The anatomy of a clinical trial
Written by: Anna Waters
Media
contact: Yvonne Taunton
A clinical trial is a special kind of research approach that physicians and scientists use to study the effects of a new treatment in order to compare it to an existing treatment. If the new treatment proves to be safer or more effective than the current standard treatment, it can become the new standard of care for treating people with cancer
Clinical trials serve as the bridge between research and patient care. Learn more about clinical trials, who can participate and why they play a vital role in cancer research.
Clinical trials represent the culmination of a long, rigorous process by which physicians and researchers translate promising scientific findings from the laboratory into medical practice so those findings can become new treatments for a disease.
As researchers ask questions about how cancers develop in the human body, they can use the results of their research to develop potential treatments for cancer that can challenge the bodily processes upon which cancers depend. These potential treatments are then tested in clinical trials where they are offered to cancer patients. Clinical trials are a vital
component of this “bench-to-bedside” model that defines the field of translational science, representing the bridge between scientific research and patient care
Barry Sleckman, M.D , Ph D , director of the O’Neal Comprehensive Cancer Center at the University of Alabama at Birmingham, says its NCI designation and diverse clinical trials portfolio differentiate the Cancer Center from other cancer care providers in the state.
“Today, many patients on clinical trials are experiencing remarkable, disease-altering effects on cancers that were uniformly lethal just yesterday,” Sleckman said “For this reason, offering cancer patients clinical trial opportunities is really the standard of care for cancer.”
How do clinical trials work?
The treatments that are tested in clinical trials must be studied carefully and evaluated in large, diverse groups of people over long periods of time before they can be officially offered to the public as the standard of care But if a new treatment does prove to be effective, trial participants could be among the first to benefit from it, especially if their cancer is not responding to existing treatments.
Doctors decide whether a patient is eligible for a clinical trial depending on the patient’s specific kind of cancer, current condition and individual needs If doctors believe a patient might benefit from a new treatment offered by a clinical trial, they will give the patient the choice to enroll.
“If you are diagnosed with cancer and aren’t sure what to do next, it’s OK,” Sleckman said. “You don’t have to know exactly what to do. You need to know where to start At the NCI-designated O’Neal Comprehensive Cancer Center at UAB, you have access to the best multidisciplinary cancer care and the latest cutting-edge trials ”
Patients participating in a clinical trial receive the new, experimental treatment or, at the very least, the best available existing treatment for their cancer. Patients who receive the existing treatment typically still benefit from it as they would have if they had received it outside of the trial.
What is in a phase?
Clinical trials are conducted in at least three phases, each of which seeks to answer different questions about a new treatment It can take a long time for a trial to move from one phase to another, which means it might be years before a treatment is officially approved by the Federal Drug Administration.
In Phase I trials, physicians and scientists learn how a new treatment should be administered, what constitutes the optimal dose and schedule, and how the treatment
Phase II trials focus on how the treatment affects a specific type of cancer in larger groups of people Then, if treatment shows promise in Phase I and Phase II, it is tested in a Phase III trial, where physicians and scientists work to confirm its effectiveness, monitor any potential side effects and compare it to the existing standard-of-care treatments for that specific type of cancer Phase III trials are large-scale studies that can include hundreds or even thousands of people.
Who participates in clinical trials?
Despite the O’Neal Comprehensive Cancer Center’s push to expand its Clinical Trials Office and increase trial enrollment, only 3 percent to 5 percent of adult cancer patients in the United States participate in trials, according to Oncology Demographic data also indicates that cancer patients who enroll in clinical trials, both in and outside the United States, are more likely to be younger, male and white.
“Offering patients the opportunity to enroll in clinical trials as part of their overall treatment plan is just one example of what the O’Neal Cancer Center can do through its cancer services to give patients a genuinely comprehensive experience,” Sleckman said. “Clinical trials are now the standard of care for cancer, and they can and should be offered to every patient at UAB who could benefit from them”
Sleckman says it is imperative that patients understand the lifesaving potential of these clinical trials, as well as the many other cancer therapies and treatments that are available at UAB.
