Preparing Clinicians for Modern Practice




18 PREPARING CLINICIANS FOR MODERN PRACTICE
The National Commission on Orthotic & Prosthetic Education has implemented new residency standards that shift focus from device-specific competencies to transferable skills that prepare graduates for real-world clinical practice. Learn about six key changes—including dual-discipline training requirements, new Minimum Activity Volumes, and expanded clinic location options— and what they mean for residents and program sites.
By JENNIFER DAVIS AND JOSEPHINE ROSSI


Get to know Brittany Gonzalez, CPO, who has reimbursement experience from both clinical and manufacturer perspectives.
View photos and highlights from AOPA's seminal conference in Orlando, where thousands of stakeholders convened to learn, network, experience the latest technologies, and celebrate the O&P community.
24 ORLANDO OVATIONS
Meet some of the brightest minds in O&P, who were honored with AOPA's most prestigious awards during AOPA's 2025 National Assembly. Find out how these individuals have and are continuing to revolutionize O&P patient care, research, advocacy, education, and business.
By JENNIFER DAVIS

Find out how Florida prosthetist Cara Negri, CP, LP, FAAOP, helped a patient recover from two amputation surgeries and prepare for a return to running competitions.

AOPA Contacts
A world where orthotic and prosthetic care transforms lives.
Board of Directors OFFICERS
President
Rick Riley
O&P Boost, Bakersfield, CA
President-Elect
Kimberly Hanson, CPRH Ottobock, Austin, TX
Vice President Matt Swiggum Proteor, Tempe, AZ
Treasurer
Chris Nolan
Immediate Past President Mitchell Dobson, CPO Hanger Clinic, Austin, TX
Executive Director
Teri Kuffel, JD AOPA, Alexandria, VA
DIRECTORS
Jeff Erenstone, CPO
Mountain Orthotic and Prosthetic Services, Lake Placid, NY
Deanna Fish, MS, CPO
Orthomerica Products Inc., Orlando, FL
Arlene Gillis, MEd, CP, LPO International Institute of Orthotics and Prosthetics, Tampa, FL
Adrienne Hill, MHA, CPO, LPO, FAAOP Kennesaw State University, Kennesaw, GA
Shane Kelly
Jim Kingsley
Hanger Clinic, Oak Brook Terrace, IL
Andrew L. Steele, MBA, CPO, LPO Clark & Associates Prosthetics and Orthotics, Waterloo, IA
Shane Wurdeman, PhD, CP, FAAOP(D) Clinician Director
Hanger Clinic, Houston Medical Center, Houston, TX
AMERICAN ORTHOTIC & PROSTHETIC ASSOCIATION (AOPA)
330 John Carlyle St., Ste. 200 Alexandria, VA 22314
Office: 571-431-0876
Fax: 571-431-0899 AOPAnet.org
AOPA Staff
EXECUTIVE OFFICES
Teri Kuffel, JD, executive director, 571-431-0876, executivedirector@AOPAnet.org
Akilah Williams, MBA, SHRM-CP, director of finance and strategic operations, 571-431-0819, awilliams@AOPAnet.org
HEALTH POLICY AND ADVOCACY
Ashlie White, MSHLS, MA, senior director of external affairs, 571-431-0836, awhite@AOPAnet.org
Joe McTernan, director of health policy and advocacy, 571-431-0811, jmcternan@AOPAnet.org
Devon Bernard, assistant director of coding and reimbursement services, education, and programming, 571-431-0854, dbernard@AOPAnet.org
Morgan Fabber, MPH, manager of state and federal advocacy, 571-431-0814, mfabber@AOPAnet.org
MEETINGS & EDUCATION
Ashley Vande Bunte, CMP, director, meetings and education, 571/431-0860, avandebunte@AOPAnet.org
Kelly O’Neill, CEM, assistant director, meetings and exhibitions, 571-431-0852, kelly.oneill@AOPAnet.org
Jules Gohng, meetings and education coordinator, 571-431-0843, jgohng@AOPAnet.org
MEMBERSHIP & COMMUNICATIONS
Joy Klapp, director of communications and membership, 571-431-0817, jklapp@AOPAnet.org
Betty Leppin, senior manager of member services, 571-431-0810, bleppin@AOPAnet.org
Madison McTernan, coordinator of membership and communications, 571-431-0852, mmcternan@AOPAnet.org
AOPA Bookstore: 571-431-0876
Reimbursement/Coding: 571-431-0833, LCodeSearch.com
O&P ALMANAC
AOPA, publisher
Josephine Rossi, editor, 703-662-5828, jrossi@contentcommunicators.com
Catherine Marinoff, art director, 786-252-1667, catherine@marinoffdesign.com
Bob Heiman, director of sales, 856-520-9632, bob.rhmedia@comcast.net
PUBLISHER AOPA
EDITORIAL MANAGEMENT CONTENT
COMMUNICATORS LLC
ADVERTISING SALES RH MEDIA LLC
DESIGN & PRODUCTION MARINOFF DESIGN LLC
PRINTING SHERIDAN
SUBSCRIBE
O&P Almanac (ISSN: 1061-4621) is published bimonthly by the American Orthotic & Prosthetic Association, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314. To subscribe, contact 571-431-0876, fax 571-431-0899, or email info@ aopanet.org. Yearly subscription rates: $59 domestic, $99 foreign. All foreign subscriptions must be prepaid in U.S. currency, and payment should come from a U.S. affiliate bank. A $35 processing fee must be added for non-affiliate bank checks. O&P Almanac does not issue refunds. Periodical postage paid at Alexandria, VA, and additional mailing offices.
ADDRESS CHANGES
Postmaster: Send address changes to: O&P Almanac 330 John Carlyle St., Ste. 200, Alexandria, VA 22314.
Copyright © 2025 American Orthotic and Prosthetic Association. All rights reserved. This publication may not be copied in part or in whole without written permission from the publisher. The opinions expressed by authors do not necessarily reflect the official views of AOPA, nor does the association necessarily endorse products shown in the O&P Almanac. The O&P Almanac is not responsible for returning any unsolicited materials. All letters, press releases, announcements, and articles submitted to the O&P Almanac may be edited for space and content. The magazine is meant to provide accurate, authoritative information about the subject matter covered. It is provided and disseminated with the understanding that the publisher is not engaged in rendering legal or other professional services. If legal advice and/or expert assistance is required, a competent professional should be consulted.
ADVERTISE WITH US
Share your message with AOPA membership— approximately 9,000 orthotic and prosthetic professionals, facility owners, and industry personnel. Contact Bob Heiman at 856-520-9632 or email bob.rhmedia@comcast.net
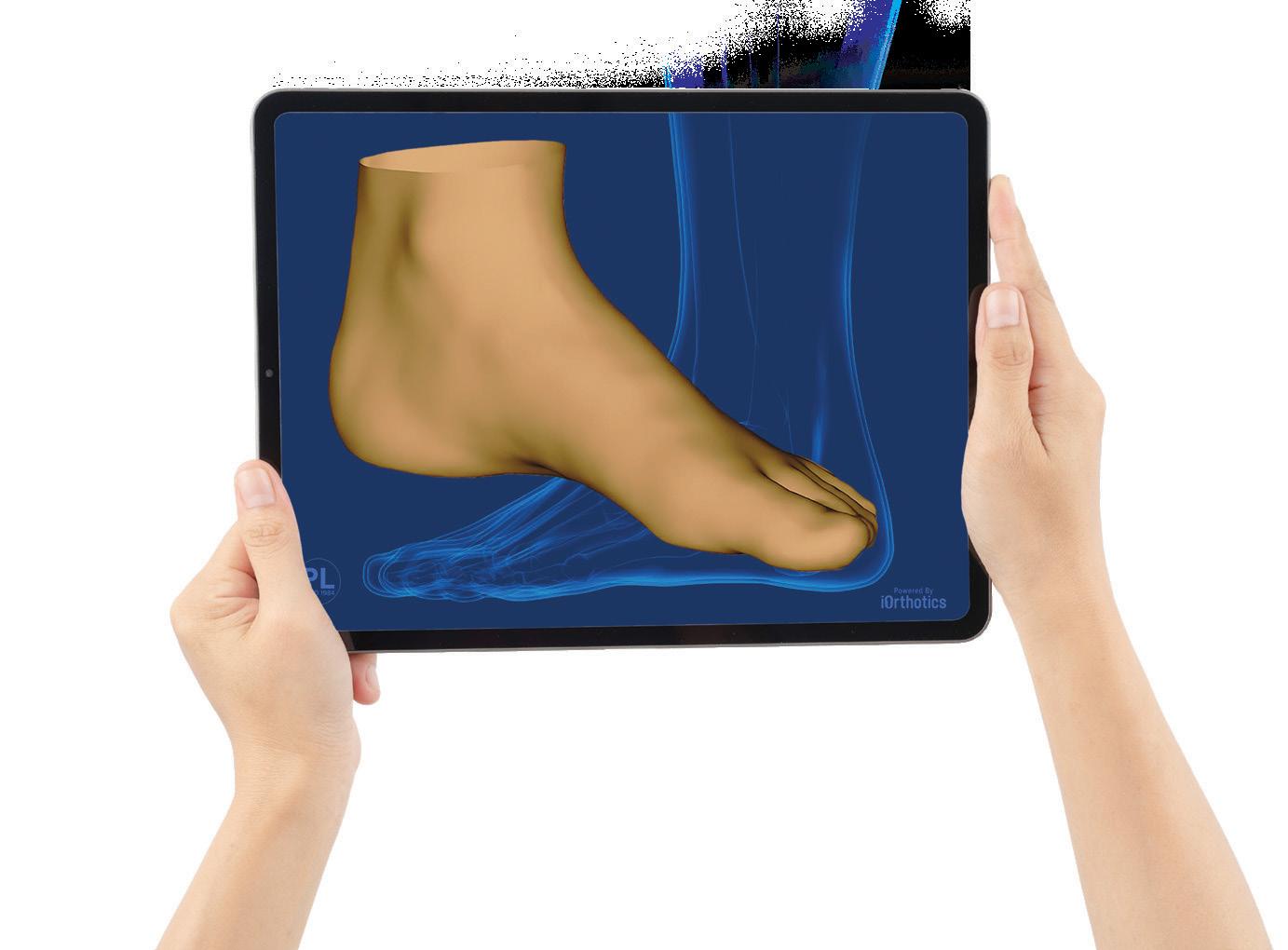
Open. Scan. Send.

few taps to order high-quality, perfectly fitting orthotics. Enjoy faster service and easy tracking – designed to simplify your practice and delight your patients. Hersco: simplifying orthotics, one scan at a time.
Happenings

RESEARCH ROUNDUP
Investigators Explore VR Training for Upper- and Lower-Limb Prosthesis Users
Two new studies demonstrate potential benefits of virtual reality (VR) training regimens for individuals with amputation.
An investigation focusing on lower-limb prosthesis users, published Aug. 31 in Frontiers in Rehabilitation Science, found that an interdisciplinary intervention involving VR promotes balance confidence. Nineteen adults with more than six months’ experience using a prosthesis for unilateral, transtibial amputation, and with low balance confidence, completed intervention sessions following a protocol that integrated physical therapy exercises—primarily VR active gaming—and cognitive behavioral therapy strategies, or eight weeks of at home-seated exercises. Results supported the initial efficacy of the VR intervention, and semistructured exit interviews suggested participants perceived benefit from the protocol.
K2 Transfemoral Prosthesis Users Benefit From MPK Technology
A landmark study published in Disability and Rehabilitation demonstrates that microprocessor knees (MPKs) significantly reduce falls and afford a better quality of life for individuals with above-knee amputations classified as limited community ambulators (Medicare K2 level). The study, “ASsessing Clinical outcomes with microprocEssor kNee uTilization in a K2 population (ASCENT K2),” was led by researchers from the Hanger Institute for Clinical Research and Education and Ottobock, working with collaborators from the University of Washington and University of Illinois Chicago.
The study followed more than 100 participants across the U.S.: half fit with an MPK and the other half using a nonmicroprocessor knee (NMPK). Over a 12-month period, researchers found that individuals using MPKs experienced significantly fewer falls and near-falls, and reported less activity avoidance due to fear of falling, compared to those using NMPKs. MPK users also maintained their health-related quality of life, while those in the NMPK group experienced a significant decline.
“These results challenge outdated assumptions about who benefits from innovative prosthetic care,” said Shane Wurdeman, PhD, CP, FAAOP(D), co-principal investigator and Hanger Clinic’s chief
A second study targeting myoelectric prosthesis users, published in Prosthetics and Orthotics International in August, sought to verify the effects of action observation and motor imagery (AOMI) using VR on myoprosthesis control. Researchers evaluated 24 healthy right-handed individuals wearing a myoprosthesis simulator in their dominant hands who were divided into three groups: VR video observation with electromyogram (EMG) presentation during manipulation; VR video observation without EMG presentation; and a control group. Results indicated that “AOMI using VR had sustained effects on motor learning of myoprosthetic control despite EMG presentation.” The researchers concluded that “AOMI, using VR, manipulates prostheses once learned, and it might be used for future training of myoprosthetic control.”

