
Up to 12 months of optimal performance with 20% less product needed than Juvéderm® Volbella
balanced volume and high flexibility
patient and partner satisfaction



Up to 12 months of optimal performance with 20% less product needed than Juvéderm® Volbella
balanced volume and high flexibility
patient and partner satisfaction

Dr Saba Raja discusses how psychology affects
Enhanced navigation makes it simple to browse by category, filter by brand and quickly access our latest offers.
A significantly improved mobile experience, making it easier to browse, shop and manage e-Pharmacy orders on the go.
Clearer visibility of our full brand portfolio and complete product ranges.
A faster, more streamlined checkout experience that lets you complete multiple orders at once while still meeting all compliance standards.













































































































































08 News
The latest product and specialty news
19 News Special: The Impact of Weight-Loss Medication Misuse in Aesthetics
Aesthetics investigates the risks and repercussions of inappropriate weight-loss prescribing
20 Event Preview: The Next Step in Your Aesthetics Journey
How beginners, intermediate and advanced practitioners can tailor learning at ACE 2026
23 Special Feature: Treating Upper Arm Laxity Following Weight Loss
Three practitioners discuss the pathophysiology of skin laxity and evaluate treatment modalities
27 CPD: Exploring Regional Nerve Blocks in Head and Neck Aesthetics
Dr Ed Robinson examines the role of regional nerve blocks
32 Managing Post-Weight-Loss Skin Changes
Dr Ahmed El Muntasar presents an overview for managing post-weight loss skin changes
37 Recognising Skin Cancer in Aesthetic Clinics
Claire Amos investigates how aesthetics can play a role in skin cancer surveillance
43 Combining Radiofrequency and Polynucleotides for Scar Management
Megan Hope explores scar management using radiofrequency and PNs
47 Collagen: The New Chromophore
Lynton discusses the key benefits of the RedTouch Pro
49 Considering Regenerative Approaches for Ageing Hands
Mr Lorenzo Garagnani reveals his protocol for rejuvenating ageing hands
52 Zemits: The New Paradigm in Body Contouring Zemits addressing cortisol belly with integrated technology
53 Abstracts
A round-up and summary of the latest clinical studies
57 Considering Psychodermatology Within Clinical Practice
Dr Saba Raja examines how psychological factors affect skin physiology
60 Exploring the Factors Behind Sustainable Clinic Growth
Danny Chavda outlines how clinic growth comes from structure, visibility and clarity
62 SEO Blind Spots in Medical Aesthetics
Jane Nriapia discusses how AI-written content influences practitioners’ online success
65 In The Life Of: Dr Glyn Estebanez
Dr Glyn Estebanez shares a day in his life in clinic and working with Allergan Aesthetics, an AbbVie company
66 The Last Word: Assessing Visual Tools
Dr Arti Singh debates how visual tools shape psychological state

News Special: The Impact of Weight Loss Medication Misuse in Aesthetics Page 19

Special Feature: Treating Upper Arm Laxity Page 23
Clinical Contributors





Dr Edward Robinson is an NHS anaesthetics doctor based in Cheshire. He specialises in skin and hair rejuvenation treatments and treating the male face. He is an associate member of BCAM and a key opinion leader for Arthrex and Sciton.
Mr Lorenzo Garagnani is a consultant hand and wrist surgeon and a founder of the OrthoPlastic Hand Unit at Guy’s & St Thomas’ NHS Foundation Trust in London, as well as honorary reader at the Faculty of Life Sciences & Medicine of King’s College London.
Claire Amos is a registered nurse, independent prescriber and clinical director of CLK Medical Aesthetics in Bridgend. Amos also leads Safer Aesthetics Training Academy and is registered with the NMC, BAMAN and JCCP.
Megan Hope is an aesthetic nurse practitioner and has a bachelors of science in adult nursing, qualifying in 2017 from Oxford Brooke’s University. Hope is the founder of MCH Clinic in Norfolk and codirector of The Nurses Network.
Ahmed El Muntasar is a UK-trained GP and aesthetic physician with extensive experience in non-surgical facial and body rejuvenation. He has a Bachelor of Science (BSc) in Medical Sciences and a Master’s degree in Medical Leadership from University College London (UCL).















Shannon Kilgariff Editor & Event Director @shannonkilgariff
Body weight loss and body contouring remain popular in aesthetic practice, but rarely have we seen the landscape shift as rapidly as it has over the past year.
In this issue of Aesthetics Journal, we explore how powerful new tools – and worrying new behaviours – are reshaping patient expectations, treatment planning and ethical boundaries.
Our Special Feature focuses on one of the most challenging, and often neglected, areas: upper arm laxity. With increasing numbers of patients achieving rapid weight loss, demand for effective solutions is rising. Our interviewees examine surgical and non-surgical approaches, skin quality optimisation and realistic patient counselling where expectations surpass what current techniques can safely achieve.
Alongside this, we turn a critical eye to GLP-1 receptor agonists and their impact on body contouring practice. As these medications
become more widely used for weight loss, we consider their effects on skin laxity, facial and body volume, and the timing and planning of aesthetic interventions.
Our News Special looks into the concerning recent news that some individuals have been using AI to exaggerate their appearance in order to secure a GLP-1 prescription. This development raises profound questions about verification, safeguarding and our role in promoting responsible, honest pathways to care.
Finally, we are delighted to reveal the Aesthetics Conference and Exhibition (ACE) agenda in this issue. Taking place on March 13-14 at the Business Design Centre, ACE is an ideal place to connect with peers, share experience and learn from leading experts. Our Event Preview highlights which sessions are best suited to beginner, intermediate and advanced practitioners, helping you to plan your time and get the most from the meeting.
ACE takes place next month, so do have a look at the programme and make sure you register by turning to p.20 – we look forward to seeing you there.
Leading figures from the medical aesthetic community have joined the Aesthetics Advisory Board to help steer the direction of our educational, clinical and business content

