in tandem with our clinical teams and our finance team.
Second, we’ve come to understand that just judging by price isn’t a fair comparison of how we are doing anymore. We’re really focused on total cost of ownership, or a cost-to-serve model. Just because we have a price increase doesn’t necessarily mean it’s a bad thing. It may increase revenue. A big challenge has been seeing that full picture and making sure that we’re encompassing everybody that needs to be in all of those discussions.
The final challenge is supply chain continuity or just making sure that we have the right products in the right place, especially around all the challenges that we’ve had since COVID. We’re luckier than most. We self-distribute, which is a huge benefit to us. We have a distribution center where we’re able to keep a lot of
Rachel Cunningham
our commodity items so we can mitigate quite a bit of risk. But I think every health system is in the same boat of all going after the same products at the same time, and when they go on a shortage or when there’s a recall, we’re all still looking for the same products at the same time.
On the value of good, clean data
Cunningham: One of the big initiatives for our systems analytics team is around our data cleanup and match exceptions. We’ve put a lot of work in the last few years into data cleansing and
data integrity. One of the mottos that we keep at Piedmont is “right product, right place, right time at the right price,” because that is what supply chain is all about.
We’ve done a ton of work around this in the last couple of years, and we were able to improve our match exception rate. When you’re going through the system, if something has to be touched by human hands because the automation didn’t work, that’s a key way to think about a match exception. For example, if your invoice price didn’t match, or the part number didn’t match. Something made it so someone had
to take it out of its automated process and actually touch it.
We took our match exception rate number from 20% of our overall purchase orders to less than 3%. I’m very proud of the team for that. They’ve put in a lot of hard work, and we’ve been able to maintain that for over 18 months at this part.
That’s coupled with astronomical growth. Piedmont has doubled in size twice in the time that I have worked here. So that’s been a really big thing for us to be able to do that amount of data cleansing on top of day-to-day maintenance.



by

Essential to Outcomes
Scales are a critical yet often overlooked factor in patient safety.
 Scales are often underestimated as essential medical equipment because they are simple tools used briefly during patient exams. “Most patient scales aren’t complex; therefore they are often overlooked for accuracy, advancements in technology and overall ease of use,” Befour explained in an interview with Repertoire Magazine .
Because scales are used for only a short part of an exam, they are sometimes disregarded when considering equipment needs, accuracy, or maintenance. But inaccurate measurements can raise serious concerns and lead to broader clinical issues.
Revenue opportunities and technology
Key opportunities for reps include scale service, repair, and education on new technologies. Calibration should be checked regularly, and routine inspections may reveal when a scale needs servicing or replacement. Befour noted its Opti-Height line increases accuracy and decreases the time it takes to capture weight and height, offering a meaningful upgrade to standard models. Clinicians often rely on reps to educate them on these innovations and how they can improve care.
Evaluating scale accuracy
Every Befour scale leaves the factory fully calibrated with a certificate of calibration. While in theory they shouldn’t need

recalibration, most medical facilities follow their own protocols, testing accuracy and recalibrating annually or more often depending on use. For example, if scales are frequently moved between rooms and risk damage, more frequent evaluations are recommended.
Impact on clinical outcomes
Outdated or inaccurate scales can significantly affect clinical outcomes. Weight is central to medication dosing, making accuracy especially critical for pediatric patients. An incorrect measurement in infants or neonates can result in miscalculated dosages with potentially severe consequences. Accurate weights are also essential in monitoring and
treating obesity, anorexia, malnutrition, growth issues, cancers, and mental health conditions.
“Inaccurate weight calculations, either by an uncalibrated scale or a broken scale, can have a negative effect on many health-related issues,” Befour warned.
When to consider an upgrade
Scales are visible fixtures in exam rooms and can influence how patients perceive a clinic. Outdated equipment – such as faded plastic models or mechanical balance beams – may send the wrong message. Compared to more expensive diagnostic tools, scales are relatively inexpensive to replace, while offering improvements in both aesthetics and patient care.
Time and efficiency also matter. Clinicians need to capture accurate weights quickly. Befour suggests considering these questions when evaluating scales:
` Does the scale measure within +/-0.1 lb accuracy?
` Does it incorporate digital technology to reduce human error?
` Does it have MotionLock Technology for capturing accurate weights of moving infants or patients with Parkinson’s?
These features can make a real difference in accuracy, efficiency, and patient confidence. Ultimately, while scales may seem like minor tools in the exam room, their accuracy and reliability play an outsized role in both patient safety and clinical outcomes. Regular evaluation, proper maintenance, and consideration of technological advancements can ensure they continue to serve as a vital part of quality patient care.