clinical officer. “Individuals that are of a lower functional ability can achieve meaningful improvements in safety, confidence, and quality of life with access to MPKs.”
“The ASCENT K2 study confirms what many clinicians have long observed in practice: Access to microprocessor knee technology can dramatically reduce fall risk and preserve independence and quality of life, even for individuals with low mobility,” said Andreas Kannenberg, MD (GER), PhD, co-principal investigator and executive medical director for Ottobock North America. “These findings should serve as a catalyst for policy change with commercial health insurances, ensuring all K2 patients, regardless of age or mobility within the K2 functional level, have access to prosthetic solutions that support both safety and quality of life.”
Nerve Stimulator May Hasten Postamputation Recovery
Patients may experience faster healing and less pain postamputation via a small nerve stimulator, combined with advanced nerve surgery, according to researchers and doctors at UVA Health.
One recent patient had lived with chronic foot pain and “debilitating discomfort” that significantly impacted his quality of life. He underwent belowknee amputation, during which doctors implanted a novel nerve stimulator designed to speed the healing process and block phantom limb pain. By the fourth day postamputation, he no longer felt any pain.
The nerve stimulator “provides the ability to stimulate the nerve in such a way that it … basically overwhelms your ability to process sensations and tricks your brain into turning off that area of your brain map of sensation,” said Brent DeGeorge, MD, PhD, a plastic surgeon at the University of Virginia. Future studies are planned.
Clinical Trial Will Test SensoryEnabled Neuroprosthesis

Researchers at Case Western Reserve University and the Louis Stokes Cleveland Department of Veterans Affairs have received a $9.9 million award from the U.S. Department of Defense Congressionally Directed Medical Research Program to test technology designed to make a prosthetic hand feel like a part of the user’s body. Participants with upper-limb amputation will compare standard prosthetic arms and hands to a sensory-enabled neural-controlled prosthesis called “iSens,” which stands for “implanted somatosensory electrical neurostimulation and sensing system.”
Part 1 of the study will involve a three-month initial testing phase to document how participants use their current devices, and participants will have electrodes and electronic modules implanted in their arms. For Part 2, participants will be sent home with their regular prosthesis for half the time and the iSens technology for half the time, then complete surveys and return to the lab for monthly testing. During the final phase of the study, participants will be randomized into a group that uses the new technology with only touch sensation enabled or with only the advanced motor control enabled, and then switch groups halfway through.
“We expect our neuroprosthesis to make life better for people with amputation,” said Emily Graczyk, PhD, who is leading the research, “but we don’t know if the biggest factor will be improved sensation or improved control, or both.”
Researchers Leverage AI for Scoliosis Care
A clinical tool that uses artificial intelligence (AI) for Cobb angle measurement is being developed by Yishan Zhong, PhD, from the Georgia Institute of Technology, and spine surgeon Selena Poon, MD, from Shriners Children’s Southern California. They studied the data of 1,000 scoliosis patients to develop an AI model that may be used in the future in patients’ medical records to help inform treatment decisions.
“Current manual scoliosis assessment is timeconsuming for clinicians who are already overwhelmed,” wrote Zhong and Poon. The subjective knowledge and experience of different clinicians result in variation in the measurement.
“Physicians diagnosing scoliosis really use the Cobb angle,” said Fran Farley, MD, Shriners Children’s chief medical officer, adding that AI can be helpful in measuring curves. “This shows lots of potential for minimizing time to make the measurement, but hopefully also making the measurement more accurate.”
CODING CORNER DME MACs and PDAC
Release 3D-Printing Guidance for Prosthetics
The durable medical equipment Medicare administrative contractors (DME MACs) and the Pricing Data Analysis & Coding (PDAC) contractor released guidance Sept. 18 on the use of additive manufacturing/3D printing. The new guidance states that 3D printing, or additive manufacturing, is an acceptable alternative to traditional custom fabrication.
The guidance emphasizes that using these means of fabrication must continue to “meet the Healthcare Common Procedure Coding System (HCPCS) long description of the individual HCPCS code, along with any other published coding guidelines.” This guidance has also been incorporated into the Lower-Limb Prostheses Policy Article. This new correct coding reminder is consistent with AOPA’s position that 3D printing/ additive manufacturing should be considered a valid fabrication method.
UPPER-LIMB USERS PRIORITIZE COMFORT
In a study to determine upper-limb prosthesis design requirements, “comfort” was found to be the most critical characteristic, followed by “maintenance” and “low weight.” SOURCE:
POLICY WATCH
O&P Alliance Launches Resources To Clarify Tariff Impact
The O&P Alliance has developed a set of resources designed to clarify potential impacts of new tariff policies that took effect Aug. 1, which may affect O&P patient-care facilities, manufacturers, and suppliers. The resources include summaries of how the tariffs may impact O&P and a flowchart outlining possible exemptions that may apply.
These resources focus on the Nairobi Protocol, a longstanding regulatory duty-free exemption for certain medical devices that has been in place for decades. While the Nairobi Protocol provides a pathway for certain medical devices, including orthoses and prostheses, to be considered for duty-free treatment, it is not a blanket exemption that applies in all situations. Tariff regulations remain complex, and exemptions are determined on a case-by-case basis.
This means that the default condition includes applicable tariffs on the import of orthoses, prostheses, O&P components, and raw materials. Interested parties must claim duty-free status upon importation of any products or materials at the point of entry

into the U.S. This process will primarily fall upon manufacturers and distributors of complete O&P devices, components, and materials using designated Customs & Border Protection forms.
While the Nairobi Protocol provides a clear pathway for consideration of tariff exemption for O&P devices, components, and materials, it is not all-inclusive and will be subject to interpretation as tariff implementation continues. AOPA will continue to monitor tariff implementation and will communicate updates and guidance as they become available. Contact Joe McTernan at jmcternan@AOPAnet.org or Devon Bernard at dbernard@AOPAnet.org with questions.
BY THE NUMBERS
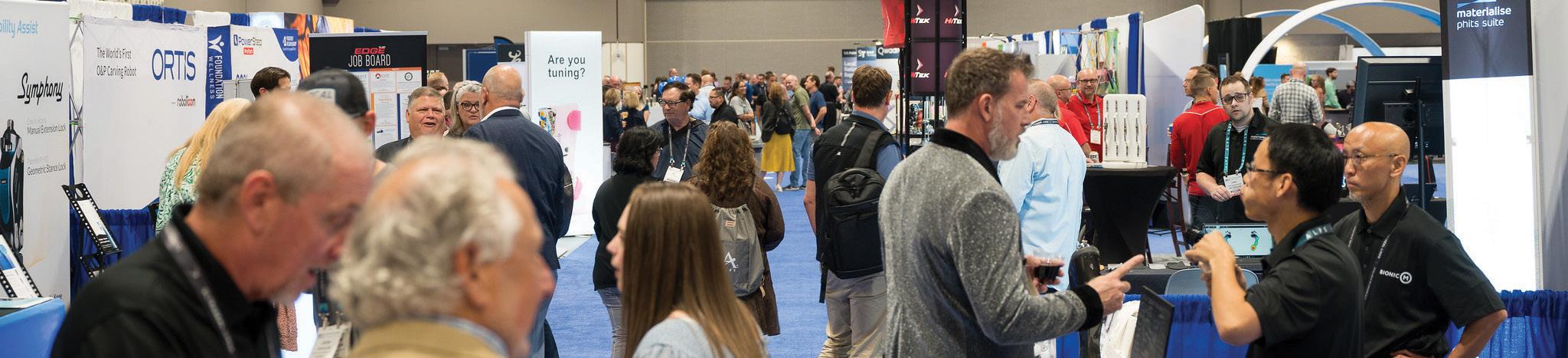
AOPA's 2025 National Assembly Makes History
This year’s National Assembly had impressive attendance and several first-time events.
30
30 first-time exhibitors, the largest number in AOPA history
2,065
2,065 attendees, returning to prepandemic levels
13
13 companies participated in the first-ever New Product Showcase

90+
30+ clinical education tracks, the most in AOPA history
Meracus®
Pure composite
Pure motion

Meracus® is crafted entirely from composite materials, setting a new standard in prosthetic design. Free from metal joints and unnecessary components, its pure composite build and rocker sole deliver a smooth, natural transition from heel strike to toe-off.
Meracus® contributes to:
ҋ a smooth, natural walking motion throughout the gait cycle
ҋ support and comfort while standing still
ҋ active everyday life due to its versatile features

O&P ADVANCES
PROSTHETIC IMPLANTS ON THE RISE GLOBALLY
“While exact global figures are difficult to pinpoint, estimates suggest that over 10,000 patients worldwide have received osseointegration implants since the technique was first introduced.”
SOURCE: “BREAKING
MEETING MASHUP
Academy and PFA To Partner for February Meeting
The Pedorthic Footcare Association (PFA) will host its 2026 Education Symposium in conjunction with the 2026 Annual Meeting & Scientific Symposium of the American Academy of Orthotists and Prosthetists (AAOP), Feb. 18–21, at the Gaylord Opryland Resort in Nashville. The PFA 2026 Education Symposium will be held Feb. 18–19.
“The Academy is proud to welcome the Pedorthic Footcare Association to Nashville,” said Gerald Stark, PhD, MSEM, CPOL, FAAOP(D), president of AAOP.
“Together, we are broadening the scope of AAOP 2026 to reflect the full continuum of orthotics, prosthetics, and pedorthics.”
“We are thrilled to partner with the Academy for this important event,” said Teresa Alpert, CO, CPed, president of PFA. “This collaboration underscores our shared commitment to improving patient outcomes through education and innovation.” Registration for both events opened Oct. 7.

Save the Date for OTWorld
Mark your calendar for OTWorld—International Trade Show & World Congress, scheduled for May 19-22, 2026, in Leipzig Germany. The conference will feature innovative studies, groundbreaking research, technical innovations, and exemplary treatment cases. Visit ot-world.com for details.

SOURCE: LEIPZIGER
PEOPLE
Shelly Barnett has been appointed chief executive officer (CEO) of Thuasne North America. Barnett joined Thuasne through the 2024 acquisition of Corflex Global, where she spent 11 years in senior leadership roles, including chief strategy officer and CEO. Her expertise in strategic integration, business optimization, and customer-focused innovation positions will help her lead Thuasne North America into its next phase of development.
Under Barnett’s leadership, the company will continue to strengthen its position in orthopedic bracing, compression care, and durable medical equipment solutions. “Our strategy must be both innovative and responsible,” said Delphine Hanton, global CEO. “Shelly’s collaborative leadership will unite our teams and drive customer-centered progress.”
“Thuasne North America has exceptional potential,” said Barnett. “By aligning our strengths and fostering innovation, we will deliver solutions that advance patient care and create lasting value for our customers, partners, and the business.”

Jeff Kessler has been named director of OPGA, where he will assist VGM’s OPGA community while further promoting the O&P profession for both OPGA’s members and their supplier partners. Kessler brings over a decade of experience across multiple roles within the VGM community. Most recently, he served as partner account manager at VGM & Associates. He began his career at VGM in managed care, later advancing to workers’ compensation operations specialist. Kessler has also held roles in Club Procure (formerly VGM Club), provider relations, and VGM market data.
“I have a deep respect for the skill, expertise, and value that O&P clinics, clinicians, and manufacturers bring to the patients they serve. While this is an endlessly rewarding field, the barriers to long-term viability for our shared mission continue to grow,” said Kessler. “As a survivor of a traumatic childhood accident, my commitment to this industry is also deeply personal. I grew up in the prosthetic community, visiting clinics and working with prosthetists for as long as I can remember. I’m excited to use my experience to help OPGA members and partners expand their impact on the patients and communities they serve.”
“Jeff has been deeply involved in the orthotics and prosthetics space for many years, and his experience working closely with manufacturers, distributors, and service providers makes him an exceptional fit for this role,” said Tyler Mahncke, senior vice president of clinical mobility and accessibility, VGM & Associates.
Jonas Ljung, CPO, has been named director of clinical and education services at the National Commission on Orthotic and Prosthetic Education (NCOPE). Ljung will lead NCOPE’s efforts to enhance clinical education standards, support residency programs, and foster innovation in O&P training nationwide.
With over 14 years of experience in O&P, Ljung brings a wealth of clinical expertise, educational leadership, and a deep commitment to advancing the profession. He previously served as clinic manager and the regional resident director of the Med-Atlantic Region at Hanger Clinic, where he was instrumental in developing residency programs, mentoring future practitioners, and advocating for evidence-based care.
“We are thrilled to welcome Jonas to the NCOPE leadership team,” said Robin Seabrook, executive director of NCOPE. “His passion for education and dedication to clinical excellence align perfectly with our mission to ensure the highest quality of orthotic and prosthetic education and training.”
William (“Bill”) Perno, MBA, FACHE, been appointed interim president and chief executive officer (CEO) of Amputee Coalition. He was most recently chairman and has been a dedicated board member of Amputee Coalition since 2018.
Perno will guide the organization with strategic focus and ensure a smooth transition, working closely with Amputee Coalition’s senior team to maintain momentum across programs, partnerships, and advocacy efforts. A national search for the permanent president and CEO will begin in October.