The O’Neal Comprehensive Cancer Center is committed to offering its patients a diverse array of high-value clinical trials with potential disease-altering impact
The O’Neal Trials program invests in building the Cancer Center’s clinical trials portfolio and training junior clinical faculty at the O’Neal Comprehensive Cancer Center to become nationally recognized clinical trialists.
May 28, 2021
O’Neal Cancer Service Line names Krontiras, Kennedy directors of clinical affairs, cancer network
Written by Anna Waters
O’Neal Comprehensive Cancer Center senior scientists Helen Krontiras, M D , and Gregory Kennedy, M D , Ph D , will begin new leadership roles within the O’Neal Cancer Service Line, effective June 1. These two new positions will direct the service line’s clinical operations and cancer network affiliations, respectively, and will replace the role of senior medical officer, which has been held by Warner Huh, M.D., since the launch of the service line in 2018
As the new director of clinical affairs for the O’Neal Cancer Service Line, Krontiras will lead its internal, operational, quality and clinical initiatives and will oversee its cancer management teams While in this new role, Krontiras will also continue to lead the Division of Breast & Endocrine Surgery in the UAB Department of Surgery as the division’s director, as well as serve as the associate chief quality officer for Ambulatory Patient Safety & Quality at UAB Medicine.
“The O’Neal Comprehensive Cancer Center at UAB has a long history of delivering high-quality cancer care,” Krontiras said “I am thrilled about the opportunity to build upon this foundation to enhance the experience of all patients diagnosed with cancer along every step of their journey”

Kennedy will serve as the O’Neal Cancer Service Line’s new cancer network director and will focus on its external-facing initiatives, including its partnerships with the St. Vincent’s Alliance, with Infirmary Health and with existing Cancer Network organizations, as well as on building relationships with the service line’s referring physicians across the state Kennedy also currently serves as a division director in the UAB Department of Surgery, where he leads the Division of Gastrointestinal Surgery.
“I am truly honored to be granted this opportunity to serve the members of the O’Neal Comprehensive Cancer Center,” Kennedy said “Our team will provide education and research opportunities for cancer providers across the region and will strive to ensure that all patients diagnosed with cancer in Alabama are able to find treatment for their disease in our state”
O’Neal Cancer Center Director Barry Sleckman, M.D., Ph.D., also oversees the O’Neal Cancer Service Line and says that, as the service line developed, it became clear that two distinct physician leadership roles were needed to support the internal and external initiatives for service line expansion The senior medical officer position search offered the opportunity to recruit candidates for both of these positions simultaneously and to quickly move forward with establishing these roles
https://www.uab.edu/medicine/news/latest/item/2340-o-neal-cancer-service-line-names-krontiras-kennedy-directors-of-clinical-affairs-cancer-network?tmpl=compon
“Weknew weneededa person dedicatedto each of these distinct and important activities,” Sleckmansaid.“The positionsof clinicalaffairs director and cancernetwork director and their associatedresponsibilitiesare key to the service line’sgrowth and its delivery of outstandingcare.”

JordanDeMoss, MSHA, vice presidentof the O’Neal Cancer Service Line, says the position of senior medicalofficer was originally createdto help bridge the gaps betweenthe more academic, research-orientedO’NealCancerCenterand the clinical, patient-facingservice line.
“We are sincerely gratefulto Dr. WarnerHuh’s leadership as senior medicalofficerover the past severalyears,”DeMoss said.“His contribution to launchingthe O’Neal CancerService Linein this role hasallowed the service line to evolveinto whatit is today.”
Huh is also a senior scientist atthe O’Neal ComprehensiveCancer Centerand the chair of the Department of Obstetrics & Gynecology in the UAB School of Medicine.
“Toserveassenior medicalofficerandbuild the O’Neal CancerService Linefrom the ground up wasa transformative and once-in-a-lifetime experience,” Huh said. “We were able to identifythe truestrengths andnecessary investments to furtherelevate ourclinicalcancerprogram. It became readily clear to us that weneededto expand physicianleadership in the areas of clinical operationsand our cancernetwork.”