Befour’s extensive line of Wheelchair Scales is expanding!
BETTER VALUE
BETTER ADA OPTIONS
BETTER PORTABILITY
BETTER LEAD TIMES
Need a scale that is made in the USA and offers features only found in Befour models? Let’s talk!
Chose from our tried and trusted legacy models or one of our new additions! The newly launched wall mount scale folds away when not in use. Or, our compact and portable ADA compliant wheelchair scale and retrofit kit might be the perfect choice!
Befour’s scale options offer American-Made dependability starting with the design and engineering, down to the components and manufacturing. Proven. Trusted. Reliable – nothing is BETTER.



Seeing the Exam Room with New Eyes
Why the exam room is a dynamic ecosystem, and how to spot hidden opportunities.
 For distributor reps, the exam room often holds untapped potential, not just in terms of sales, but in creating safer, more efficient environments for patients and providers. Roy Reese, Vice President of Sales for the Western U.S. at Graham-Field, believes the key lies in changing the way reps view this familiar space.
“Too often, we walk past opportunities because we’re not looking closely enough,” Reese said.
One of the most overlooked categories is equipment repair and replacement parts. “Our job isn’t simply selling products. It’s about being consultants, being good finders. When equipment isn’t working properly, it impacts compliance, safety, and ultimately patient care.”
Reese recommends that reps approach every exam room visit with a structured plan. He
suggests carrying an equipment checklist to review what’s already in the room, then asking probing questions: What’s broken? What could be improved?
The process doesn’t end with a visual scan. He advises taking detailed notes, including make and model numbers, serial numbers, and even photos of worn or broken items. “Documentation is critical,” he emphasized. “It helps you build credibility and provide solutions, not just products.”
One common disconnect Reese sees is the tendency for providers to “patch” problems rather than fix them. Torn exam tables covered with tape may seem harmless, but they pose real risks of contamination. Likewise, broken or missing wheelchairs compromise patient safety but are sometimes overlooked. “It’s like putting a bandage on a wound without treating the infection,” Reese explained.
Instead of viewing the exam room as a static space filled with furniture and tools, Reese encourages reps to see it as a dynamic ecosystem. It is a place that directly shapes patient experiences and staff performance. Foundational items such as exam tables, patient seating, stools, and specialty chairs may not be glamorous, but they are central to comfort, ergonomics, and compliance.
Clinicians and practice managers, Reese noted, are often motivated to upgrade equipment when they understand how improvements affect outcomes. That includes smoother workflows, safer environments, and more positive patient reviews. “When they see the benefit of compliance tied directly to staff and patient satisfaction, that’s when the decision to invest becomes easy,” he said.
For reps hoping to tap into those decision-making moments, Reese’s advice is straightforward: be mindful, document everything, and follow through.
“Don’t just point out what’s broken,” he said. “Connect the dots between the problem and the solution, and then ask for the business.”
By reframing the exam room as more than four walls and a table, reps can uncover both sales opportunities and ways to support better care. In Reese’s view, that is the real win-win.
HIDA Emerging Leaders
Shaping the future of supply chain.