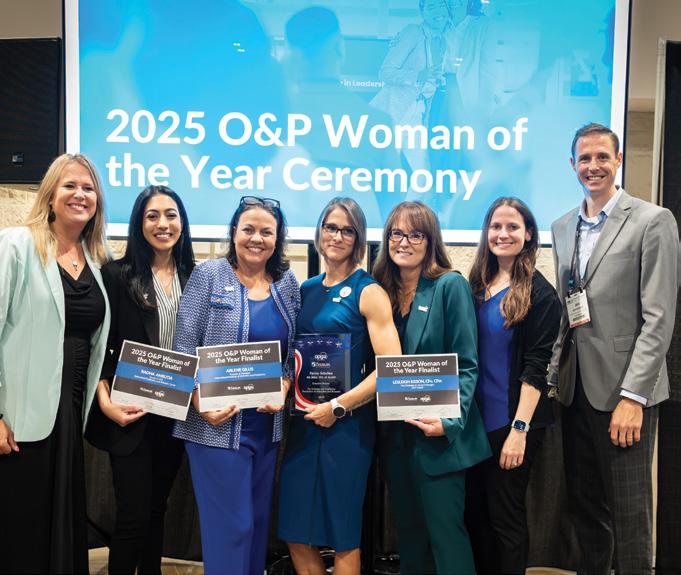
Fanny Schultea, MS, MSEd, CPO, LP, FAAOP, executive director of the Orthotics and Prosthetics Foundation for Education and Research, has been selected as the 2025 O&P Woman of the Year by OPGA. The award was presented to Schultea during AOPA’s 2025 National Assembly. Prior to her current role at the O&P Foundation, Schultea served as an assistant professor in the Baylor College of Medicine program in Houston and as director of O&P iQ at the American Academy of Orthotists and Prosthetists. She continues her service to the profession with the Limb Loss and Preservation Registry on the Scientific Committee. She is passionate about knowledge translation, healthcare quality, access, and innovation in O&P clinical care.
“Fanny Schultea exemplifies the spirit of innovation, leadership, and dedication that this award was created to honor,” said Tyler Mahncke, senior vice president of clinical mobility and accessibility for VGM & Associates. “Her contributions to education, research, and clinical excellence in the O&P profession continue to inspire and elevate the entire community.”
The O&P Woman of the Year Award, sponsored by Össur and presented by OPGA, a division of VGM & Associates, recognizes outstanding women in the O&P profession. Other finalists this year included Lesleigh Sisson, CFo, CFm, vice president and general manager at O&P Insight; Arlene Gillis, CP, LPO, founder and president of International Institute of Orthotics and Prosthetics; and Radha Amrutia, CPO, CFm, owner of Bakersfield Prosthetics and Orthotics Center.
Jeff Kessler
Fanny Schultea, MS, MSEd, CPO, LP, FAAOP


AHighlights From AOPA'S 2025 National Assembly
sense of growth and opportunity surrounding the O&P industry was in the air in Orlando Sept. 3-6 during AOPA’s 2025 National Assembly, when an impressive 2,065 O&P stakeholders came together for education, networking, exhibits, and camaraderie. From students and young clinicians to experienced business owners, manufacturers, educators, and entrepreneurs, everyone enjoyed exploring the latest innovations in orthotics and prosthetics from renowned researchers and skilled practitioners.
Enjoy these photos from the event, and be sure to read “Orlando Ovations” on page 24 for a deep dive into the award winners honored at the Assembly. Virtual content from this year’s Assembly will be available online through Nov. 25.
Mark your calendars now for next year’s Assembly, slated for Sept. 9-12 in Las Vegas.




AOPA Membership Meeting
Introduction of AOPA leadership by Rick Riley, AOPA president
Exhibit Hall
Welcome to Orlando Reception Singing Quartet
Welcome to Orlando Reception and Ribbon Cutting by Rick Riley, AOPA president







Law Judge Trial— Simulation Proceedings”

OPGA Woman of the Year (Center) Fanny Schultea, MS, MSEd, CPO, LP, FAAOP
Product Preview Theater Session
AOPA President-Elect
Kimberly Hanson, CPRH, Ottobock
Lesleigh Sisson, CFo, CFm; Curt Bertram, CPO, FAAOP; Mitchell Dobson, CP; Kimberly Hanson, CPRH; Dale Berry, CP, LP, FAAOP
BY DEVON BERNARD

Catch Up on Codes
New and revised codes and fees took effect Oct. 1

During the 2019-2020 coding cycle, the process for creating/adding a new code, revising an existing code, and discontinuing an existing code was updated by CMS to shorten the time from application submission to implementation. Under the updated process, code applications may be submitted on a biannual basis, and CMS publishes its final coding determinations more frequently. Code applications are now submitted either by the first business day in January, with a review in May/June and a new, revised, or deleted code possibly becoming active Oct. 1; or by the first business day in July, with a meeting and review in
November/December and the determinations becoming effective April 1 of the following year. This process enables a more rapid review and quicker update to the code set, allowing for newer technologies to be implemented more efficiently.
In addition to deciding if a code is to be added, revised, or deleted, the final code application determinations include an assignment to a Medicare benefit category (brace, artificial limb, durable medical equipment, etc.) and a Medicare payment determination. The payment determination includes being placed into a payment category (not separately payable, routinely purchased, oxygen, orthotics/prosthetics,
etc.) and the assignment of a fee under established protocols. The final determinations include a detailed explanation of how the fee is determined. At times, however, a new coding determination is not immediately assigned a new fee.
The updated biannual process is more transparent than in the past. For example, CMS has now published some of the criteria it uses when evaluating code applications, and it publishes the rationale for all preliminary and final determinations for each application. Now, everyone can see why a new code was created or why an existing code is acceptable, and how the new fee was established.
So, what were the results of the June 2-3, 2025, meeting? This month’s Reimbursement Page examines the new, revised, and deleted codes effective for claims with a date of service on or after Oct. 1, 2025.
New Codes & Fees
On Aug. 19, CMS released its final determinations from the first biannual Healthcare Common Procedure Coding System (HCPCS) code application meetings of 2025, which were held June 2-3. As a result of these final determinations, there are 12 updates of note for O&P providers/suppliers: seven new codes and five code revisions.
The first new code, L1007—Scoliosis orthosis, sagittal-coronal control provided by a rigid lateral frame, extends from axilla to trochanter, includes all accessory pads, straps, and interface, custom fabricated— was created to describe an adult scoliosis

brace. The final determination stated that the brace “could be beneficial to individuals with adult scoliosis based on the personalized fit, targeted postural alignment, possibility of pain reduction, and as a noninvasive alternative to surgery.” Because of these benefits, it was determined that the brace should be considered custom fabricated, and it is the only custom-fabricated scoliosis brace.
The L1007 was assigned to the brace benefit category; however, no fee was determined or assigned at this time. It was decided that a fee would be established during a future meeting.
The next new code is L5657—Addition to lower-extremity prosthesis, manual/automated adjustable air, fluid, gel, or equal socket insert for limb volume management, any materials. Initially, the preliminary findings of the panel were to not create





a new code for socket inserts designed to provide limb-volume management, as the panel believed the current sock codes would be appropriate. However, the panel reversed course and created the new code, indicating that the L5657 could take the place of multiple socks and is adjustable, where current socks are not.
The L5657 was assigned to the prosthesis (artificial leg) benefit category; however, no fee was determined or assigned at this time. It was decided that a fee would be established during a future meeting.
The remaining five new codes describe upper-limb prostheses—more specifically, partial hand prostheses and prosthetic digits. The majority of these codes are a continuation of the recent work being done to overall partial hand coding. The new codes include the following:

Style: 728-E | Triple Depth
Size: 5, 5.5-11.5, 12-17




• L6034—Partial hand, finger, and thumb prosthesis without prosthetic digit(s)/ thumb, amputation at distal to metacarpal joint, including flexible or nonflexible interface, molded to patient model, for use without external power and/ or passive prosthetic digit/thumb, not including inserts described by L6692
• L6035—Single prosthetic digit, mechanical, can include metacarpophalangeal, proximal interphalangeal, and/or distal interphalangeal joint(s), with or without locking mechanism, can include flexion or extension assist, any material, attachment, initial issue or replacement
• L6036—Prosthetic thumb, mechanical, can include metacarpophalangeal, interphalangeal joint(s), with or without locking mechanism, can include flexion or extension assist, any material, attachment, initial issue or replacement
• L6038—Addition to single prosthetic digit or thumb, mechanical, attachment, multiaxial, and/or internal/external rotation/abduction/adduction mechanism, with or without locking feature, any material
• L6039—Passive prosthetic digit or thumb prosthesis not including hand restoration partial hand, full or partial, custom made, any material, initial or replacement, per single passive prosthetic digit or thumb
These five codes were assigned to the prosthesis (artificial arm) benefit category; however, no fees were determined or assigned. It was decided that a fee would be established during the second biannual meeting in November/December. In the meantime, the fees or payments will be determined by each durable medical equipment Medicare administrative contractor (DME MAC).
Revised Codes & Fees
The first two of the five codes whose official descriptor changed, or verbiage was updated, are for the socket inserts L5673 and L5679. The changes were made
to reflect new manufacturing methods and the availability of perforated liners that enhance breathability. Here is the new verbiage:
• L5673—Addition to lower extremity, below knee/above knee, custom fabricated from existing mold or prefabricated, socket insert, silicone gel, elastomeric, or equal, with or without perforations, with or without breathable material, for use with locking mechanism
• L5679—Addition to lower extremity, below knee/above knee, custom fabricated from existing mold or prefabricated, socket insert, silicone gel, elastomeric, or equal, with or without perforations, with or without breathable material, not for use with locking mechanism
The revised liners remain within the prosthesis (artificial leg) benefit category, and the fees were not changed: The average fee for the L5673 in 2025 is $895.15; the average fee for the L5679 is $745.93.
The next two verbiage updates are related to fairly new codes that describe “mechanical, residual-limb volume management systems,” codes L5783 and L7406. The revised language is as follows:
• L5783—Addition to lower extremity, user adjustable, mechanical, residual limb volume management system (with or without lamination kit)
• L7406—Addition to upper-extremity prosthesis, user adjustable, mechanical, residual limb volume management system (with or without lamination kit)
The change was to include the mention of the lamination kit involved with the fabrication of the system into the prosthetic socket. The revised codes remain within the prosthesis (artificial leg) benefit category, and the fees were not changed; the average fee for both the L5783 and L7406 in 2025 is $3,088.30.
The last code revision is to partial hand code L6028. The new verbiage is: Partial
hand, finger, and thumb prosthesis without prosthetic digit(s)/thumb, amputation at metacarpal level, including flexible or nonflexible interface, molded to patient model, including palm, for use without external power and/or passive prosthetic digit/thumb, not including inserts described by L6692.
What is interesting about this change is that the panel has determined and stated that L6028 will be temporarily invalid for Medicare claims submission, because there are already a series of codes to describe partial hand, finger, and thumb prostheses without prosthetic digit(s)/thumb. These codes are the L6000 (partial hand, thumb remaining), L6010 (partial hand, little and/or ring finger remaining), and L6020 (partial hand, no finger remaining). The panel has indicated it plans to delete the L6000, L6010, and L6020 as part of the second biannual meeting, and crosswalk the three codes to the L6028.
The reason for the delay in deleting the L6000, L6010, and L6020 is that the panel wants to create a fee for the newly revised L6028 first, which will be done during the November/December meeting. This means that come April 1, 2026, the L6000, L6010, and L6020 will be deleted from the HCPCS code set, and L6028 will become valid for Medicare claims submission.
Deleted Codes
No codes were deleted as a result of the first biannual meeting. However, it is likely that a few codes may be deleted as a result of the November/December meeting.
Be sure to update your code sheets and systems to accommodate these changes, and remember that they took effect for all claims with a date of service on or after Oct. 1, 2025.