Sharon Bennett is the former chair of the British Association of Medical Aesthetic Nurses (BAMAN), UK lead of the BSI committee for aesthetic non-surgical standards and member of the Clinical Advisory Group for the JCCP. She is a trainer and a registered university mentor in cosmetic medical practice, and is finishing her MSc at Northumbria University. Bennett has won the Aesthetics Award for Nurse Practitioner of the Year and the Award for Outstanding Achievement.
Sharon Bennett, Clinical Lead



Mr Naveen Cavale has been a consultant plastic, reconstructive and aesthetic surgeon since 2009. He has his own private clinic and hospital, REAL, in London’s Battersea. Mr Cavale is the national secretary for the ISAPS, president of the Royal Society of Medicine, and vice-chair for the British Foundation for International Reconstructive Surgery.
Miss Elizabeth Hawkes is a consultant ophthalmologist and oculoplastic surgeon. She is the lead oculoplastic surgeon at the Cadogan Clinic, specialising in blepharoplasty and advanced facial aesthetics. Miss Hawkes is a full member of the BOPSS and the ESOPRS, and is an examiner and fellow of the Royal College of Ophthalmologists.
Mr Adrian Richards is a plastic and cosmetic surgeon with over 30 years’ experience. He is the clinical director of the aesthetic training provider Cosmetic Courses and surgeon at The Private Clinic. He is also a member of the British Association of Plastic and Reconstructive and Aesthetic Surgeons and the British Association of Aesthetic Plastic Surgeons.
PORTFOLIO MANAGEMENT
Shannon Kilgariff • Editor & Event Director
T: 0203 196 4351 | M: 07557 359 257 shannon.kilgariff@easyfairs.com
EDITORIAL
Holly Carver • Deputy Editor & Content Manager
T: 0203 196 4427 | holly.carver@easyfairs.com
Amer Saleh • Journalist | T: 020 3196 4270 amer.saleh@easyfairs.com
Mia Sawyer • Content Writer | T: 020 3196 4242 mia.sawyer@easyfairs.com
Sophia-Fai Roche • Journalist sophia-fai.roche@easyfairs.com | T: 0203 196 4391



Dr Mayoni Gooneratne (MBBS, BSc, MRCS, MBCAM, AFMCP) was an NHS surgeon before establishing The Clinic by Dr Mayoni and founding Human Health – an initiative combining lifestyle with traditional and functional medicine to provide a ‘cell-up’ regenerative approach to aesthetics. She is also the co-founder of The British College of Functional Medicine.
Jackie Partridge is an independent nurse prescriber. She is the clinical director and owner of Dermal Clinic in Edinburgh and a KOL for Galderma. She holds an MSc in Non-surgical Aesthetic Practice and a BSc in Dermatology. Partridge is a stakeholder group member with Scottish Government/HIS, Honorary BACN member and JCCP Fitness to Practice Nurse.
Dr Souphi Samizadeh is a dental surgeon with a Master’s degree in Aesthetic Medicine and a PGCert in Clinical Education. She is the founder of the Great British Academy of Medicine and Revivify London Clinic. Dr Samizadeh is a Visiting Teaching Fellow at University College London and King’s College London.
DESIGN
Aimee Bish • Senior Graphic Designer
Callum Benyon • Junior Graphic Designer
Aaron Smyth • Graphic Design Intern
ADVERTISING & SPONSORSHIP
Judith Nowell • Head of Sales
T: 0203 196 4352 | M: 07765 407629 judith.nowell@easyfairs.com
Charlotte Norville • Senior Sales Executive
T: 020 3196 4418 | Charlotte.norville@easyfairs.com
MARKETING
Susana Burguera • Senior Marketing Manager
T: 020 3196 4281 | susana.burguera@easyfairs.com
Ella Carey • Marketing Executive T: 020 3196 4410 | ella.carey@easyfairs.com
If you are interested in contributing to the journal, get in touch...
Email: editorial@aestheticsjournal.com

Dr Sophie Shotter is the founder & medical director of Illuminate Skin Clinic in Kent and Harley Street, London. Her passion is for natural treatments delivered with utmost attention to safety. She works closely with Allergan as part of their UK and International Faculty.

Dr Anjali Mahto is one of the UK’s leading consultant dermatologists. She is a Fellow of the Royal College of Physicians, member of the Royal Society of Medicine and a spokesperson for The British Skin Foundation. In 2023 Dr Mahto opened Self London, a dermatology and lifestyle clinic aimed at managing skin conditions holistically.