Read more aboutthe O’Neal CancerService Lineand its role within the UAB Health System, the University andO’Neal CancerCenter.
https://www.uab.edu/medicine/news/latest/item/2340-o-neal-cancer-service-line-names-krontiras-kennedy-directors-of-clinical-affairs-cancer-network?tmpl=compon
Peopleof
Lindeman inducted into ACS AcademyofMaster SurgeonEducators
Written by: Anna Waters
Media contact: Adam Pope
Brenessa
Lindeman, M.D., assistant professor inthe UAB Division of SurgicalOncology, isamong a group of 91 esteemed surgeons from seven countries selected into membership or associate membership inthe new American Collegeof Surgeons Academy of Master Surgeon Educators™. The academy’s first induction ceremony occurred Oct. 3 atthe John B. Murphy Memorial auditoriuminChicago.
Lindemanwas inducted asan associatemember of thisprestigious Academy.She isthe associate program director for theUAB GeneralSurgery Residency Program and the associate designated institutionalofficial fortheclinical learning environment intheUAB Office of Graduate MedicalEducation.
Lindemanis a distinguished surgicaleducator whose experience inthe fieldincludes working nationally with the AAMC as a member of the draftingpanel fortheCore EntrustableProfessional Activities for EnteringResidency,andas a member of both the
drafting and implementation groupsfortheAmerican Board ofSurgery’sGeneral Surgery EPAs Project. She alsoservesas a module director for theAmerican Collegeof Surgeons’Advanced General Surgery Curriculumprojectandserved previouslyon the AAMC Board of Directors from 2012-2016.
“Itcomes asno surprisethat Dr. Lindeman has been selected tojointhe ACS Academy of Master Surgeon Educators,” said UAB Department of Surgery Chair Herbert Chen, M.D.“Her work, both inand out of the operatingroom,has benefited thelives of her patients, aswellasher co-workers and students. Brenessa’s hands-on approach to ensuring thecompetency and well-beingof medical students andresidents isexemplary of a surgical educator whoisdriven byher commitmenttoqualitypatient careand the education of current and future physicians.”
Developed under theauspices of theACS Division ofEducation, the academy recognizes surgeon educators who have devoted theircareers tosurgical education. Individualsare selected asmembers or associatemembers followingstringent peer review.Theacademy’smission isto play a leadershiprole inadvancing thescience and practice of education acrossallsurgical specialties, promoting thehighest achievements inthelifetimes of surgeons.
Health & Medicine
UAB opens new Multidisciplinary Endocrine Tumor Clinic
Written by: Anna Waters
Media contact: Adam Pope

Patients with thyroid, parathyroid, pancreas and adrenal tumors will soon have a onestop shop for endocrine neoplasia treatment. The University of Alabama at Birmingham’s new Multidisciplinary Endocrine Tumor Clinic opens Tuesday, Oct. 1, on the third floor of The Kirklin Clinic of UAB Hospital.
Patients who visit the clinic will have the opportunity to see a team of specialists in a single, initial consultation in order to accommodate patients and expedite their treatment plans
The Multidisciplinary Endocrine Tumor Clinic offers comprehensive and streamlined care for patients with benign or malignant tumors of the endocrine organs, such as neoplasms like thyroid cancer, hyperparathyroidism, multiple endocrine neoplasias and functional adrenal tumors
The clinic is led by co-directors Deepti Bahl, M.D , Ronadip Banerjee, M.D , Ph D , and Brenessa Lindeman, M.D., and is additionally supported by UAB Department of Surgery Chair Herbert Chen, M.D. Endocrinologists Bahl and Banerjee serve as assistant
professors inthe Department of Medicine’s Division of Endocrinology, Diabetes and Metabolism, while endocrine surgeons LindemanandChen serve as an assistant professor and professor inthe Division of SurgicalOncology, respectively.