Devon Bernard is AOPA’s assistant director of coding and reimbursement services, education, and programming. Reach him at dbernard@AOPAnet.org





Cover Story COVER STORY
BY JENNIFER DAVIS AND JOSEPHINE ROSSI

PREPARING CLINICIANS FOR MODERN PRACTICE
Six key changes to O&P residency standards aim to better train clinicians for the realities of today’s healthcare environment
The way O&P patient-care professionals are trained is changing. Educational programs and accrediting bodies are moving away from a narrower focus on specific devices and toward the broader skills clinicians need in today’s healthcare environment. With new residency standards and updated certification processes taking effect, the goal is clear: Produce adaptable, well-rounded practitioners who can handle the real-world complexities of patient care and business management while maintaining the profession’s high standards.
O&P educational programs are increasingly addressing the gap between academic training and clinical practice by expanding their curricula beyond traditional technical content. Updated programs now emphasize professional skills such as conflict management and professionalism, while also incorporating practical business competencies including coding, billing, and documentation. These curricular enhancements are designed to complement residency training and better prepare graduates for the
realities of full-time clinical work, reflecting a broader trend across O&P education toward developing more well-rounded practitioners.
As a next step, the National Commission on Orthotic & Prosthetic Education (NCOPE) has implemented new residency standards that maintain the core purpose of residency but no longer tie competency to a particular device. Instead, the standards have evolved to provide immersive real-world experiences that aim to develop independent, competent, entrylevel professionals. According to Chris Robinson, CPO, ATC, FAAOP(D), MS, MBA, NCOPE’s director of accreditation and technology services, the 2025 residency standards include 44 unique competencies, with a new focus on transferable skills applicable across multiple interventions and enhancing adaptability in practice. Professionalism and ethics, communication, decision-making skills, collaboration, and professional development and well-being figure heavily in the competencies residents must master to receive a certificate of completion.
NCOPE works closely with American Board for Certification in Orthotics, Prosthetics, and Pedorthics (ABC) to ensure residency standards align with the updated certification process and the profession’s trajectory. Every five to seven years, ABC conducts a formal practice analysis by distributing a comprehensive survey to professionals in the field. “This survey helps identify the tasks prosthetists and orthotists perform in their daily practice,” said Stephen Fletcher, CPO, director of professional credentialing for ABC. “The results are then used to develop the certification exam blueprint.”
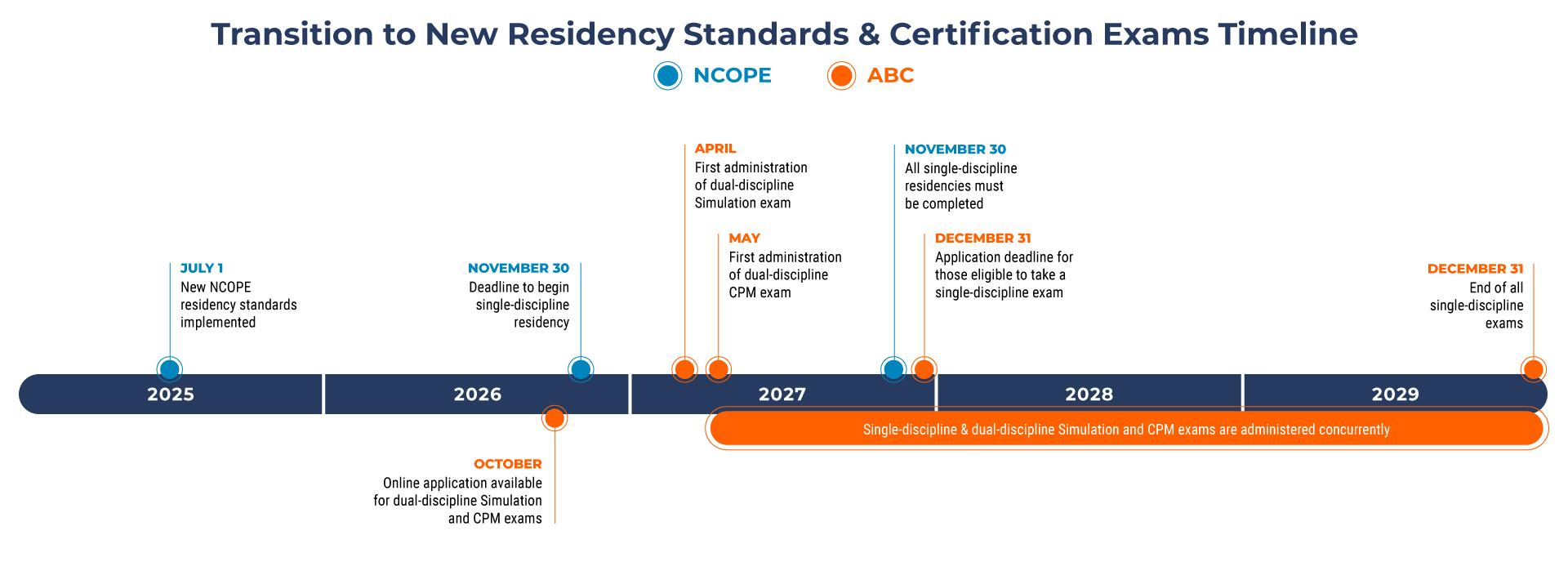
A clear example of how ABC’s exams adapt to changes in education and training is the integration of prosthetic and orthotic disciplines within the exams. The written multiple-choice exam was combined in 2019, and the written simulation and clinical patient management (CPM) exams will transition to the dual-discipline format in 2027. These updates align with the profession’s transition to a combined-discipline master’s degree in orthotics and prosthetics, which became the standard educational pathway in 2015.
The new NCOPE residency standards went into effect on July 1, 2025, for any program receiving initial accreditation or reaccreditation after that date. Programs accredited prior to that date will continue to follow the previous standards until they seek reaccreditation.
At the 2025 AOPA National Assembly, Robinson and Jonas Ljung, MSPO, CPO, director of clinical and education services for NCOPE, discussed these important changes and helped attendees navigate the relevant effects for residents and program site managers. O&P Almanac also followed up with NCOPE to highlight six key changes with the 2025 update:
Both orthotic and prosthetic training are required. Before July 1, individuals could pursue singlediscipline residencies and receive a certificate of completion for each discipline. Now, candidates must meet all requirements in both orthotics and prosthetics to successfully finish an NCOPE-accredited residency program. They will receive a single certificate of residency completion. These changes dovetail with ABC’s transition to combined simulation and CPM exams. Residents may begin to apply for
dual-discipline simulation and CMP exams in October 2026. “By the end of 2029, all newly certified clinicians will be certified in both orthotics and prosthetics—so CPO only,” Ljung explained to Assembly attendees.
Residency sites are not required to offer training in both disciplines. Sites that can only train residents in a single discipline may continue to hold NCOPE accreditation. Residents seeking training in both disciplines will need to pursue a 2-Site Residency Program—completing orthotics training at one site and prosthetics training at a second site. Upon finishing training in both disciplines, these residents will receive a single certificate of completion that identifies both sites.
Clinics that traditionally offered training in both orthotics and prosthetics but trained residents in one discipline at a time may continue this approach under the new standards. These residents register once for a 1-Site Residency Program. “They do the training in both the disciplines focusing on one at a time, and there’s one certificate of completion and subsequent board eligibility to sit for the combined boards,” Robinson explained.
MAVs have replaced time requirements. Previously, combined O&P residents were required to spend a minimum of 40% of their time being trained in either discipline. Now, Minimum Activity Volumes (MAVs) are being used to measure a resident’s clinical exposure.
MAVs identify a minimum number of visits a resident must have for specific orthoses and prostheses, patient demographics, and visit type, such as an initial evaluation. Each office visit with the resident equals one MAV activity, and the resident must act independently for a specific number of visits for specific O&P devices. Fabrication activities do not count toward MAVs.
“These numbers haven’t been pulled out of thin air,” Ljung said. Using a decade’s worth of NCOPE data, they were determined based on what a typical individual sees throughout their residency at hosting clinics with the “bottom 5%” patient volume. “So, 95% of existing residency sites will meet these minimum activity volumes in normal day-to-day operations. You don’t have to make any changes to your program.”






See through design
instructions and

One-piece body MONO CORE Technolog y®
Lenna rt , a foot drop pat ient from the Netherlands , walking the rainy streets of Leipzig, Germa ny
A Message for Current Residents

Pediatric prosthetic experience is not required. Residents can complete their training without any exposure to pediatric prostheses at any level of engagement. Pediatric MAVs are still required in orthotics training, however.
This change for the prosthetic discipline reflects real-world practice, where patients with congenital limb differences are rare and typically treated in specialty clinics, according to Ljung.
4Minimum duration is 18 months. The new minimum duration for an O&P residency—whether performed at one site or two—is 18 months. Individuals who take the two-site pathway must spend at least nine months focused on orthotic or prosthetic practice at each site.
The standards allow for O&P residency programs to operate for longer than 18 months, and many sites capable of training in both orthotic and prosthetic management plan to offer 24-month residency programs, according to NCOPE. “The standards define minimums. At no point is NCOPE going to tell you, ‘Sorry, you’ve
Need More Information?
The NCOPE website has been updated to provide resources tailored to residency education under the 2025 residency standards. Scan here or visit ncope. org/residency-resources.

If you’re already in training or about to start, the requirements that apply to you are based on your residency’s first day. You'll be held to the standards that were in place when you began. There’s also a transition window for single-discipline training. Residents can still register for a single-discipline orthotic or prosthetic residency under the previous standards, but only if they start by Nov. 30, 2026, and complete their training by Nov. 30, 2027. Sites that held active NCOPE accreditation as of June 30, 2025, and maintain that accreditation can continue enrolling single-discipline residents in any discipline they were previously approved to offer.
got to teach it faster. It's got to be 18 months,’” said Robinson. “If you have a curriculum … that enables effective training, but it takes 24 months, go for it.”
Residency terms are determined at the time a site applies for accreditation, and the site must advertise and operate the program for the approved duration. Residents who fail to meet all requirements within the defined duration may have their training program extended.
Satellite and partner clinics have replaced affiliate sites. Residency programs that meet accreditation requirements can now utilize remote partner clinics and satellite locations to provide residents with exposure to a more diverse patient population. Under the previous standards, residency sites could identify “affiliate” clinics to enable residency training within a 75-mile radius of the primary residency training facility.
The new standards allow residency sites to designate additional types of training locations within a 50-mile radius of the primary facility: “local satellite” clinics owned and operated by the same company as the primary facility, and “local partner” clinics owned and operated by a different organization. "Remote" satellite and partner clinics beyond 50 miles also are permitted, provided they hold full independent NCOPE accreditation. These changes help ensure residents maximize their time engaged in patient care.
Two important exceptions apply to these distance requirements. Rural clinics located in federally designated rural areas may extend the radius to 75 miles for both local satellite and partner clinics. Additionally, remote satellite and partner clinic rotations cannot exceed two weeks for a 52-week period unless the resident agrees to an extended placement prior to accepting the residency position.
Program leadership requirements, structure, and responsibilities have changed. According to the new standards, each residency program must have a single program director, though that director may appoint one or more associate directors. The director and/or any associate directors must participate in all quarterly resident evaluations, but only the program director has the authority to complete the final evaluation. The program director also bears overall responsibility for the program.
The education and certification/licensure requirements for directors, associate directors, and mentors remain unchanged. However, directors must have four years of post-certification experience, while mentors need two years of post-certification experience. Additionally, both mentors and directors must complete their required training within three years of their site’s accreditation or renewal.
“What that means is that those online director and mentor training courses that you’ve taken? They're no longer one and done—you do have to take a refresher every three years,” Ljung explained to attendees.
The 2025 standards also introduce new qualifications for research mentors at sites that choose to offer a research residency track. Research advisors provide oversight and guidance for research-focused residents’ directed studies. To qualify as a research advisor, individuals must have at least two
publications, two conference presentations, and documented research ethics training.
Greater Flexibility, More Opportunities
Overall, the updated standards give residency programs more flexibility in how they structure training. Sites that have developed effective approaches over the years can continue using them, while all programs now have options that weren’t available under the old standards. By defining elective orthoses and prostheses rather than requiring a fixed list of interventions, the new standards open the door for more sites to pursue and achieve accreditation.
Still, some core program requirements remain essential. Training and documentation must still demonstrate that residents are gaining autonomy progressively throughout their program. Patient-care experiences continue to be documented in NCOPE Tracker, and all required forms must be submitted through the system.
Jennifer Davis is a contributing writing for O&P Almanac Josephine Rossi is editor. Reach them at jdavis@contentcommunicators.com and jrossi@contentcommunicators.com
Editor’s Note: For more information, view the 2025 residency standards on the NCOPE website or email residency@ncope.org with questions.