Dr Stefanie Williams is a dermatologist with a special interest in adult acne, rosacea and aesthetic medicine. She is the founder and medical director of multi-award winning EUDELO Dermatology & Skin Wellbeing in London, and creator of Delo Rx skincare. She is the author of three books and has published more than 100 scientific articles, book chapters and abstracts.
Material may not be reproduced in any form without the publisher’s written permission. For PDF file support please email, contact@aestheticsjournal.com
© Copyright 2026 Aesthetics. All rights reserved. Aesthetics is published by Aesthetics Media Ltd, which is registered as a limited company in England; No 9887184
Follow us on Instagram @aestheticsjournaluk
#Launch
Dr Priyanka Chadha @drpriya.plastics
A wonderful reception for Relfydess in Dubai, as I was met with open arms and open minds by some of the most engaging doctors and plastic surgeons.

#Education
Cosmetic Courses @cosmeticcourses

#Community TNN - The inclusive community of medical injectors @thenursesnetwork
The beginning of the year is the perfect time to bring our regional leads together to celebrate the exciting plans we have ahead for 2026!
A great training week in Ireland with our medical director and Cosmetic Course leads, always striving to elevate our knowledge and continue safe, high-quality practice.

#Networking
Dr El Mouttaki @dr.elmouttaki
Honoured to be among the top hair transplant surgeons in India at the amazing FUE Asia Conference 2026!

#International Louise Prothero @sciton_louise
Heading to Miami with Sciton to learn, grow and bring you best-in-class technology, innovation and education.

GLP-1 Medication
The US Food and Drug Administration (FDA) has approved weight loss drug Wegovy as the first once-daily oral GLP-1 weight loss pill. The FDA approved the first oral GLP-1 medication for chronic weight management in adults with obesity or overweight and related health risks on December 22, 2025, marking it as the first oral treatment of its kind in the US. The medication became available in US pharmacies and via telehealth providers from January 5, 2026. Currently, the approval applies only in the US, with regulatory decisions in other countries, including the UK, still pending.
Developed by Danish pharmaceutical company Novo Nordisk, the Wegovy tablet contains the same active ingredient, semaglutide, as the injectable alternative. The pharmaceutical company further outlines clinically meaningful weight-loss outcomes from late-stage trials. It reported that Wegovy produced an average weight-loss of 16% over 64 weeks and among 307 adult participants in a phase III clinical trial.
Ed Cinca, senior vice president of marketing and patient solutions at Novo Nordisk, commented, “The Wegovy pill is here, and it represents a significant innovation as the first and only GLP-1 pill for weight loss. This moment is about changing what’s possible in weight management, and to make that possible, we have worked to ensure Wegovy pill is affordable and accessible to those who need it, however they choose to receive their care.”
Dr Nestor Demosthenous, aesthetic practitioner and trustee of the British College of Aesthetic Medicine (BCAM), commented, “Oral GLP-1 therapies are a powerful tool, but they must be used responsibly. In medical aesthetics, they should sit alongside a muscle-centric nutrition and training programme to protect metabolic health and body composition. Safety is paramount, and prescribing should be undertaken only by medically qualified and registered healthcare professionals.”
Regulatory Approval
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved a new maximum weekly dose of semaglutide of up to 7.2mg.
The regulatory agency shares that this is designed to target weight management in adults with obesity, and states that the higher dose applies only to patients with a body mass index (BMI) of 30kg/m² or above. It also outlines that the stronger dosage must be used alongside a reduced-calorie diet and increased physical activity. According to the MHRA, the new maximum dose is administered as three consecutive 2.4mg injections on the same day, following a structured dose-escalation schedule.
The agency states that treatment begins at 0.25mg per week, with doses increased every four weeks under healthcare professional supervision until 2.4mg is reached. It further advises that, where clinically appropriate, the dose may be increased to 7.2mg after a minimum of four weeks at 2.4mg.
The MHRA further highlights that the approval does not apply to patients using semaglutide to reduce cardiovascular risk.
Aesthetics Awards