On November 16, leading multiple endocrineneoplasiaphysicianswillpresent thelatest medicalinformation about MEN1, MEN2A, andMEN2B at the UAB WestPavilion
Conference Center from 8 a.m. to 5 p.m. Theevent issponsored by theUAB Department of Surgery,the O’NealComprehensive Cancer Center atUAB,Children’s of Alabama and AMENSupport. Toregister, please visitthe event'sofficialwebsite.
Referring physicians and other providers should call205-934-1211 andspeak with Vernessa Williams or Kelly Lovell, CRNP, tobegin the consultationprocess.
UAB alumnus/student/employee becomes patient following brain blood clot
Written by: Anna Waters
Media contact: Bob Shepard, bshep@uab.edu
Die-hard University of Alabama football fan Michel Thomas would not have missed the 2016 SEC championship game — the Florida Gators against his Crimson Tide for anything. Although he had spent the days before the game suffering from debilitating headaches and would spend the week after too nauseated to participate in final exams or project meetings with his classmates, Thomas made it to the Georgia Dome on Dec. 3, 2016, with his co-worker of 14 years, Tracy Taylor, R.N., nurse to UAB neurosurgeon Mark Harrigan, M.D.
Unbeknownst to both of them, Thomas attended

that game with a blood clot inhis brain,andHarriganwould later bethe one to remove it.
“I willsay I was pretty miserableduring thegame,” saidThomas, a business officer inthe UAB Department of Neurosurgery.“Iremember cheeringduringthefirstquarter during a turnover and thinking my head was going to explode.”
After nearlya week of constant headaches andnausea, Thomas — a UAB alumnus and a Master of Science inHealth Informatics studentinthe UAB School ofHealth Professions — finally sought treatmentat UAB Medicine UrgentCare for what he thought were common migraines.
“That Monday, after I quitthrowing up,I remember getting into the car to goto work, realizing I didn’t have my wallet, going backinside andthen going back to thecar just to realize I stilldidn’t have my wallet,”Thomas said. “By that point,itwas day five,and I was still having theseheadaches.Attheinsistence ofmyprimary care physician, Dr. Amy Lejeune,I decided to goto urgentcare,thinking that they would just giveme a migraine cocktail so I couldgoback to work and then gohome.”
Andrew Allen, M.D., thedoctor Thomas saw aturgentcare,says hecouldtellsomething was seriously wrong themoment hewalked in.
“Michel saidhewent to anAlabama footballgame the weekendbefore,and itseems likehis clot was expanding during thatgame,” Allen said. “He was complaining of a lot of intermittent headaches and vomiting,which wasa redflag for me.Initially,theintensity and localization of those headaches made meconcerned about an aneurysm.”
Allen immediatelysent Thomas to the emergency room,where a CTscan showed not ananeurysm but a blood clot. Thatnight,Thomas wasadmitted tothe hospital under thecare of Winfield Fisher, III,M.D., a UAB neurosurgeonwithwhom Thomas worked. Atthehospital, Thomaslearned that his most severe headaches andvomiting,as well ashis current, persisting symptoms,were due toa brain bleed anda blood clot inhis duralvenous sinuses,which drain bloodfrom the brain.Intracranial venous sinus thrombosis,as it iscalled, is a rare disorder that,inthiscase,was caused by a factor V Leiden deficiency,a hereditary hypercoagulability disorder.
“The symptoms of my condition were similarto thoseof an aneurysm; buta lot of people who have this kind of clot actually havestrokes, so I got lucky with a bleed instead,”Thomas said. “Eitherway,they’re bad; but the urgent care doctorgot meto the ER quickly.”
Angiogram images show blood vessels following thrombectomy and treatment with blood thinners.