November 17-18, 2025
BY JENNIFER DAVIS

ORLANDO OVATIONS
AOPA celebrated its best and brightest minds during the 2025 National Assembly

Arecord 2,065 members of the O&P community convened Sept. 3-6 in Orlando for the AOPA’s 2025 National Assembly, shining a light on the individuals and innovations that are revolutionizing patient care and evolving the industry.
Attendance at this year’s premier O&P conference surpassed prepandemic attendance levels once again. Participants enjoyed several new and exciting features at the event, including popular “Ask Me Anything” sessions and hands-on labs and digital showcases.
One of the most anticipated events of each year’s Assembly is the prestigious awards program, which honors the bright minds and dedicated professionals continually working to improve the field. Here’s a recap of the research, business, and advocacy efforts recognized in 2025 via the Thranhardt Award, Hamontree Business Education Award, inaugural James H. Campbell Commitment to Outcomes Award, Lifetime Achievement Award, and Snell Legislative Advocacy Award.
Raising the Bar in Research
Celebrating outstanding research contributions that advance patient care and improve outcomes has been a hallmark of the Thranhardt Award, and the presentation of its best-in-show clinical abstracts is a highlight of AOPA’s National Assembly.
Established in 1996 by an endowment from the Hanger Southeast Co. and now supported by the Orthotics and Prosthetics Foundation for Research and Education, the Howard R. Thranhardt Award has become one of the most respected honors in O&P. The information shared in Orlando by the 2025 award winners—Levi Hargrove, PhD, for his work related to phantom limb pain, and Tyler Klenow, MSPO, MBA, CPO, FAAOP, and Russell
Howard R. Thranhardt 2025 Award for Orthotics: “Improvement in Walking Speed and Reduction in Falls and Risk of Falling in SCI Patients in the C-Brace ® Registry” by Russell Lundstrom, MS (far left), and Tyler Klenow, MSPO, MBA, CPO, FAAOP, Ottobock (right), pictured with Andreas Kannenberg, MD (GER), PhD (center)

Lundstrom, MS, for their work evaluating the C-brace among individuals with spinal cord injury—exemplifies the power of clinical research to shape and elevate the O&P profession, according to Rick Riley, president of AOPA.
Hargrove, scientific chair of the Regenstein Center for Bionic Medicine at Shirley Ryan AbilityLab, presented the results of a clinical trial evaluating a new portable, at-home pain management system for treating phantom limb pain (PLP). The trial assessed the effectiveness of an electromyography-driven virtual reality (VR) system in reducing PLP symptoms in individuals with upperand lower-limb loss. The system connects an expandable cuff that conforms to the residual limb with an app that uses games and simulations to encourage wearers to attempt movements with their phantom limb. “The idea is that you can decode physiologically appropriate muscle movements into commands for prosthetic limbs,” Hargrove said.
Following 45 patients who used the device at least 20 minutes, four times a week, for eight weeks, the study documented a statistically significant and clinically meaningful reduction in pain over 32 weeks, highlighting the potential of VR therapy for long-term PLP management and telerehabilitation.
Hargrove is working with Coapt, a company he co-founded in 2012 to commercialize pattern recognition control algorithms for prostheses and orthoses, to launch a commercial version of the home-based therapy next year.
Klenow and Lundstrom returned to the Thranhardt lecture series this year, delving back into the C-Brace Registry, which collects real-world safety and effectiveness data from patients fitted with the microprocessor stance- and swing-controlled orthosis designed to help users achieve a more natural gait.

Digital Distinction
Cara Negri, CP, LP, FAAOP (right), and O&P resident MaryKate Dennis, (left), both of Gainesville Prosthetics, received the Professor Hans Georg Näder Digital O&P Care Award for their presentation, “Integrating Traditional and Additive Manufacturing in Prosthetic Residency.”
Sponsored by Ottobock Healthcare in honor of Professor Hans Georg Näder’s many contributions to the field of orthotics and prosthetics, the Digital O&P Care Award highlights innovations in technology that are changing the direction of patient care.
They were recognized in 2024 for their overall study analyzing the C-brace’s effectiveness for individuals with all injury types following one year of use. Their 2025 presentation featured a sub-analysis of patients with spinal cord injury (SCI), revealing the C-brace improved walking speed, functional mobility, and balance confidence while reducing fall frequency and improving quality of life in these SCI patients.
Klenow, a senior clinical research associate with Ottobock, has managed the C-Brace Registry for more than three years. Patients involved in the research were assessed using the 10-Meter Walk Test and the Timed-Up-and-Go test, and provided information about their pain, quality of life, falls, and personal goals, such as walking on uneven terrain or completing household chores.
Eighty percent of SCI subjects were “responders,” meaning they improved in at least one outcome and did not decline in any, or “partial responders,” meaning they improved in more outcomes than they declined in, Lundstrom, director of clinical research and services for Ottobock North America, explained.
“When we specifically look at SCI, the C-brace played a significant role in helping patients achieve their individual goals, and that resulted in improved quality of life in most patients,” he said.
Howard R. Thranhardt 2025 Award for Prosthetics: “Phantom Motor Execution Therapy for Phantom Limb Pain: A 45 Participant Home-Based Connected Health Clinical Trial” by Levi Hargrove, PhD (left), pictured with Matt Wernke, PhD
The Business of Charting
The Sam E. Hamontree, CP(E), Business Education Award was created to recognize the best business education paper, idea, or proposal submitted for presentation.
The two contenders for the 2025 award both explored the hot topic of how clinicians can adjust their documentation to improve the likelihood of getting insurance claims approved—and how tailoring documentation to include the information insurance companies need and want can simultaneously improve clinical notes.
Curt Bertram, CPO, FAAOP, and Lesleigh Sisson, CFo, CFm, of O&P Insight Consulting, clinched the Hamontree Award for their presentation, “Lessons Learned from a UPIC Audit.”
The other nominee, Dale Berry, CP, FAAOP, LP, of Prosthetic Xpert Consultation, provided tips for improving charting in his presentation, “SOAP Charting for the New Millennium.”
Berry said he learned Subjective, Objective, Assessment, and Plan (SOAP) charting in college in 1978 when Medicare was just 6 years old and 72% of all Americans were covered by three broad categories of private insurance. Today, SOAP charting is still taught in much the same way, despite massive changes in the insurance industry and claims processing.
“There are 1,176 insurance companies in the USA,” Berry said. “Each one of these insurance companies has its own process, its own procedure for prior authorizations, for reviews, for audits and everything else.”
Berry suggests revising the SOAP method to provide for “Specific patient information, an Overview of their case, Accurate device descriptions, and coding information and a Personalized care plan.”
Focusing on describing a patient’s injury and mobility needs, what device they have, what device they need, and why they need it is the key to providing good patient care and getting the necessary insurance approval.
During Bertram’s and Sisson’s presentation, Sisson explained that one of the biggest pitfalls to achieving those approvals is cloned documentation. Whether AI-generated or crafted by a clinician who then cuts and pastes language from one chart to another, insurance companies balk at seeing remarkably similar language from claim to claim and beneficiary to beneficiary.


E. Hamontree, CP(E), Business Education 2025 Winner:
“When using templated information, it’s not patient-specific,” Bertram said. “This is the trap you can get yourself into. It can become rote, especially using templates. Instead of telling us what the device can do, tell us how the patient can benefit.”
Bertram, Sisson, and Berry agree that short—but detailed and individualized—patient notes are the most efficient way to achieve insurance authorizations and approvals. Spending a few extra minutes to provide examples of the patient’s activities and barriers to tell the story of a day in the life of the patient is what will achieve approvals—and ultimately save time by avoiding appeals.
“If you can read the documentation and picture that patient and what their unmet needs are and why they will benefit from the prescription you have recommended for prosthetic or orthotic treatment, then you’ve done your job,” Bertram said.
Driving Outcomes, Advancing Patient Care
Nearly 30 years after giving his first talk on outcomes at an AOPA meeting, Robert Gailey, PhD, PT, FAPTA, was selected as the inaugural recipient of AOPA’s James H. Campbell Commitment to Outcomes Award, recognizing his pioneering contributions to evidence-based amputee rehabilitation.
Established in 2025 and funded by Hanger Inc., the award celebrates the accomplishments of James H. Campbell, PhD, CO, FAAOP, by celebrating those who advance evidence-based practice, implement clinical outcomes programs, contribute to peer-reviewed research, and drive innovation in outcomes-based product development.
Gailey’s creation of the Amputee Mobility Predictor (AMP) revolutionized functional assessment in prosthetics and remains the most widely used performance-based outcomes measure for individuals with limb loss today. He also co-developed the Comprehensive High-Level Activity Mobility Predictor (CHAMP), which has become a critical standard in military and high-performance rehabilitation programs.
James H. Campbell Commitment to Outcomes Award 2025 Winner: Robert Gailey, PhD, PT, FAPTA, University of Miami at the Miller School of Medicine
Sam
“Lessons Learned From a UPIC Audit” by Curt Bertram, CPO, FAAOP, and Lesleigh Sisson, CFo, CFm

“Dr. Gailey’s work has advanced the profession in immeasurable ways,” said Riley. “His commitment to data-driven care has improved access to prosthetic technology, informed policy, and transformed the lives of countless individuals living with limb loss.”
In addition to AMP and CHAMP, Dr. Gailey has contributed to the development of more than a dozen outcomes measures, including the PLUS-M, the Comprehensive Lower-Limb Amputee Socket Survey, and the Prosthetic Satisfaction Survey–13. Serving as a key thought leader in bridging prosthetics and physical therapy, Gailey has published more than 90 peer-reviewed journal articles and 25 book chapters, defining best practices in amputee rehabilitation and paving the way for evidence-based justification in coverage and clinical practice.
“Dr. Campbell used his influence within the profession to champion regular clinical use of outcomes and to effect the change that will benefit our patients, our practices, and our profession,” Gailey said. “I can’t tell you how much this means because I really have embraced this profession.”

Life-Long Impact
by over 300%, strengthening and expanding the residency program, and re-establishing UMOPC as one of the premier academic sites for O&P.
Having developed a statewide O&P provider network and becoming active in the O&P field, she also consulted and taught in areas of managed care, accreditation, business management, and other healthcare-related topics. Liberman-Lampear was part of the development team that worked with Eastern Michigan University to develop its O&P master’s program.
She was a board member of the Michigan Orthotics and Prosthetics Association, serving stints as its treasurer, chair of education, and liaison to Medicaid, as well as serving as a member of the Medical Care Advisory Council to the director Medicaid.

Liberman-Lampear also served on AOPA’s Government Relations Committee and spent several years as a member of AOPA’s Board of Directors. Notably, she was president of AOPA in 2013-2014. She, and the AOPA board and its spouses, developed the AOPA Wine Auction to raise money for the O&P PAC.
“This award is one of the highest honors a member of AOPA can receive,” she said. “To be listed with those who have received it before me is an amazing honor, and to be the first woman to receive this award is even more important to me. You have made my life’s work and achievements even more meaningful.”

A Legacy of Advocacy
With a remarkable career spanning over five decades, Don E. Hardin Jr. engaged with legislators and policymakers to address the most complex healthcare issues and trends impacting O&P.
Hardin, who died in April at age 89 following a battle with cancer, left an indelible mark on the O&P field. He was posthumously honored with the Ralph R. “Ronney” Snell, CPO, FAAOP, Legislative Advocacy Award, which recognizes individuals who have made valuable contributions toward advancing legislative and regulatory goals of the O&P field, motivating members of Congress and other decision makers to take action on behalf of O&P.
When Anita Liberman-Lampear, MA, became the assistant department administrator in physical medicine and rehabilitation at the University of Michigan Medical Center, she embarked on a career path that would leave a lasting impact on the national O&P landscape.
In September, Liberman-Lampear became the first woman ever bestowed AOPA’s prestigious Lifetime Achievement Award when she was recognized with the honor in Orlando for her significant contributions to the field of orthotics and prosthetics.
Charged with managing University of Michigan’s Orthotics and Prosthetics Center (UMOPC), she spearheaded a revitalization of the program, quadrupling her division in size and growing revenue
Starting in sales, Hardin’s career took him across the United States, Canada, Mexico, and much of Europe, introducing innovative technologies for companies from Camp to Truform and Tri Bar to Ottobock. His passion for being with people was evident in his participation in numerous international O&P industry and association events throughout the years, fostering lasting relationships within the industry.
“Don’s ability to truly connect with people, paired with his deep knowledge and unwavering advocacy, inspired countless professionals—including myself,” said his stepson Matt Swiggum, AOPA vice president and CEO of Proteor USA. “His leadership, integrity, and vision have left a legacy that will ripple through the prosthetics and orthotics community for years to come.”
AOPA President Rick Riley presents the Lifetime Achievement Award to Anita Liberman-Lampear, MA.
Don E. Hardin Jr.
In his later years, Hardin worked behind the scenes to influence policy makers and decision makers within the payor community, according to Brad Ruhl, retired former managing director, Ottobock North America. Focusing on reimbursement, access to care, and Medicare issues, Hardin also provided consulting services for small business owners in the O&P field.