Broadcaster and television personality Rylan has been revealed as the host for The Aesthetics Awards ceremony on Saturday, March 14 at Hilton, Park Lane.
Rylan first rose to prominence as a contestant on The X Factor in 2012, where he reached the quarter finals, before going on to win Celebrity Big Brother in 2013. Since then, he has established a successful broadcasting career, fronting numerous television programmes, including Big Brother’s Bit on the Side, This Morning, Supermarket Sweep, and Strictly: It takes Two
The Aesthetics Awards represent a pinnacle moment in the specialty calendar, recognising outstanding achievements by companies, clinics and practitioners across the sector. Categories this year include the AlumierMD Award for Rising Star of the Year, the DermaFocus Award for Best Injectable Result and the Galderma Award for Best Clinic in South England.
Shannon Kilgarrif, editor and event director of Aesthetics, said, “Rylan brings a fresh, dynamic energy to The Aesthetics Awards, perfectly capturing the spirit of innovation and creativity that defines our specialty. We’re excited to have Rylan guide us through an evening dedicated to recognising the best in medical aesthetics.”
Regulatory Reminder
The Committee of Advertising Practice (CAP) contacted trade bodies and regulators to remind their members that promoting prescription-only medicines (POMs) is prohibited under both the advertising code and the law.
Its guidance also makes clear that POMs used in medical aesthetics, including botulinum toxin and GLP-1 medications, must not be advertised to the public. It warns that breaches could result in suspension or revocation of a licence to practise.
Ed Senior, senior compliance executive at CAP, commented, “We’ve written to various trade bodies and regulators to remind their members that promoting POMs to the public is against the advertising rules and the law. We won’t hesitate to take action where we do see the rules being broken. This may include applying our own sanctions, as well as informing other regulatory partners or trade bodies of any of their members that are breaking the rules so they can take appropriate action.”
Following this, organisations including the Nursing and Midwifery Council (NMC), the British Association of Medical Aesthetic Nurses (BAMAN) and UK training provider Harley Academy have issued reminders of the CAP guidance for its members.
Gareth Lewis, chief operating officer at BAMAN, commented, “In practice, this means nurses should avoid naming POMs in promotional posts, advertising botulinum toxin appointments, listing prices, offering discounts or time-limited deals, running giveaways or using before-and-after marketing where the clear purpose is to promote a prescription-only medicine-led treatment.”
Out of 500 women aged 18-75, 44% cite financial burdens as the biggest barrier to ‘feeling and looking their best’
(Oriflame, 2025)
Among 2,000 UK women aged 35+, 43% say their skincare routines are more complex than they were 10-20 years ago, yet 81% now prefer simpler routines (Olay, 2025)
Pressure from online beauty ideals has led 16% of 2,004 men and women to feel pushed toward botulinum toxin, with a further 13% feeling pressured to consider dermal fillers (Genaura, 2025)
Glutathione administration is predicted to be a popular treatment for 2026, driven by 9,903,000 google searches between December 2024-November 2025 (Fresha, 2025)
‘Treatment burden’ leads up to 40% of androgenetic alopecia patients to discontinue minoxidil within one year (Absci, 2025)
New data points to a growing public concern around skin cancer, following a 147% surge in searches for “melanoma mole” in December 2025 (LocalIQ, 2025)
5th February 2026
Future Patient Congress
6th February 2026
Menopause in Practice
13th-14th March 2026
Aesthetics Conference & Exhibition (ACE)
14th March 2026
The Aesthetics Awards
1st-2nd October 2026
Clinical Cosmetic Regenerative Congress (CCR)
Eleanor Hartley discusses safeguarding patients
In an episode of the Wednesday podcast, aesthetic nurse practitioner Eleanor Hartley joined co-host Melissa Tattam, where she spoke on the importance of practitioners declining treatment when appropriate. Hartley noted that, in some instances, both medical and non-medical practitioners prioritise commercial interests over clinical judgement. She revealed, “I am working on a framework that questions whether we should treat a patient based on the treatments’ long-term impact, how reversible the treatment is, how suitable the patient is, and the likelihood of good and bad outcomes.”
Dr Al-Zubaidi raises concerns surrounding GLP-1 medication
Appearing on BBC News, general practitioner Dr Hussain Al-Zubaidi describes the transitional period of stopping weight-loss medication as “Jumping off a cliff,” while warning that the food cravings can return as quickly as the next day. Dr Al-Zubaidi emphasised that appropriate support is essential, noting that patients who obtain the drugs privately do not always receive the support needed. He stressed the importance of a clear exit strategy, noting that without broader support and a shift in society’s relationship with food, lasting change is unlikely. Dr Al-Zubaidi concludes, “The environment that people live in needs to promote health, not weight gain.”
A review published in the British Medical Journal indicates that individuals using weight-loss medication may regain lost weight up to four times faster than those who lose weight through conventional diet.
The data indicates that individuals can lose around one-fifth of their body weight, but often regain it quickly once treatment stops. On average, patients regain about 0.8 kilograms per month, returning to their pre-treatment weight within roughly 18 months, according to the review.
The findings were drawn from 37 clinical trials involving more than 9,000 participants, comparing the effects of weight-loss injections with conventional dieting or other pharmacological approaches. By contrast, the review notes that individuals who lose weight through dietary changes alone tend to regain weight more slowly, on average around 0.1 kilograms per month, although rates vary between individuals.
Only eight of the studies evaluated newer GLP-1 drugs, including semaglutide and tirzepatide, with follow-up periods limited to one year after discontinuation.
Patient Safety
A consensus guideline for the management of tissue filler-induced vision loss has been published in the Aesthetic Surgery Journal (ASJ).
The guideline outlines clear recommendations on emergency management, access to specialist care, informed consent and awareness of vision-related risks associated with dermal fillers. Developed by a multidisciplinary steering group, the guidance recommends that practitioners performing tissue filler injections keep an emergency kit on hand to manage vision loss or ischemic complications. Practitioners are also advised to obtain explicit consent that includes the risk of vision loss and to promptly initiate appropriate non-invasive measures in cases of filler-induced vision loss to help dislodge an embolus and restore retinal perfusion.
Consultant ophthalmologist and vitreoretinal surgeon Mr James Neffendorf, who played a leading role in the multidisciplinary steering group, commented, “We have written this peer-reviewed publication to help injectors understand the risk of vision loss after dermal filler injections and provide guidance on management.”
Non-profit organisation the British Beauty Council has announced the return of the Great British Beauty Clean Up (GBBCU).
Commencing on March 2, the initiative returns with a developed focus aimed at driving a nationwide shift towards reusing, refilling and preventing product waste, according to the organisation. The British Beauty Council shares that the 2026 campaign promotes refillable systems, the donation or resale of surplus products to combat hygiene poverty and the repurposing of hard-to-recycle materials.
Victoria Brownlie, chief of policy and sustainability at the British Beauty Council, commented, “The 2026 GBBCU is about reimagining waste completely. Whether it is donating surplus stock to companies like In Kind Direct to help those in need, or using MYGroup to turn compacts into construction materials, we are asking the field to think more purposefully about closing the loop when it comes to packaging.”
The British Beauty Council will be speaking at The Association Zone at ACE. Turn to p.20 to register.