By Kathryn DiBitetto, Vice President, Government Affairs
 Healthcare distribution is not just a career: it’s a calling. The professionals who keep the medical supply chain running ensure that when care is needed, the right products are in the right place at the right time. It is a purpose-driven profession, and for students seeking meaningful careers, it offers a pathway to make an impact on patients’ lives.
That is why HIDA is excited to announce that applications are now open for the 2026 Medical Supply Chain Emerging Leaders: Campus Edition Program. This initiative identifies and supports college students who are passionate about healthcare distribution, logistics, and supply chain management – and who want to be part of shaping the future of this critical industry.
Building on momentum
The 2024 and 2025 cohorts included students from leading universities across the country, many of whom brought international experience, unique academic backgrounds, and deeply personal reasons for pursuing careers in healthcare supply chain.
Past participants have praised the program for the impact it has had on their career paths: ` “My life changed drastically when I began experiencing severe heart issues that required immediate surgery. Due to delays in the healthcare system, I had to wait six months for the procedure. This experience shifted my perspective and ignited my passion for entering the medical field.”
– Student from North Carolina
A&T University
` “I consider healthcare to be one of the most important supply chain fields to exist presently. The consumers are patients, not customers. If a particular medical product is not delivered to the
hospital on time, the patient will have to suffer for it, especially with their lives on the line.” – Student from Wayne State University
` “The seamless care I received as a child relied on efficient supply chain management to ensure that patients like me received the right care at the right time.” – Student from Western Michigan University
Looking ahead to 2026
This year, HIDA continues its outreach to a greater number of schools and more diverse group of students, expanding the reach of our workforce development efforts and inspiring the next generation of leaders.
These students will attend HIDA’s 2026 MedSupplyChain Conference, in Dallas. Emerging Leaders will gain access to exclusive panel discussions and invaluable networking with senior executives shaping the industry. We encourage you to seek out and connect with these future leaders.
If you know a promising student with a passion for healthcare distribution, encourage them to apply. Applications for the 2026 program are open through October 31, 2025, at jobs.hida.org.
MicroCare Medical™ Spec Clean™ Pre-Treatment Gel Spray
The Spec Clean™ Pre-Treatment Gel Spray from MicroCare Medical™ is a ready-to-use neutral pH gel spray for medical instruments that rinses off easily, replacing the need for messy liquid soak pans.
Spec Clean™ Pre-Treatment Gel Spray is formulated with biodegradable surfactants and wetting agents and is designed for pre-treating surgical instruments and medical devices to improve cleaning effectiveness and efficiency during subsequent cleaning steps.
In healthcare settings, proper instrument cleaning is required before high-level disinfection and sterilization, as inorganic and organic materials that remain on the device surfaces can interfere with the efficacy of the sterilization process.
With the use of Spec Clean™ Pre-Treatment Gel Spray, surfactants maintain moisture and protect contaminated instruments during transport for up to 72 hours.
Safe, effective instrument disinfection
Spec Clean™ Pre-Treatment Gel Spray delivers a simple, effective solution for sterile processing pros for use in even the most challenging orthopedic, neurospinal and gastrointestinal cases. If soiled materials from surgical procedures dry or bake
onto medical instruments, the removal process is more difficult, and disinfection becomes less effective. Surgical instruments therefore must be presoaked or rinsed prior to sterilization.
The Spec Clean ™ PreTreatment Gel Spray specifically features Humectant gel, helping to prevent soils from drying and hardening after instrument use. The Pre-Treatment Gel

Spray leaves no sticky residue behind on carts or trays, rinsing off easily during cleaning.
Confidence in every clean
Spec Clean™ Pre-Treatment Gel Spray Bag-on-valve technology keeps soils moist by administering broader spray coverage with more controlled delivery. The green-tinted gel foam allows for visible confirmation of coverage and compliance, providing confidence in every clean.
The Pre-Treatment Gel Spray is ideal for use in Central Sterile instrument processing areas in labor & delivery rooms, emergency departments, off-site healthcare facilities and more for spot treatment of heavy residual soils, or for when high caseloads lead to delays.
Neutral and non-corrosive
Spec Clean™ Pre-Treatment Gel Spray, with a neutral pH of 7.0-8.0, is non-corrosive, with no fragrance added, protecting delicate surfaces from corrosion during prolonged hold times. The goal of pre-treating medical and surgical instruments is to preserve the value of the instruments being reprocessed.
The Pre-Treatment Gel Spray is compatible with a wide range of materials including stainless steel, aluminum, plastics, glass and delicate ophthalmic instruments.
Sources: www.cdc.gov/infection-control/hcp/disinfection-sterilization/cleaning.html#:~:text=Cleaning%20is%20the%20removal%20of,process%20less%20effective%20or%20ineffective. www.cdc.gov/infection-control/hcp/disinfection-sterilization/sterilizing-practices.html




Stops dried-on soils that slow down cleaning. Fulfills AAMI and AORN Recommendations.
• Ready to use, neutral pH gel with full coverage that rinses clean -- no messy soak pans
• Perfect for busy ORs, L&D, ER, and clinics
• Distributors value strong reorder potential; clinicians trust proven results
• Made in the USA for quality and availability
Clean™ Pre-Treatment Gel Spray locks in moisture and protects instruments for up to 72 hours!
MTMC Expands Supplier Showcase Program
Hands-on events bring products and people together.