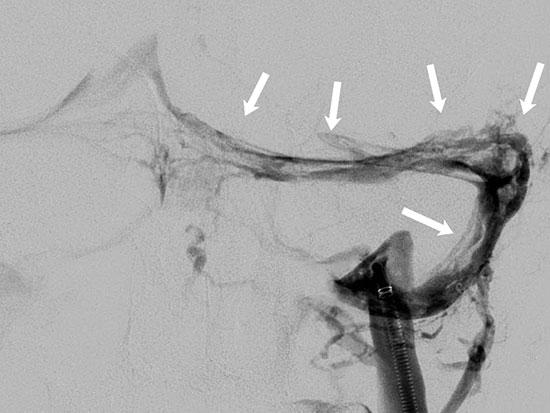
The arrows indicate scattered blood clots present throughout the venous system, which were diminished in size and extent after treatment.Fisher initially treated Thomas’ blood clots with blood thinners, hydration and pain
medication, which Fisher hoped would dissolve the blood clot and ease Thomas’ symptoms Because Thomas was in the hospital during finals, the School of Health Professions allowed him to take one of his finals on paper rather than on a computer screen, which caused him fewer headaches. However, even after he returned to work part time at the end of December, his headaches were still severe and frequent It was then that he went back to the ER and started to consider surgery to remove the clot.
The second time Thomas was admitted to the hospital, he was met by Harrigan, who suggested a thrombectomy, a procedure in which neurosurgeons lead a plastic catheter from the femoral vein in the leg to the venous sinuses in the head and then pull the blood clot out using a mechanical aspirator.
“This technique has come on the scene in the last six or eight years as a therapy for acute stroke, but we use it for intracranial venous sinus thrombosis as well,” Harrigan said “That system has certain design features that make it very useful for Michel’s condition.”
Thomas says his experience as a Department of Neurosurgery staff member helped him navigate the ins and outs of a neurosurgical procedure but didn’t prepare him for the experience of being the one in the hospital bed
“I already knew a little bit about the process from working in the hospital and directly with neurosurgeons, but it’s different when you’re the patient,” Thomas said.
Harrigan performed Thomas’ thrombectomy on New Year’s Eve, removing much of the blood clot and alleviating some of Thomas’ symptoms.
UAB neurosurgeonsWinfield Fisher and MarkHarrigan.
However, after three months,Thomaswasstillsufferingfrom severe,frequent headaches and light sensitivity that were interferingwithhis life.Part of theblood clot was still present inhisvenous sinuses, andthe samepainthat had followed him since December wasmaking it difficultfor him towork or gotoschool full time.When he discussed theseongoing symptoms withHarrigan, they began toconsider another thrombectomy to remove theremainder of the bloodclot.
“Wehave to relyon his opinion,”Harrigansaid. “In the old days,weused to reserve this for people who were getting really sick, like going into a comaorthingslikethat, and in that case,theneurologicchangeismore objective.But withthe bad headaches Michel was having,it’ssubjective.Wehad to relyon him totellushow bad his headaches were.”
Finally, Thomas’ second thrombectomy,onMarch 6, 2017, removed the entire clot and relieved mostof his symptoms.
“Weused thelargestof the catheters, called an ACE68,” Harrigansaid. “It’slikea great big straw, but bigger and longer.”
Thomassays hehas feltmarkedlybetter since his secondsurgery and has resumed his work and classes full time.
“I never fell behind in academics, thanks to the School of Health Professions, and I’m so grateful to them for working with me through all this,” Thomas said. “My co-workers were also just really supportive when I had to stay home or leave for doctors’ appointments, and I know that would have been the case even if I weren’t being treated by the faculty members in my department.”
Eta S. Berner, Ed.D., one of Thomas’ professors in the School of Health Professions, says she was impressed by his diligence in completing his coursework while he was in and out of the hospital.
“This is a disease that seems to affect younger people more than older people. We’ve done a lot of these procedures on people in their 20s or 30s”
“Michel was very conscientious in making up the work, even though he was still sick and had to manage the regular course workload as well,” Berner said “He did very well in the course, even with all that stress.”
While Thomas’ quality of life has been drastically improved, he still sees several UAB specialists to manage his headaches and is aware that this doesn’t mean he will remain blood-clot-free.
“He’s young; but he’s still at risk for recurrence of the blood clots in his head and for developing blood clots in other veins in his body, too,” Harrigan said. “This is a disease that seems to affect younger people more than older people We’ve done a lot of these procedures on people in their 20s or 30s.”