Aesthetics has unveiled the agenda for the Aesthetics Conference & Exhibition (ACE) 2026, taking place on March 13-14.
Returning as Headline Sponsor is Allergan Aesthetics, an AbbVie company, that will host sessions within the Allergan Aesthetics Auditorium. Allergan Aesthetics will also be supporting this year’s Meet the Mentor Speed Dating initiative. The Innovation Forum returns as the dedicated platform for forward-thinking developments in medical aesthetics, with Dermapenworld as Theatre Sponsor. Day 1 will feature sessions supported by AesthetiCare, BTL Aesthetics, Cure Medical, Hydrafacial, Klira Clinical, SkinCeuticals, Sofwave and iiaa. Day 2 will welcome Arthrex, Fotona UK and SR Biotech (Idenel).
Championing both the artistic and scientific foundations of the specialty, the Aesthetics Mastery Theatre will once again take centre stage, with DermaFocus confirmed as Lunchtime Takeover Sponsor on both days. Day 1 will hear from AestheticSource, BeautyEurope, Evolus, Healthxchange, Merz Aesthetics and S.Thepharm. Day 2 will feature IBSA alongside the renowned Aesthetics Challenge, which will explore pushing the limits of cannula mastery with key opinion leaders from Alma, Allergan Aesthetics and IBSA performing live demonstrations.
New for 2026 is the Cutting Edge Theatre, designed to spotlight pioneering theories and emerging concepts shaping the future of aesthetics. Sessions here will be supported by Croma, Cutera, Galderma and VIVACY.
Located within the Platinum Hall, the Association Theatre will focus on ethics, safety and the latest developments across medical aesthetics. Rounding out the programme, the In Practice Theatre will deliver practical business insights and solutions from leading practitioners. Phorest and Zenoti join as Associate Sponsors, while Cosmetic Courses will partner the Starting Strong in Aesthetics session. ACE Group World will once again partner for complications support. Additional sponsors bringing ACE 2026 to life include Dermapenworld as Networking Sponsor, Healthxchange as Registration and Lanyard Sponsor, HYPO21 as Skin Prep Partner and Initial Medical as Clinical Waste Partner. View the full agenda online. Turn to p.20 to register.
Collaboration
Aesthetic device company InMode Global has announced a business collaboration between InMode UK and aesthetic distributor Cure Medical. As a result of this global collaboration, InMode UK and Cure Medical will align their marketing and sales activities, operating as a unified commercial team in the UK. Alongside his role of managing director and CEO of Cure Medical, Adam Bashir has been appointed managing director of InMode UK. In this additional role, Bashir will lead the company’s commercial strategy, drive growth and further strengthen partnerships with surgeons, dentists, medical practitioners and clinics throughout the UK.
Bashir commented, “With InMode UK poised for the next phase of growth together with the complimentary portfolio of Cure Medical advanced skin solutions, I am excited. It is a very timely commercial collaboration, helping to achieve the critical mass needed to become the leading medical aesthetics company in the UK and Ireland.”
InMode and Cure Medical are both exhibiting at ACE on March 13-14. Turn to p.20 to register.
A round-up of the latest news and events from the British Association of Medical Aesthetic Nurses
We’re proud to share that the BAMAN Education & Training Committee has been shortlisted as a Finalist for The Zenoti Award for Best Initiative/ Strategic Project in Aesthetics at The Aesthetics Awards 2026!
The committee has worked with real purpose to raise educational standards, create meaningful opportunities and develop new partnerships that directly support the growth and professional development of our members. Congratulations also to all the BAMAN members who are nominated across the Award categories, and best of luck.
BAMAN’s board of directors and head office team came together on January 27 for a mini-strategy day to look ahead at 2026.
New initiatives are already underway to ensure members get the most from their membership, including the introduction of monthly BAMAN virtual member forums.
These informal sessions give members the opportunity to hear updates on what the BAMAN board and head office team have been working on, learn about current projects, ask questions, share feedback and explore more ways to get involved.
January also marked the first of our 2026 regional meetings, with our members in Kent gathering in Sevenoaks for a day of education, connection and professional development. They were joined by a selection of BAMAN’s strategic partners for 2026, with more to come across the regions throughout the year.
We’re thrilled to be working with an expanded group of partners in 2026, giving members access to big companies.
You’ll see them at upcoming meetings, supporting education, sharing insights and building valuable connections with the BAMAN community.
All upcoming regional meetings are listed on the BAMAN website – and are available to book onto via the QR code below.
This column is written and supported by BAMAN