MTMC, an outsourced medical and supply sales firm, expanded its Supplier Showcase Program earlier this year, adding 12 events across the country for suppliers, distributors, and IDN decision makers under one roof for a trade show style event. This showcase is designed by MTMC to be impactful for attendees, allowing medical suppliers to put on live product demonstrations and create opportunities for direct dialogue with health system and supply chain leaders.
Mike McCabe, Vice President of Sales for MTMC, said, “The Supplier Showcase Program was hatched out of a necessity to get our distribution channel partners together in front of our supplier partners, in lieu of a sales meeting. A lot of our distribution partners were cutting back on sales meetings anyway, so we wanted to put something together that would allow them to see a showcase of current and new product offerings.”
This program is only in its second year, but McCabe said that MTMC’s decision to expand the program for 2025 was based on the success of six showcases in 2024. “Last year was really
successful for us in a select group of cities. This year, we took it to a new level with a package of 12 showcases in major markets throughout the country.”
These showcases are immersive events where supply chain customers can see and interact with products like EKGs, defibrillators, or exam tables that they could put into new clinic setups. Additionally, each event will have interactive sessions with distribution teams, allowing suppliers and distributors to make meaningful connections with each other. The showcase also allows for supply chain decision makers from IDNs across the country to come and take
a look at some of the products they have already purchased, as well as check out any new products that they could potentially incorporate into their workflows.
With supplier partners like BD, Baxter, Ansell, BioNix, Massimo, Graham Medical, ZOLL and more, McCabe is excited about the potential that these showcases hold for everyone in attendance. He said, “There are a lot of opportunities being developed at the ground level at these local showcases –sometimes even more so than they might get at a national trade show, which are so large in scope. This is where you get true opportunities being generated.”


Know Your Risk: Breast Cancer
Breast Cancer Awareness Month is recognized each October.
 When talking about women’s health, one topic continually comes up – breast cancer – and for good reason. With increased awareness, physicians have been finding and treating breast cancer earlier through improved screening, according to the American Cancer Society. Breast cancer death rates have been decreasing steadily since 1989, for an overall decline of 44% through 2022.