Harrigan explained that, while treating a co-worker is a different experience for him, he’s thankful to have had the opportunity to spend more time with Thomas during his recovery, and that Thomas has returned to work
“Because Michel is a colleague and friend, I see him a lot more frequently than I see other patients,” Harrigan said. “As his neurosurgeon, it is rewarding to see Michel successfully back in his daily routine.”
UAB spine surgery patient sees quick recovery after operation
UAB spine surgery patient sees quick recovery after operation
Details
Details
Written by: Anna Waters
Written
Published: October 30th, 2018
by: Anna Waters
Published: October 30th, 2018


Norine Wilson plays with her grandchildren in the yard, an activity she is now able to do after receiving spine surgery from UAB neurosurgeon Dr. Mamerhi Okor in June 2017. (Photo courtesy of Norine Wilson)
Norine Wilson plays with her grandchildren in the yard, an activity she is now able to do after receiving spine surgery from UAB neurosurgeon Dr. Mamerhi Okor in June 2017. (Photo courtesy of Norine Wilson)
Norine Wilson says she’s never been the type to sit around and wait on anything. After living with chronic pain in her back and legs for more than a year and meeting with physicians who suggested only short-term treatments, she was ready for a real solution.
Norine Wilson says she’s never been the type to sit around and wait on anything. After living with chronic pain in her back and legs for more than a year and meeting with physicians who suggested only short-term treatments, she was ready for a real solution.
“They said to try an epidural, or a shot, that would work for a while, but I wasn’t looking for temporary fixes,” Wilson said. “I wanted something that was going to work.”
Wilson, 69, had already met with an orthopedist, a chiropractor and a spine specialist and had spent months in rehab for the pain before she was referred to Mamerhi Okor, M.D., an associate professor in the UAB Department of Neurosurgery, in May 2017.
“They said to try an epidural, or a shot, that would work for a while, but I wasn’t looking for temporary fixes,” Wilson said. “I wanted something that was going to work.”
Wilson, 69, had already met with an orthopedist, a chiropractor and a spine specialist and had spent months in rehab for the pain before she was referred to Mamerhi Okor, M.D., an associate professor in the UAB Department of Neurosurgery, in May 2017.
“Pain kind of comes on gradually when you get older, so you don’t really know whether it’s something that can be fixed or you just need to rest more – whether you need to do more exercise or don’t need to do any exercise,” Wilson said. “But by the time that I got to see Dr. Okor, I already had it in my mind that I wanted a permanent fix.”
“Pain kind of comes on gradually when you get older, so you don’t really know whether it’s something that can be fixed or you just need to rest more – whether you need to do more exercise or don’t need to do any exercise ” Wilson said. “But by the time that I got to see Dr. Okor, I already had it in my mind that I wanted a permanent fix.”


Dr. Mamerhi Okor
Okor told Wilson that the epidural might only work for a few months at most but that the pain would eventually come back and that her best bet for a long-term solution was surgery.
“Ms. Wilson’s condition was the result of arthritic injury and age-related changes in the body, not any sort of trauma,” Okor said. “But she needed a lumbar fusion operation to lock down that joint between the bones in the spine to decompress the spinal canal.”
Okor told Wilson that the epidural might only work for a few months at most but that the pain would eventually come back and that her best bet for a long-term solution was surgery.
Okor said Wilson suffered from spondylolisthesis, a condition in which the vertebrae slip out of place, compressing the spine. This pressure eventually narrowed her spinal canal, causing spinal stenosis and the severe pain in her back and legs.
Dr. Mamerhi Okor
Wilson
“Ms. Wilson’s condition was the result of arthritic injury and age-related changes in the body, not any sort of trauma,” Okor said. “But she needed a lumbar fusion operation to lock down that joint between the bones in the spine to decompress the spinal canal.”
Okor said Wilson suffered from spondylolisthesis, a condition in which the vertebrae slip
Okor said Wilson suffered from spondylolisthesis, a condition in which the vertebrae slip out of place, compressing the spine. This pressure eventually narrowed her spinal canal, causing spinal stenosis and the severe pain in her back and legs.