Mentor Yogeeta Bawa explains how you can benefit from the Aesthetics Mentoring at ACE 2026

How can mentoring at ACE benefit different types of delegates?
As Warren Buffet famously said, “It’s good to learn from your mistakes. It’s better to learn from other people’s mistakes.” The mentoring sessions are an opportunity to learn from experts. It is an opportunity to ask questions around concerns, challenges and practical advice we all need at some point. This is relevant if you’re new to your aesthetics career or are more experienced. The specialty continues to evolve at a fast pace and the mentors can provide guidance and support to help navigate your steps.
In what ways can mentoring be beneficial compared to talks and workshops?
The unknown can feel intimidating, but it’s often where growth begins. Mentoring is for everyone, and regardless of your experience having a mentor is fundamental to always elevate yourself, as well as have a trusted person to ask questions, learn and navigate challenges with. Attending workshops and sessions is vital for continuous learning and knowledge, but a mentor is bespoke to your own journey, guiding and supporting you through your unique and individual goals. They can help you provide clarity, structure and practical advice, and tools to unpick the overwhelm. A mentor is like having your own cheerleader, they want to accelerate your growth and reduce roadblocks, and provide the confidence to excel in your continued success.
What should delegates prepare in advance so they can get the maximum value from their time with you?
This is a golden opportunity to have time with aesthetic experts, so come prepared. My advice is think about your desired outcome, then prepare five tailored questions to ensure you get specific answers to help support you.
Mentoring will take place over both days at ACE, on March 13-14. Get your complimentary space by scanning the QR code.
The US Food and Drug Administration (FDA) has updated its guidance regarding how it regulates certain health-related technology.
Under the revised guidance, a product may be classified as a general wellness product – rather than a regulated medical device – if it is intended to maintain or encourage a general state of health, or if it relates a healthy lifestyle to reducing the risk or impact of certain chronic diseases or conditions.
Among the examples cited by the FDA are wrist-worn wearable devices designed to assess multiple biomarkers, such as sleep duration, sleep quality, pulse rate and blood pressure. However, the guidance makes clear that if a product’s claims suggest use in a medical or clinical context – such as diagnosing, treating or managing a disease – it would no longer be considered a low-risk general wellness product and would remain subject to FDA regulation.
In a second guidance, the FDA announced changes to its approach to regulating clinical decision support (CDS) software. The agency indicated that certain types of software may resemble medical tools but are considered sufficiently low risk to fall outside active FDA oversight, provided they remain within defined boundaries.
In the guidance the FDA stated it will not regulate software that estimates a patient’s future cardiovascular risk based on established clinical factors such as weight, current and historical smoking status, blood pressure and brain natriuretic peptide (BNP) in vitro diagnostic (IVD) test results.

Aesthetic distributor Healthxchange has introduced a new technology-enabled ePharmacy.
The platform is designed to simplify how clinicians discover, purchase and manage products online. Replacing the company’s previous system, the platform features intuitive navigation, alongside advanced search and filtering, designed to improve promotions visibility and faster checkout. The company shares that the platform is optimised for mobile, and allows clinicians to order across multiple patients in a single transaction and access Healthxchange’s multi-brand portfolio, including injectables, skincare and devices.
CEO of Healthxchange Jack Curran commented, “This launch is about far more than a technology upgrade. As a clinician-founded business, we understand the pressures our customers face every day. The new ePharmacy has been purpose-built to save time, simplify decision-making and give clinicians confidence that they are shopping with the most trusted partner in aesthetics.”
Healthxchange will be exhibiting at ACE on March 13-14. Turn to p.20 to register.
Product Releases