Breast cancer is the most common cancer for women in the United States (besides skin cancers), accounting for nearly 30%, or 1 in 3, of all new female cancers each year, according to the American Cancer Society.
Breast cancer is a disease in which cells in the breast grow out of control, according to the Centers for Disease Control and Prevention (CDC), and mainly occurs in middle-aged and older women, with a median age of 62 at diagnosis. Most breast cancers
begin in the ducts (tubes that carry milk) and the lobules (glands that produce milk) of the breast.
“One of the most common misconceptions is that all breast cancers are the same. In reality, breast cancer varies significantly from person to person,” said Caroline Koffke, RN, BSN, OCN, Director, Educational and Healthcare Provider Programs at Living Beyond Breast Cancer (LBBC). “Subtype, tumor biology, and specific biomarkers can make each diagnosis unique, leading to very different treatment plans.”
Living Beyond Breast Cancer is a national nonprofit organization that connects people affected by breast cancer with expert information and a community. Through
recognize that no two journeys are identical,” said Koffke.
Understanding modifiable risk factors
Advances in technology including 3D mammography, breast MRI, AI-assisted interpretation and other emerging technologies have improved breast cancer detection rates and accuracy. Early diagnosis significantly improves prognosis and long-term survival rates, according to the National Library of Medicine.
“By identifying more cancers earlier, these innovations are giving patients better outcomes and saving lives,” said Koffke.
There is no sure way to prevent breast cancer, but there
“ One of the most common misconceptions is that all breast cancers are the same. In reality, breast cancer varies significantly from person to person. Subtype, tumor biology, and specific biomarkers can make each diagnosis unique, leading to very different treatment plans.”
practical resources, real stories, clear information and meaningful connections, the organization helps guide people through diagnosis, treatment and life beyond breast cancer.
There are many different types of breast cancer, and not all types are the same. Each type has its own features, characteristics and health considerations.
“While it’s natural for people to seek support from someone they know who has experienced breast cancer, it’s important to
are lifestyle changes that women (and men) can make that may lower their risk, according to The American Cancer Society.
Risk factors for breast cancer fall into two categories: non-modifiable and modifiable. Non-modifiable risk factors include increasing age, personal or family history of breast cancer, and reproductive history – such as age at first menstruation or menopause, according to Koffke.
“Non-modifiable risk factors cannot be changed, but they may
warrant earlier or more frequent screening and proactive conversations with a healthcare provider,” said Koffke. “Modifiable risk factors – like maintaining a healthy weight, regular exercise, limiting alcohol, and avoiding smoking – can be addressed to help reduce risk.”
Yet, 1 in 2 women don’t get their annual breast screenings, missing a crucial opportunity to diagnose and treat the disease early. If diagnosed early, breast cancer patients have a significantly increased survival rate for breast cancer then when it is found in its more advanced stages.
seen a growing appetite among patients for detailed, accurate information to help them make informed decisions.”
Advocacy and awareness
Advocacy and policy are key to shaping the screening and treatment guidelines for breast cancer care, as well as care access and disease prevention, according to Koffke.
“Many patients now actively participate in advocacy, research panels and clinical trials. At the same time, breast cancer care has become more complex, making reliable information more essential
Breast Cancer Awareness Month is a health campaign recognized each October to promote early screening, support those diagnosed with breast cancer and raise money for ongoing disease research.
“Living Beyond Breast Cancer participated in the Your Attention Please campaign, which offers tools to help people calculate their risk and prepare for conversations with their providers,” said Koffke.
The Your Attention Please campaign highlighted that everyone has a different breast cancer risk, and that anyone 40 and older should make annual screenings a priority.
For women under age 40, the campaign encourages individuals to understand their risk and decide whether to start their own screening earlier.
“Over the past decade, there has been greater understanding of risk factors, early detection and the importance of personalized care,” said Koffke. “We’ve
than ever,” said Koffke. “Increased awareness has also fueled greater philanthropic and corporate support, particularly during Breast Cancer Awareness Month.”
Breast Cancer Awareness
Month is a health campaign recognized each October to promote early screening, support those diagnosed with breast cancer and raise money for ongoing disease research.
Public campaigns from a variety of organizations focused on breast cancer have reduced the stigma around the disease and began crucial conversations around breast health, especially in families with a history of the disease.
“Digital platforms have also transformed how people connect – closed Facebook Groups, for
example, provide safe, moderated spaces where people share practical tips, emotional support, and encouragement,” said Koffke.
Ongoing research into breast cancer treatment has also been a significant aspect of breast cancer advocacy and policy advancement.
“The pace of research and innovation is remarkable. Each year at major conferences like the American Society of Clinical Oncology (ASCO) and the San Antonio Breast Cancer Symposium (SABCS), we see new treatments, imaging tools and prevention strategies coming to light,” said Koffke.
Koffke says that people across the nation can help get involved in Breast Cancer Awareness Month by donating, volunteering, sharing resources, or advocating for legislation that impacts the breast cancer community.
Living Beyond Breast Cancer’s 2025 Breast Cancer awareness campaign is centered around ‘connection through stories,’ specifically with the My Why campaign that invites people living with breast cancer, caregivers, healthcare providers and advocates to share the reasons they preserve, care, give and advocate.
Living Beyond Breast Cancer also shares clear and accessible information about breast health and risk factors, and the ability to donate, volunteer and raise awareness throughout the year.
Koffke expresses that “breakthroughs in research, paired with a more engaged and informed patient community, give us tremendous hope for a future with better outcomes and more personalized care for everyone diagnosed with breast cancer.”