Mary Hardin (center), accepted the Legislative Advocacy Award on behalf of Don E. Hardin Jr., who passed away in April, from AOPA Executive Director Teri Kuffel, JD (left), and AOPA President-Elect Kimberly Hanson, CPRH (right)
He served as president of AOPA in 1991-1992 and was presented with AOPA’s Lifetime Achievement Award in 2003. Throughout his career, Hardin served as a mentor to countless individuals and was an ardent advocate for those in need, taking an active role in organizations such as Challenger Little League (later OPAF), INTERBOR, and the International Society for Prosthetics and Orthotics.
Jennifer Davis is a contributing writer to O&P Almanac Reach her at jdavis@contentcommunicators.com
NEW THIS YEAR

2025 Student Poster Award Winners
Two talented students were honored for their meritorious scientific papers submitted for presentation as a poster at the 2025 AOPA National Assembly.
The Otto and Lucille Becker Award 2025 Winner: • “Sensor-Integrated Cranial Helmets” Anna B. Summers, Student, International Institute of Orthotics & Prosthetics
The Edwin and Kathryn Arbogast Award 2025 Winner: • “On the Beam and On the Clock: Balance and Gait Speed Relation in Upper- and Lower-Limb Amputees" Abdullah A. Alhuzaymi, PT, MSPO, PhD Student, University of Pittsburgh
Best in Show: New Products Showcase
Congratulations to the winners
Orthotics: First Place: Surestep Runner-Up: Icarus


Prosthetics, Upper Extremity: First Place: Metacarpal Runner-up: Aether Biomedical


Prosthetics, Lower Extremity: First place: Alps South LLC Runner-up: Blatchford



Documentation Guru
Reimbursement manager leverages
her
education and expertise to help patients navigate the complicated insurance landscape
The Fresh Faces column introduces readers to prominent O&P professionals who are making an impact with their contributions to the orthotics and prosthetics profession. This month, we speak with Brittany Gonzalez, CPO, reimbursement manager at Össur.
Brittany Gonzalez, CPO, reimbursement manager at Össur, started her career at Prosthetic and Orthotic Group in Southern California, where she worked as a clinician and eventually in a management role. In that capacity, she was passionate about fighting for insurance coverage for her patients and
recognized the importance of understanding medical policies to ensure her clinical documentation and coding decisions complied with payor requirements.
Gonzalez joined Össur in 2023, where she continues to advocate for O&P patients at work and through her involvement with several different O&P organizations.

O&P Almanac: How did you get involved in O&P?
Gonzalez: I was introduced to the world of O&P while studying biomedical engineering at Cal Poly, San Luis Obispo. During one of my introductory courses, Cameron Clapp spoke about his life as a person with bilateral lower-limb and right upper-limb amputations. I was so inspired by his story and how he was able to live such an active, fulfilling life, thanks to his prosthetic devices.
After his talk, I went home and researched the field of prosthetics and then volunteered at a local O&P clinic over the summer. I continued to be inspired by the patients I met and quickly realized that I wanted to pursue a clinical career in O&P so I could continue to work with these amazing patients every day.
O&P Almanac: What did you most enjoy about the time you spent in O&P clinical care?
Gonzalez: My favorite thing about clinical care was working with patients. Oddly enough, I always thought of myself as an introvert and wasn’t much of a talker growing up. However, I loved listening to patients’ stories and helping them in any way I could.
I worked at Prosthetic and Orthotic Group in Southern California for eight years,
Brittany Gonzalez, CPO
Gonzalez speaks with an attendee at the Össur booth at the AOPA National Assembly.
where I specialized in pediatric orthotics, and cranial remolding orthoses quickly became my passion. I truly loved working with children and babies, and I enjoyed connecting with their parents throughout the treatment process. Whether I was improving a head shape, treating scoliosis, or helping a child walk with more balance and stability, I was always motivated to improve the lives of every child and family I worked with.
O&P Almanac: What brought you to your current role as reimbursement manager at Össur?
Gonzalez: To be honest, it was my family. Although I loved working directly with patients, once my two beautiful girls were born, I felt a strong pull to be more present and available at home—so much so that I even considered being a stay-at-home mom. However, I wasn't quite ready to put my career on hold, so I decided to look for a remote position that would provide a better work-life balance for me and my family. I was always very interested in understanding medical policies and fighting for insurance coverage for each of my patients. But as time went on, I became increasingly frustrated with the O&P reimbursement system; it felt nearly impossible to balance increased audits and denials with decreased reimbursement rates. This frustration motivated me to find a job where I felt I could make a bigger impact.
O&P Almanac: What are your current responsibilities, and how did your previous work prepare you for your current position?
Gonzalez: While working at Prosthetic and Orthotic Group, I was given several opportunities to explore the many different nuances of running an O&P clinic. As a CPO, I learned how to make clinical arguments for medical necessity and gained a better understanding of insurance coverage requirements for O&P devices. I also spent a lot of time working with O&P students from CSUDH and developed a passion for educating other


Gonzalez gave a presentation at Children’s Hospital Los Angeles on cranial remolding orthoses.
practitioners. During my last few years in practice, I had the opportunity to manage three offices. I focused on improving office workflow efficiency and encouraged more collaboration between departments to optimize coverage for our patients.
My background as a clinician, educator, and manager opened my eyes to the real-world challenges faced by patients, practitioners, and administrative staff. I brought these insights with me to Össur, where I am responsible for providing reimbursement support to our customers, internal employees, and ForMotion clinics.
My day-to-day responsibilities vary widely, but often include documentation and appeal support, medical policy reviews, webinars, e-learning courses, meeting presentations, and internal training. I also assist with coding submissions for our products, and I enjoy collaborating with other industry experts to identify new ways to enhance access to O&P care.
O&P Almanac: Why is advocating for O&P patients a priority?
Gonzalez: Unfortunately, many insurance companies do not make it easy for patients to get access to the care they need and deserve. We continue to see an increase in audits and denials from all payors, and many O&P businesses don’t have the infrastructure or staff to support the increased
volume of appeals. I think it is essential to not only assist O&P clinics with this process but also help educate clinicians on medical policies and proper documentation to increase their chances of approval.
I also believe it is important to help patients understand their own insurance plans and potential options for better coverage. For example, Medicare Advantage plans often make it more difficult to get coverage than fee-for-service Medicare plans, and some insurance plans have specific exclusions for powered and/ or microprocessor prostheses. If patients are aware of these limitations during open enrollment, they may have the opportunity to choose a different plan with easier access and/or better O&P coverage. As experts in the field, I believe it is our responsibility to advocate for our patients and help them navigate the complicated insurance landscape, whenever possible.
O&P Almanac: What do you enjoy most about working for a manufacturing company?
Gonzalez: I really enjoy being exposed to so many different facets within the O&P industry. While I am still heavily involved with helping clinical practices navigate the world of reimbursement, it is also exciting to help launch new, innovative technology. I’ve learned so much about the Pricing,
Gonzalez presented Medicare updates at the Ancillary Revenue Conference in Denver earlier this year.
Data Analysis, and Coding verification process and how new Healthcare Common Procedure Coding System (HCPCS) codes are created, both of which are essential to ensuring access to and reimbursement for our products.
O&P Almanac: How have you been involved in AOPA over the years, and what other organizations are you involved in?
Gonzalez: I was a part of the AOPA Coding & Reimbursement Committee for two years before I started working at Össur. During my time on this committee, I helped review new products and recommend appropriate coding. I was also lucky enough to help submit a request to the Durable Medical Equipment Medicare Administrative Contractors (DME MACs) to expand coverage for osteoarthritis (OA) knee orthoses. Almost two years later, the DME MACs accepted the request and recently proposed changes to the Local Coverage of Determination to allow coverage for patients without knee joint laxity. It was such an honor to be part of this process and learn about the hard work that goes into changing policy and expanding coverage for our patients.
Currently, I am on AOPA’s Committee for Access, Representation, and Empowerment. We strive to bring awareness to diversity, equity, and inclusion issues within the field of O&P, and we help practitioners address these complex topics within their own practices.
I am also a member of the California Orthotic and Prosthetic Association’s Government Affairs Committee, where we explore opportunities to increase access to O&P care within the state of California. Most recently, we joined the So Every BODY Can Move initiative and hope to expand coverage for activity-specific orthotic and prosthetic devices.
Additionally, I am a member of the DME MAC Jurisdiction C and D Councils. I participate in quarterly meetings, where we receive updates from Noridian/CGS, Medicare auditing entities, and the DME MAC medical directors.
O&P Almanac: What piece of advice about reimbursement and coding would you like to share with O&P clinicians?
Gonzalez: Documentation is key. Although it is impossible to avoid pre- and postpayment audits, having strong, patient-
focused documentation will drastically increase your chances of avoiding denials and winning appeals.
I often see generic, templated arguments for medical necessity that focus on what the device can do as opposed to what the patient actually needs based on their day-to-day activities. And since most insurance policies specifically state that they will only cover the most basic device that meets the patient’s needs, this often leads to denial. The medical records must not only show that the patient meets the payorspecific coverage criteria, but they also must clearly explain how the unique features of the recommended device are necessary to meet the patient’s individual medical and functional needs. Every patient is unique, and therefore, no two arguments for medical necessity should be the same.
I also believe that providers play an important role in the creation of new HCPCS codes. When a new code is requested, CMS reviews several different factors, including utilization. If there is minimal billing for a new product, CMS may decide that there is not enough need to justify the administrative burden of creating a new code. Furthermore, historical billing data is used to help determine appropriate payment for

PHOTO: Brittany Gonzalez, CPO
Gonzalez took part in the SEBCM Leadership Roundtable at AOPA’s 2025 National Assembly in September.

Gonzalez created an e-learning course on appropriate documentation for the recent Medicare coverage expansion for K2 patients.
the new code. Unfortunately, many practitioners do not want to provide innovative products because they are forced to bill with a miscellaneous code until a new code is created. This not only delays the process but may even prevent the approval of a new code altogether due to a lack of utilization. If you want to support the advancement of O&P solutions, it is important not to shy away from purchasing and billing for new devices that are appropriate for your patients. Although there may be some short-term risk, it is essential for establishing long-term coverage and reimbursement to ensure patient access to state-of-the art orthoses and prostheses.
O&P Almanac: What are the biggest challenges and opportunities for the future of O&P?
Gonzalez: One of the biggest challenges right now is getting fair reimbursement and coverage for our work. The increased audits and denials, along with the low reimbursement rates, make it increasingly difficult for O&P companies to keep their doors open. However, we must continue to fight back against insurance companies by consistently appealing wrongful denials and renegotiating outdated payor contracts. Furthermore, recent HCPCS coding decisions show a preference for creating codes with broad, generic language that encompass a wide range of products.



This ultimately restricts the ability to bill separately for more advanced, innova tive products and features. Again, we must continue to push back against CMS with increased research and outcome measures to show the clear benefits of these products that deserve appropriate
With that being said, I also think that there are a lot of opportunities right now in the O&P industry. Along with the proposed OA knee brace coverage expan sion I mentioned previously, Medicare also expanded coverage for fluid, pneumatic, and microprocessor knees on K2 patients in September last year. Although commercial and state insurance plans are not required to follow Medicare coverage requirements, these policy changes increase the likelihood that other insurers will also expand their coverage in the future.
At the state level, the Move initiative is gaining a lot of momen tum, with 12 states successfully passing legislation so far to expand coverage for activity-specific orthoses and/or prosthe ses. Their goal of passing legislation in 28 states by the 2028 Paralympics in Los Angeles will open up the opportunity to push for the same coverage expansion at the federal level. While we continue to fight against the many day-to-day challenges within the O&P industry, these recent expansions in coverage provide hope for a better future where all patients have access to the care they need.