Skincare company Obagi Medical has delivered both the Nu-Cil BioStim Scalp Serum and SUZANOBAGIMD Claribright Radiance Brightening Lotion.
Accessible through aesthetic distributor Healthxchange, Obagi Medical has expanded its Nu-Cil collection with a leave-in hair serum. The treatment is formulated with the brand’s proprietary BioStim Complex, combining biotin, amino acids and peptides, alongside biotinoyl tripeptide-1, niacinamide and panthenol to hydrate the scalp, strengthen follicles and improve hair elasticity.
Accompanying this is the SUZANOBAGI Claribright Radiance Brightening Lotion, developed by dermatologist and Obagi Medical chief medical director Dr Suzan Obagi. The formula targets uneven skin tone and dullness, featuring liposomal tranexamic acid, encapsulated phloretin and liposomal oligopeptide-68 to address pigmentation, support collagen production and enhance radiance, according to the company.
Simone Shoffman, education and clinical director at Healthxchange, commented, “Obagi has long been trusted for delivering scientifically backed skincare solutions, and with Nu-Cil BioStim Scalp Serum, it’s bringing that same expertise to scalp health. We’re also thrilled to introduce SUZANOBAGIMD Claribright Radiance Brightening Lotion, this beautifully balanced formulation delivers visible brightening and improved skin clarity without irritation, utilising slow release technology to deliver a synergistic blend of advanced brightening actives and antioxidants.”
Healthxchange will be exhibiting at ACE on March 13-14. Turn to p.20 to register.
Aesthetic manufacturer Teoxane presented a new injection technique for skin quality at the International Master Course on Ageing Science (IMCAS) Paris 2026.
Two scientific posters and a dedicated symposium detailed the Teoxane babyGLOW technique, a standardised, anatomy-based subdermal injection approach designed to support consistent product distribution while avoiding facial danger zones. The company explains that the method involves Teosyal Puresense Redensity 1, a non-crosslinked hyaluronic acid formulation with a dermostructuring complex, selected for its high fluidity and suitability for dermal and subdermal skin redensification.
Mounia Heddad-Masson, director of global medical education and medical affairs at Teoxane, commented, “At IMCAS our ambition is to bring our educational standards, clinical rigor and scientific vision directly to the heart of the global aesthetic community. Teoxane babyGLOW is a clear expression of this approach. The technique was developed in close collaboration with a board of more than 20 expert injectors across six countries and refined through real-world clinical practice.”
Distribution

Aesthetic distributor Wigmore Medical has announced the expansion of its distribution partnership with skincare company IMAGE Skincare.
Wigmore Medical will undertake exclusive UK distribution of the full IMAGE Skincare portfolio across medical, aesthetic, spa and beauty channels, as well as the brand’s direct-to-consumer platform, the company shares.
The expansion builds on the existing medical distribution partnership between the two companies. Wigmore Medical shares that it will now oversee nationwide distribution, professional education and practitioner support across all channels.
Raffi Eghiayan, CEO of Wigmore Medical, commented, “IMAGE Skincare’s clinical excellence, commitment to education and practitioner-first ethos aligns closely with our own values. Together, we’re excited to bring a joined-up approach to distribution, training and professional support, helping practitioners feel confident, empowered and fully supported in delivering outstanding results for their patients.”
Wigmore Medical is exhibiting at ACE on March 13-14. Turn to p.20 to register.
Survey Findings
The Irish College of Aesthetic Medicine (ICAM) has released findings from its National Practitioner Audit survey.
According to the survey, which featured 77 members of ICAM, medical prescribers reported that patient safety has been compromised due to a lack of regulation, with more than 80% of complications managed by ICAM doctors and dentists originating from non-prescribers, including non-healthcare providers.
Additionally, it revealed 68% of practitioners reported a decrease in dermal filler popularity, alongside rising concerns about complications and overuse. Of those questioned, 85.5% support restricting dermal fillers to medically trained professionals and specifically trained “prescribers.”
ICAM’s education officer and aesthetic practitioner, Dr Cormac Lynch, commented, “These figures represent a snapshot of the risk posed to the general public seeking non-surgical aesthetic procedures in Ireland. They underpin the necessity for urgent legislative change and a mandatory training pathway to ensure all practitioners are adequately trained.”
ICAM will be speaking at The Association Zone at ACE on March 14. Turn to p.20 to register.

mesoestetic’s next-generation microneedling device
mesoestetic proudly announces the launch of axion, a breakthrough microneedling device engineered to elevate precision, performance, and patient comfort
axion brings a new standard to clinics seeking reliable, high-impact results supported by scientific excellence.
axion integrates technologies that act synergistically and simultaneously: precise creation of microchannels, automated product dispensing and red LED light with restorative action, maximising efficacy and enhancing results. scan to contact us about axion