Wilson had done some research on this kind of spine surgery and lamented the long recovery times that many other patients had reported.
“If you go online and add yourself to these groups and read all of these horror stories, which is what I did, it’s scary,” she said. “I know doctors can’t guarantee anything, but Dr. Okor was really optimistic about everything and how the results should be. It really put me at ease after I had decided that I had to do something permanent.
“I just felt very comfortable with him, so we went ahead and scheduled the surgery and went that route.”
Okor performed Wilson’s surgery in June 2017, and although recovery was difficult, she avoided rehab altogether by getting up, moving around and just performing the daily tasks she had been doing before surgery, per Okor’s suggestion.
“You kind of have to do regular stuff around the house, like picking stuff up off the floor, or at least try to,” she said. “Just do your regular, day-to-day activities, and then you can make yourself well on your own, rather than sitting around and letting people wait on you. Someone who just sits around won’t get as well as fast.”
In less than a month, Wilson had completely weaned herself off of the pain medication she was prescribed and had regained some of her independence.
“The process of getting up to walk around, sitting up from a chair and getting up from a chair really was my rehab,” she said. “By three weeks, I was completely off my meds and able to drive, which was a big thing for me because I’m very independent and just wanted to get out of the house. I think that’s why I recovered so quickly, because I was determined to get better as quickly as I could.”
Within two months, Wilson said she was completely free of the pain that had plagued her for more than a year.
“You go from having pain all the time when you walk to not having pain at all in two months,” she said. “I’ve walked and carried on all my life, but it always hurt, all of the time. In two months’ time, I was completely pain free in my back and free from the pain down my leg, which is amazing.”
Okor lauded Wilson’s recovery, noting that her results were, by no means, atypical.
“She is on the good side of things,” Okor said. “Some people struggle to get better overall, but a majority of patients have meaningful symptom relief after the surgery. Ms. Wilson had excellent results from the surgery which have remained until today.”
After her surgery, Wilson left a review of her operation online and was soon contacted by someone else who was considering the same operation but who was afraid of a long recovery time.
“Older people like me like to hear or read that it’s not going to be that long to recover, that it’s not going to be six months to a year until you feel better,” she said. “But I know that a doctor can’t guarantee that, so it’s really hard to say that you’re going to be driving in three weeks and, in two months, you’re going to be back to normal, which is what happened to me.”
Wilson said she was happy to share her positive experience with someone in the same position she was in prior to meeting Dr. Okor at UAB because she understood the need to talk about surgery with someone who had gone through it before.
“I don’t know, but I think that it’s very important for people to know that the recovery time is not that bad if you put the effort in,” she said. “And people like the interaction of speaking to someone familiar with it – not just the doctor.”
The patient with whom Wilson had spoken took her advice and shared the positive results of her own surgery in October 2017.
“I had the best results that I could have had, so I would definitely recommend Dr. Okor and UAB,” Wilson said. “I mean, you’re dealing with pain for over a year, and for someone to walk in and tell you that they think they can make you better and that they think the pain will be gone right after surgery, it’s amazing.”
https://www.uab.edu/medicine/neurosurgery/news-events/department-news/uab-spine-surgery-patient-sees-quick-recovery-after-operation
December 11, 2017
UAB joins national emergency trials network
Written by Anna Waters

The University of Alabama at Birmingham Department of Surgery within the School of Medicine has joined the National Institutes of Health SIREN network SIREN, short for Strategies to Innovate EmeRgENcy Care Clinical Trials Network, will coordinate and lead high-quality, multisite clinical trials to improve outcomes for patients who experience neurologic, cardiac, respiratory, hematologic and trauma emergency events
UAB is a sub-hub of the Oregon Health and Science University site, and will be participating as a site in a study of the use of hyperbaric oxygen following brain injury.The Division of Acute Care Surgery’s Jeffrey Kerby, M.D., Ph D , is the local principal investigator Mark Harrigan, M D , from the UAB Department of Neurosurgery, as well as Dag Shapshack, M D , and Michael Kurz, M D , from the UAB Department of Emergency Medicine, will also serve as local investigators in the trial