Racing Toward Recovery
Florida prosthetist helps author and speaker recover from two amputations and train for races

The Transformations column features the success story of an O&P clinician who has worked with an inspiring or challenging patient. This issue, we speak with Cara Negri, CP, LP, FAAOP, who assisted a patient through recovery of both transtibial and transfemoral amputation.
Cara Negri, CP, LP, FAAOP, doesn’t mind going to work on a Saturday. Creating new devices. Exploring different ways to restore mobility. Watching people take their first steps after a traumatic injury or life-changing surgery. It’s not like a regular job. Who wouldn’t want to go in on a Saturday?
She particularly enjoys patients who learn alongside her and want to work as partners to achieve shared goals. When she met Rebecca Denae, a young woman who chose amputation—twice—to preserve the active lifestyle she loves, a unique alliance was forged.
“Rebecca has an amazing attitude and spirit,” Negri says. “She’s wanting to live life to fullest and do what she wants to do, and these are the kinds of people who make this not [feel like] a job. I feel lucky we get to do this, and I get to be part of it.”
A Lifelong Ambition
Negri, clinical director at Gainesville Prosthetics, fell in love with a book about a girl with a prosthesis when she was in fourth grade. She checked it out so frequently, her school librarian gave it to her at the end of the year. When her high school had a job shadowing program, she was assigned to spend the day on the job with a prosthetist and felt she had pinpointed her future.
Rebecca Denae
Rebecca Denae (left) Cara Negri, CP, LP, FAAOP (right)

Determined to Succeed
“I said, ‘This is for me.’ We build things and they help people regain mobility. It blended everything that I loved—medicine, engineering, and art.”
She volunteered at that clinic, Bremer Prosthetic Design in Flint, Michigan, throughout high school and college, working her way up to be a prosthetist’s assistant. In college, she completed a co-op program, studying mechanical engineering for three months, then working in prosthetics for three months until she graduated.
Two weeks after she earned her mechanical engineering degree from Kettering University, she began the prosthetics certification program at Northwestern University, returning to Bremer for her residency training.
Her complementary interests in research and product development spurred her to work for a manufacturer, and she spent eight years in research and development for Össur, in North America, Iceland, and Australia. Once she returned home to the U.S., Negri got back into patient care and teaching. She also worked on a pet project developing video analysis tools to help clinicians evaluate gait, improve the patient experience, and facilitate documentation of clinical decisions.
“It’s been a whirlwind, but awesome,” Negri says. “I’m lucky to have found something I’m still very passionate about.”
Denae, now 25, was diagnosed with Stage III Ewing sarcoma in 2019 at 18 years old. Her surgeon removed a large tumor and half her tibia, replacing it with cadaver bone. Despite chemotherapy, physical rehabilitation, and warnings she may never walk unassisted again, Denae was climbing the local lighthouse steps near her home in Florida 10 months after her surgery.
Reclaiming her active lifestyle, she got into kickboxing and jiu jitsu. One of her coaches dared her to try a Spartan Sprint, a 5K race set with 20 obstacles. Two years after her cancer treatment, she triumphed in the Spartan Sprint and set even loftier goals. Nine months later, she embarked on
a Spartan Trifecta Weekend, completing a 21K, a 10K, and a 5K over two days.
Denae relished these physical challenges, but not long after the Spartan Trifecta weekend, the bone graft and metal plate in her reconstructed leg gave out from her intense level of activity. Her surgeon recommended a second limb-sparing surgery but warned her that racing—and walking—would be in her past.
Denae fought hard for another option, unwilling to concede her ability to be active. When the possibility of amputation was introduced, she saw it as a way forward and set out to find the right prosthetist to assist her in her recovery. She walked into Gainesville Prosthetics, on crutches and without an appointment, and started asking Negri questions.
“The thing that blew my mind was she was the first person who sat down with me and asked what I wanted my life to look like and what my job was like so she could design a leg for my lifestyle,” Denae says. Negri “spent so much time asking about my hobbies and interests, and she was completely undaunted.”
Nonlinear Recovery
Negri was prepared to advocate for Denae’s wishes, but the two didn’t agree on every aspect of her care.
Denae wanted to bypass a transtibial amputation and pursue transfemoral amputation from the start. Negri and Denae’s surgeon both felt he should try for a transtibial amputation to preserve her knee, yielding better function and an easier rehabilitation.

Denae (center) was able to compete in a Spartan 5K race 10 months after her first amputation.

Denae got the transtibial amputation in 2023 and recovered well. She completed her first Spartan 5K as an adaptive athlete 10 months later. However, foreign metal and bone left behind in her residual limb began causing her discomfort, necessitating another amputation above the knee to remove the foreign materials and keep Denae active.
“It was bittersweet,” Denae says. “There’s grief over time we lost, but I gained so much experience, and I got a lot less discouraged.”
Her second amputation occurred in 2024. Her primary goal was to avoid using a wheelchair as much as possible. Negri wanted to set her up for post-op success: “Thinking outside the box and not putting any limitations on it—that kind of fuels me to say, ‘Why not? Let’s figure it out and make it happen.’”
She crafted an immediate post-operative device for Denae from a casting brim. The long socket allowed her to bear weight through ischial tuberosity, but prevented any distal contact to the residual limb, protecting Denae from bumps and further injury while she healed.
While less comfortable than the permanent weight-bearing socket she eventually received, the post-op casting brim allowed Denae to stand immediately—even with
staples in her leg, bear weight, and avoid the mental toll of weeks to months in a wheelchair or on crutches.
“In my opinion, we should be doing this for everyone, all the time,” Negri says.
A Reciprocal Relationship
After Denae’s first amputation, she was walking independently in three weeks. The second time around, the process took three months.
While coping with the loss of stabilizing muscles, trying different knees, and adjusting to bearing weight was more physically demanding, her prior experience recovering from the transtibial amputation left her feeling more prepared and confident.
“Mentally it was easier the second time,” Denae says. “Physically, it was harder … but we did really good after that second amputation.”
She recently received a running blade from Össur’s Challenged Athletes Foundation and is working her way back to racing, hoping to be competition-ready in about six months. In the meantime, she remains focused on education and advocacy efforts. As a speaker and author, Denae shares her experiences to break the stigma that amputation is “the end of life as we know it.” She
teaches students and professionals in healthcare fields how to be better providers and advocate for their patients, and she helps patients learn the importance of educating themselves and voicing their needs and wants.
“That’s something that bonded us early on,” Negri says. “Rebecca is always very willing to put in the effort to learn about whatever is going on. She’s not just a passenger, she’s actively learning and understanding how [her prosthesis] works and what adjustments might make it feel better.”
Denae says Negri deserves credit for teaching her about the mechanics of prostheses, drawing on white boards and bringing in models to help her understand how different adjustments would impact her comfort and mobility.
“She’s the kind of person who will spend as much time as possible to make you as comfortable and functional as possible,” Denae says. “It’s a really special relationship working with someone so closely who understands your goals and dreams in life and is helping to get you there. I consider her my friend, if not my sister.”

Denae is focused on education and advocacy, sharing her experiences as a speaker and author.
Denae says her relationship with Negri is beneficial because Negri understands her goals and dreams, and helps her prepare to reach them.
Technicians
Choose Restech+ For Crystal-Clear Cosmetic Resin Laminations



Fast Curing Time
Easy 2:1 Mixing By Volume
Superior Toughened Resin Matrix
Crystal Clear High Luster Finish
Vacuum Socket Certified & Tested
Imperceptible Shrinkage
2 Year Shelf Life





FACILITY: Advanced Prosthetics OWNER: Mobility Ideal Health Group



PWhy Am I an AOPA
Member?
“We find that being an AOPA member not only gives us financial discounts, but keeps us abreast of the latest news and updates in our field.”
—Ken Gavin, CO
LOCATIONS: Greenville, Columbia, Anderson, Greer, Spartanburg, and Easley, South Carolina; Gastonia, North Carolina
Carolina Care
HISTORY: 27 years
Patient-care facility is an active contributor to surrounding communities
hillip Peters, CP, lost his right leg below the knee when he was just 15. He had had an anterior cruciate ligament injury from playing football, and a too-tight cast cut off circulation, leading to amputation. Peters pursued a career in prosthetics so that he could help other individuals with limb loss. In 1998, he and his wife, Miriam Peters, opened their own facility, Advanced Prosthetics, in Easley, South Carolina.

“It was one tiny office—the two of us and a secretary,” says Miriam, who is a certified mastectomy fitter. She had been part of the prosthetics department at Shriners Hospital in Greenville and is chief executive officer of Advanced Prosthetics.
The business slowly expanded, opening a second facility after a couple of years, and five more after that. “We looked at the local demographics and talked to patients to decide where to locate,” says Miriam. “We found that older people, especially, liked to stay in their local area to get care, so we focused on small communities outside of larger cities. We went to nursing homes, developed good relationships with doctors and physical therapists, and hired good people.”
Advanced Prosthetics recently became a subsidiary of Mobility Ideal Health Group but will continue to operate under its own name. Ken Gavin, CO, president of Mobility Ideal Health, along with current management, will be leading the company.
Nearly 50 employees, including nine clinicians, work for Advanced Prosthetics, which offers orthotic, prosthetic, and mastectomy care. Services also include compression garments and diabetic shoes and inserts. The company treats all ages, and a mix of upper- and lower-extremity and vascular and traumatic amputees.
“One thing that sets us apart is that we have several amputees on staff, including Phillip,” says Miriam. “Our company slogan is ‘Amputees Serving Amputees,’ and we feel that extra level of understanding is key to our success. It creates a personal connection and gives patients confidence in their providers and the comfort of knowing that they are truly understood.”
The facility uses advanced components, such as Össur’s i-Limb bionic hand, and has tried such newer technologies as 3D printing and CAD/CAM.
To assess outcomes among patients, practitioners evaluate functional mobility and safety, as well as the effectiveness and timeliness of the insurance process, care, and delivery. Phillip Peters notes: “We look at patient experiences with staff, location, and satisfaction with the device, as well as effective cost management. With feedback from our patients, we’ve been able to identify areas for improvement.” Measurements of patient progress focus on integrating care with the care teams to ensure unbiased outcomes. “We listen to feedback from the entire care team, patients, and our practitioners.”
The facility is an active member of the communities in which its offices are located. Staff members are encouraged to participate in charitable activities. Each office chooses a cause, and many employees participate in walks and other fundraising events.
Miriam knows a number of patients she met at Shriners when they were children who now need adult care. “One of them, whom I’ve known since he was a kid, had a congenital limb loss, below the elbow, on one arm,” she says. “We fitted him at Advanced Prosthetics for the i-Limb, and he got a job driving trucks. He’s out there trucking every day, and his arm is working great. It’s always a pleasure to see him.”
“As we progress further into the integration with Mobility Ideal Health, we will improve corporate decision-making and performance standards for each employee and manager,” notes Gavin. “We are also developing growth strategies and operational plans, both corporately and locally, as well as improving our financial planning. We want to focus on our brand, patients, people, referrals, and community, as our best work is done for our patients and referrals when we focus on their needs.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net
A technician fabricates customized prosthetic sockets.
Lydia Morris, CO, works with a patient at Advanced Prosthetics.
Miriam Peters, CFm, and Phillip Peters, CP, founders of Advanced Prosthetics
Adam Fitzpatrick, CPO, adjusts a patient’s prosthesis.
WORK SMARTER, NOT HARDER
microprocessor knee
The Icon microprocessor knee offers a user-friendly experience for patients and clinicians. Featuring responsive sensors, streamlined setup, and the intuitive Stride Studio app, this dynamic knee was designed to enhance user confidence. Clinicians can easily access all adjustments, custom modes, and more in Stride Studio. Equipped with a longlasting battery and IP68 rating, the Icon is the versatile solution for low to high activity users.









microprocessor foot
The new Odyssey® iQ is a hydraulically dampened microprocessor foot that is lightweight and incredibly low-profile. With an IP67 rating, long-lasting battery, and fast responses, it accommodates a wide range of users and activities. It also features simple setup and a unique method of spring-assisted dorsiflexion. Patients and clinicians can access valuable functions in College Park’s Stride Studio app.