Industry News
Thermo Fisher Scientific opens manufacturing center of excellence site in North Carolina
Thermo Fisher Scientific Inc. announced the grand opening of its innovative manufacturing center of excellence facility in Mebane, N.C. The new 375,000-square-foot carbon neutral site will be capable of producing at least 40 million laboratory pipette tips per week, helping to ensure that life-saving medicines and therapies continue to be developed and produced in the U.S. for decades to come.
Pipette tips are critical tools for research and diagnostics, enabling precise liquid handling in high-volume applications such as disease studies and diagnostic testing. Thermo Fisher manufactures its tips with high-quality materials and strict quality controls to ensure accuracy, reduce contamination, and deliver consistent performance. The new Mebane site is built for efficiency, with advanced automation that produces 96 tips every 12 seconds and 5,000 finished assemblies per hour. Designed for seamless operations, it also features automated packaging and shipping to meet growing customer demand.
The new Mebane site has already hired 40 people and is expected to add 50 jobs in manufacturing, engineering and business operations. Thermo Fisher currently employs approximately 7,800 colleagues across 13 sites
in N.C., including a center of excellence for laboratory equipment in Asheville, three life sciences [and] manufacturing sites in Durham, pharmaceutical manufacturing sites in Greenville and High Point, and a Raleigh distribution center.
BD hosts inaugural ‘Patient Day’ to celebrate purpose and impact of patient journeys
BD proudly hosted its firstever “Patient Day” event at its Advanced Patient Monitoring headquarters in Irvine, Calif. recently, bringing together patients and BD associates in a powerful celebration of purpose, innovation and community.
Themed “Our Patients, Our Purpose,” the event offered a deeply moving experience for all attendees. Patients shared their personal stories in live panels, highlighting how BD’s technologies have impacted their lives.
Associates from across BD APM participated in the day’s activities. In a particularly moving moment, team members from BD’s manufacturing sites joined the event in person, meeting face-to-face with patients whose lives were directly impacted by the products they helped create. This powerful exchange underscored the real-world significance of BD associates’ work and the deep connection between innovation and patient outcomes.
The day featured a giving-back initiative supporting Children’s
Hospital of Orange County (CHOC). Over 100 care packages were assembled by associates at the Irvine campus, filled with items for pediatric patients. The activity reflected BD’s ongoing commitment to supporting local communities.
QuidelOrtho welcomes Erich Wolff as Executive Vice President, Strategy & Corporate Development
QuidelOrtho Corporation welcomes Erich Wolff as Executive Vice President, Strategy & Corporate Development. In this role, Mr. Wolff will report directly to President and Chief Executive Officer Brian Blaser, and he will lead the Company’s enterprise strategy, business development, government affairs and portfolio management functions.
Mr. Wolff brings over two decades of leadership experience in strategy, M&A and business development across the healthcare, diagnostics, and MedTech sectors. Most recently, he served as Buyouts Lead for MedTech and Life Sciences Tools & Diagnostics at Partners Group, a global private equity firm with $174 billion in assets under management. Prior to that, he held senior leadership roles at BD and Medtronic, where he led transformational initiatives spanning corporate strategy, investment planning and inorganic growth.
KNOW THE DEALS.
WIN THE SALE.
Midmark is offering exclusive savings across top-performing product lines. Complete the room by selling the entire point of care ecosystem to unlock bigger savings and deliver more value for your customers.
Point of Care Exam Room Promotion
Customers get $950 Back or a Diagnostic Set
Scan for details.
Examination Chair Trade-In Promotion
Rebates up to $400 + a Bonus $150 with delivery and trade-in removal services.
Scan for details.
Sterilizer Trade-In Promotion
Customers save up to $500 when they trade in a sterilizer and purchase an eligible Midmark model.
Scan for details.





Digital Vital Signs Device Promotion
Customers get $300 back or a Free BP Cuff Kit value of $260 with eligible digital vital signs purchases.
Scan for details.

Sterilizer Maintenance Kit Promotion
$225 Value – Customers get a free maintenance kit when they register their new Midmark sterilizer.
Scan for details.



Spotlight on Welch Allyn Solutions for Outpatient Care
Baxter has more than 100 years of innovation, 268,000 customers nationwide, and 100 configurable Welch Allyn products.
Redefining Healthcare Delivery
< Scan To View Our Current Promotions