OWNER:
The Family of Founder Noel Murphy

Bryan Schloss, director of sales and marketing; Olive Gunning, chief executive officer; and Kristi Huddleson, national sales manager—breast care at AOPA’s 2025 National Assembly

A patient wearing Trulife’s newest anterior-shell, carbon-fiber AFO
Why Am I an AOPA Member?
“We recently rejoined AOPA because we want to operate within this wonderful community of professionals who serve amputees across the country. We’re pleased that AOPA has recognized the topic of providing breast-care services. We enjoyed teaching our breast-care class and having our breastcare kiosk at this year’s National Assembly in Orlando, and we look forward to doing it again in Las Vegas in 2026.”
—Bryan Schloss
BY DEBORAH CONN
LOCATIONS:
International Headquarters: Dublin, Ireland; U.S. Headquarters: Jackson, Michigan; and Several Manufacturing Facilities
HISTORY: 67 years
Global Coverage
O&P manufacturer started with breast-care products and expanded to encompass all of O&P
Orthotic and prosthetic manufacturer Trulife dates back to 1958, when Walter Kausch developed a breast prosthesis in Detroit, Michigan. Noel Murphy acquired the company in 1987 and, through a series of acquisitions, expanded to encompass the full range of orthoses and lower-extremity prostheses. “These acquisitions added to the extensive breast-care product offering that we see Trulife manufacturing today,” says Bryan Schloss, director of sales and marketing.

industries,” Schloss says. TES’s clients include SpaceX, Boeing, and Lockheed Martin. “Our company uses the same highly technical manufacturing machinery that produces Trulife lower-limb prosthetic devices and componentry to also produce advanced aerospace and military products.”
Trulife’s 400 employees are located in Ireland, the United States, England, and Canada, with international headquarters in Dublin and U.S. headquarters in Jackson, Michigan. Trulife’s manufacturing facilities are located in Bellingham, Washington; Trenton, Canada; and Sheffield, England.
“Our state-of-the-art factory in Dublin manufactures our external silicone breast prostheses,” Schloss says. “We are one of only three global manufacturers in this space, and so we are strongly positioned in the breast-care arena.”
Over the years, a series of acquisitions—Camp Healthcare, Seattle Systems, and the United States Manufacturing Co.—expanded Trulife’s capabilities as an O&P manufacturer and increased its customer base. “When Trulife acquired Camp Healthcare, we acquired our largest distributor in the world, securing our U.S. business for the last 40 years,” Schloss says. “We also learned from our Camp Healthcare history that a focus on education is key. When you learn about products from the company that manufactures them, you will continue to buy from that company, and you will tell your colleagues in the field about your positive experience.”
Another acquisition further expanded Trulife’s reach. “About 10 years ago, we purchased and rebranded a company called TES, Trulife Engineered Solutions, which caters to the aerospace and military
Trulife’s lower-limb prosthetic devices and components “are proudly made in the United States, in beautiful Bellingham, Washington,” Schloss says. The company’s carbon-fiber ankle-foot orthoses— which it has been producing for 30 years—are made in its Sheffield, England, manufacturing facility.
The company sells its products exclusively through a network of more than 300 distributors that serve more than 100 countries around the world. “We rely on our distributors and very much value our relationships with them,” Schloss says.
Trulife also develops its relationships with O&P patient-care facilities in partnership with its distributors. “We ask the O&P facility up front which distributor they prefer,” Schloss explains, “and we work with the local rep of that distributor to support the needs of the O&P facility.”
Recently, the company teamed up with Steps of Faith, a nonprofit that helps individuals afford prostheses. “We will be providing them with Trulife products at a heavily discounted price,” says Schloss. “We’ve also partnered with Cascade to provide nonprofit Limbs for Life with free prosthetic equipment.”
As O&P products and technology evolve at an accelerating pace, “Trulife will continue to be on the forefront of technological advancements in both the materials we use and the machinery that makes our products,” Schloss says. “We have one of the most robust O&P research and development departments in the world.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net
An artisan at Trulife’s Bellingham, Washington, facility crafts the finishing touches on a foot shell.

View Virtual Assembly Content Until Nov. 25

Sign Up for the Virtual Coding & Billing Seminar in November
AOPA will host the last coding and billing seminar of the year Nov. 17-18, from noon to 4 p.m. each day. The seminar will be virtual.
Designed to equip O&P professionals with the tools and knowledge to excel in today's dynamic reimbursement environment, the seminar will offer 8.25 CE credits (attendance and quiz required).
Learn directly from O&P coding and billing experts as they help you:
• Navigate HCPCS updates and reimbursement policies
• Minimize denials and maximize reimbursements
• Master Medicare audits and appeals
• Strengthen coding and documentation best practices.
Don’t miss your chance to level up your coding & billing knowledge before the year ends! Visit AOPA's website for details and to register.
If you registered for the 2025 Virtual National Assembly, you have on-demand access to sessions covering clinical, business, technical, pedorthic and digital O&P care until Nov. 25. With a virtual-only registration, you can earn an estimated 80 CEs from the comfort of your home or office and get the latest from some of the best minds in O&P.
In-person attendees with full conference registrations can earn nearly 70 additional CE credits online post-event by attending the concurrent breakout sessions you missed on site.
Log on now to view sessions from the 2025 Assembly, but hurry—virtual access ends Nov. 25. Visit aopaassembly.org

It’s never too early to begin planning for the next AOPA National Assembly! Mark your calendars now for Sept. 9-12, 2026, when we’ll meet in exciting Las Vegas!
Looking for a new position? Seeking new employees?
Visit the AOPA Job Board on AOPA’s website to post an open position announcement or look for a new job. Visit jobs.aopanet.org.


The officers and directors of the American Orthotic & Prosthetic Association (AOPA) are pleased to present these applicants for membership. Each company will become an official member of AOPA if, within 30 days of publication, no objections are made regarding the company’s ability to meet the qualifications and requirements of membership.
Welcome New AOPA Members
Doctor in the House 721 Skippack Pike, Ste. 103
Blue Bell, PA 19422 610-277-1990, Ext. 151 docinthehouse.com
Scott Fried, DO Supplier Startup
Lehigh Valley Health Network
480 S. Cedar Crest Blvd., Ste. 200 Allentown, PA 18103 214-934-0112
Brian Spence, CO Patient-Care Facility
OandPServe LLC 26150 Oak Leaf Trail Excelsior, MN 55331 952-237-8489
oandpserve.com
Kevin Symms
Supplier Consultant
Prosthetic & Orthotic Associates of Tennessee (POA of Tennessee) 2116 McCallie Avenue Chattanooga, TN 37404 423-622-2000 poatn.com
Ronald Dickson, CP Patient-Care Facility
Proxy Health Partners 44 Christy Lane Manchester, NH 03104 603-837-6076
proxyhealthpartners.com
Keriann Catlaw Supplier Startup
Meracus® Pure composite Pure motion

Experience the power of pure composites with Allard’s new Dynamic Response Foot — Meracus®
Discover Meracus®


Precision Fit With Mt Emey® Custom Shoes
Embrace the comfort of custom-fit with Mt Emey®’s Custom Shoe (Medical) Program. Our precise 3D scanning captures your unique foot contours, promising a perfect fit without the wait or waste. From stylish athletics to roomy comfort designs, our handcrafted shoes adapt to your needs. Satisfaction guaranteed before payment. Plus, qualified wholesale accounts receive a free 3D scanner. Step into the Mt Emey difference— where every shoe is made for you.

Waterproof Terrain Foot From College Park
Navigate the bumpy road of life with comfort. The Terrain foot was created to achieve anatomical ankle motion and high energy return in a low-profile design. College Park uses its tri-axial technology expertise in a unique way. Versatile and service-free, the Terrain foot features a carbon fiber base and permanent bumpers inside the ankle housing for a progressive, comfortable response during low to high impact activities.
Learn more: college-park.com/terrain


For more information, call 1-888-937-2747 or visit emeys.com


Move with Confidence.
Aeris Performance LP
Aeris Performance LP – Fillauer
The Aeris Performance LP adds Compliant Composite Technology (CCT) that is derived by using multiple springs to increase the range of flexibility. The result is a unique Advanced Energy Release (AER) pylon design composed of nested parallel springs. This enables the foot to react in a compliant manner at heel strike and then work together to create a dynamic transition ... fillauer.com


Hersco Ortho App
Download the Hersco app on your iPhone and connect to the lab anytime. The Hersco app and order portal makes scanning and ordering seamless. Scan patients for foot orthotics, Richie braces, and ankle gauntlets, and submit at your convenience. Our digital workflow allows you to easily track jobs, re-order devices, and manage your account. Download the app and get your username and password.
Our 3D printers produce accurate and precise orthotics, reducing landfill waste by over 90%!
Email us today at fastorthotics@hersco.com or call 800- 301-8275 to get a free product sample. Visit hersco.com

Advertisers Index
COMPANY
A large number of O&P Almanac readers view the digital issue— If you’re missing out, visit AOPAnet.org to view your trusted source of everything O&P. Scan the QR to start advertising in the O&P Almanac
PAGE PHONE WEBSITE
Allard USA 9 866-678-6548 allardusa.com
ALPS South LLC 1 800-574-5426 easyliner.com
Apis Footwear Co. 15 888-937-2747 apisfootwear.com
College Park 39 800-728-7950 college-park.com
ComfortFit Orthotic Labs 3 888-523-1600 comfortfitlabs.com
Fabtech Systems 37 800-322-8324 fabtechsystems.com
Ferrier Coupler Inc. 10 810-688-4292 ferrier.coupler.com
Fillauer Cos. 17 423-624-0946 https://fillauer.com/products/motion-foot-six/
OrthoFeet Inc. C4 800-524-2485 https://orthofeet.shoes Performance Orthotic Laboratories 27 973-523-8610 performlab.com
TurboMed Orthotics 21 888-778-8726 turbomedorthotics.com
Contact Bob Heiman at bob.rhmedia@comcast.net
Monthly Events
ABC: Application Deadlines, Exams Dates, O&P Conferences, and More! Check out ABC’s Calendar of Events at abcop.org/calendar for the latest dates and event details, so you can plan ahead and be in the know. Questions? Contact us at info@abcop.org or visit abcop.org/contact-us

Live and Online/On-Demand CEs
The Pedorthic Footcare Association: The Active Foot—From 1st Step to Last! 10-session online education program series. Approved CEs by ABC and BOC, monthly classes are 2 hours each. For more information and to register, visit pedorthics.org.
November 17-18
Virtual Coding & Billing Seminar. For more information, visit aopanet.org

For Job Seekers:
Job searching is easy with the pane-view job search page. Set up job alerts, upload your resume or create an anonymous career profile that leads employers to you.
For Employers:
Reach 4,500+ O&P professionals through the Job Flash™ email. Ensure high visibility for your open positions through this highly engaging email.
2026
January 9–11
2026 Leadership Conference. Huntington Beach, CA. For more information, visit aopanet.org

March 6-15
2026 Paralympic Winter Games
Milano and Cortina, Italy. Visit teamusa.com/ milano-cortina-2026/paralympic
September 9–12
AOPA National Assembly. Las Vegas, NV. For more information, visit aopanet.org
2027
September 22–25
AOPA National Assembly. Long Beach, CA. For more information, visit aopanet.org
Finding your next job or hire just got easier with the AOPA Career Center.







Advocates in Action
Read this roundup of key O&P-related activities underway in several states
Colorado
Several AOPA members provided comments during this year’s Colorado Medicaid Provider Rate Review Advisory Committee’s (MPRRAC’s) quarterly public meetings for rate reviews of durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS). With testimony from AOPA members and other information, MPRRAC is recommending the following for Colorado Medicaid:
• “Prosthetics: Bring any codes below 80% of the Medicare benchmark up to 80%. All other codes remain as is.”
• “Orthotics: Bring any codes below 80% of the Medicare benchmark up to 80%. Leave any codes above 80% where they are. For codes without benchmark rates, increase 3% to account for inflation.”
Any changes due to the MPRRAC’s recommendations to the Colorado Medicaid schedule would be seen in July 2026 after a legislative process. Thank you to all who provided their expertise and advocacy.
Kentucky
The Kentucky Orthotic and Prosthetic Association is gathering support and planning advocacy around Medicaid coverage for orthotics and prosthetics and So Every BODY Can Move legislation. Kentucky residents can visit https://p2a.co/QuL7DKC to email their state legislators to show support for these efforts. To get more involved, email Kristy Young at kryoung@hanger.com
Mississippi
The revitalized Mississippi Prosthetic and Orthotic Association will host its inaugural meeting on Nov. 6 from 3:30 to 5 p.m. CST. During the first meeting, elections will be held for officer positions. If you would like to get involved, please contact Larry Word, CPO, FAAOP, at lword@mmrcrehab.org
New Jersey
New Jersey’s Medicaid fee schedule has been increased. Previously, New Jersey Medicaid DMEPOS rates were at 48.2 % of the Medicare rate in 2024. The updated Medicaid fee schedule reimburses at 70% of the current Medicare rate. Two codes, L5856 and L7181, are reportedly now on the Medicaid fee schedule.

So Every BODY Can Move
• In Massachusetts, the So Every BODY Can Move (SEBCM) bills, H4549/S811, were reported favorably by the Committee on Financial Services and have been referred to the Joint Committee on Health Care Financing. Massachusetts residents can fill out this link (https://p2a.co/tdM43jT ) to email legislators on the Joint Committee on Health Care Financing.
• At AOPA’s 2025 National Assembly, enthusiastic advocates took part in SEBCM -related events, including a Leadership Roundtable, a happy hour event, and a So Every BODY Can Move Activation Celebration. More than 200 attendees were present for the Activation Celebration.
Start earning your CE Credits
AOPA 2025 National Assembly Virtual Access is now open and earn even more at aopanet.org/education-ce/aopaversity-learning-center/.

100+ TOP-QUALITY ORTHOTIC, PROSTHETIC, AND PEDORTHIC EDUCATION COURSES.
EARN SCIENTIFIC, BUSINESS, AND PEDORTHIC CE CREDITS BY STUDYING THE COURSE MATERIAL AND PASSING THE QUIZ.
ACCESS YOUR PERSONAL ACCOUNT, VIEW VIDEOS, PRINT CERTIFICATES, OR REVIEW CE CREDIT HISTORY 24/7.