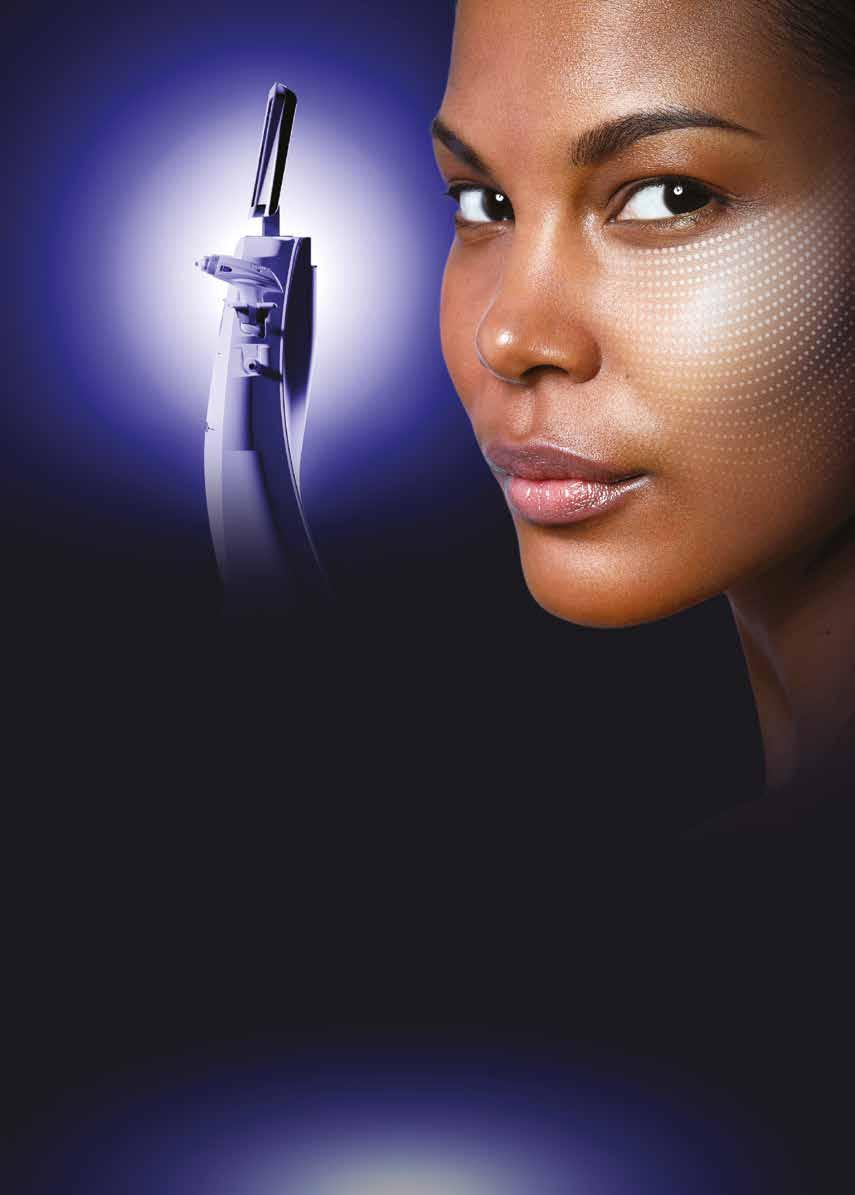
Skincare company DIBI Milano has introduced the DIBI Milano Skin Analyzer system.
According to the company, the system incorporates a dermoscanner equipped with five-megapixel cameras capable of capturing high-definition images at up to 20 times magnification. DIBI Milano states that the device enables detailed skin imaging and three-dimensional skin analysis, with integrated visual comparison across seven skin parameters, including pores, wrinkles and impurities.
Rebecca Loades, brand manager at DIBI Milano, commented, “Innovation has always been at the heart of DIBI Milano, and our new Skin Analyzer is no exception. The precise level of data-driven results undoubtedly empowers practitioners and skin specialists to deliver truly personalised treatment plans and measurable results for every patient.”
Patient and clinic management software provider Clinicminds has launched an AI-powered system for video consultations. According to the company, the AI powered system, Quinn Smart Summary, automatically generates structured clinical documentation during video calls, capturing patient remarks and treatment discussions, without requiring practitioners to manually take notes. Clinicminds shares that the release also introduces picture-in-picture functionality available on iPad, laptop and desktop, allowing practitioners to shrink the video call to a corner of the screen and access patient records, treatment history or clinical notes mid-consultation.
Guy Makmel, CEO of Clinicminds, commented, “Complete documentation is the foundation of continuity of care, yet medicine has long relied on practitioners remembering details after the fact. Quinn Smart Summary closes that gap, capturing every consultation in full so patients and practitioners can pick up exactly where they left off.”
A round up of the latest aesthetic clinics opening across the UK
Aesthetic practitioner Dr Priya Verma has officially opened her new clinic, ART Clinic by Dr Priya Verma, in Belgravia, London. Having relocated from Notting Hill, Dr Verma is well known in the aesthetics community for her expertise

Laser technology company UltraClear, owned by aesthetic device company Acclaro Medical, has introduced Victoria Voysey as vice president of EMEA for UltraClear.
The company reveals that Voysey joins UltraClear following two years as managing director for aesthetic device company InMode. According to UltraClear, Voysey’s role includes working with each territory across Europe, the Middle East and Africa to grow and strengthen market penetration, alongside brand presence.
Voysey commented, “What excites me most about this role is the opportunity to build something meaningful at scale, shaping a truly strategic EMEA presence while working with technology that has the potential to redefine standards in our field. I’m looking forward to combining disciplined execution with bold thinking, building high-performing teams and creating long-term value for both the business and its partners.”
Acclaro Corporation will be exhibiting at ACE on March 13-14. Turn to p.20 to register.
Stem Cell
Medical device and regenerative medicine company Seffiline has launched kits for harvesting and reinjecting adipose-derived stem cells (ADSCs).
Available through aesthetic distributor ES Aesthetic Solutions, Seffiline explains that its range of kits includes all required disposables, along with a patented guide and specialised syringes and cannulas, designed to safely harvest stromal vascular fractions. The company adds that the kits can be used by aesthetic physicians with no prior liposuction experience and are offered in four specialised sets tailored to face rejuvenation, hair restoration, intimate treatments and orthopaedic care.
Edina Bashich, CEO and co-founder of ES Aesthetic Solutions, commented, “This innovative regenerative treatment allows practitioners to harness the body’s natural healing potential, raising the standard of medical aesthetics while providing patients with safe, science-driven and natural results.”
in non-surgical skin rejuvenation. To celebrate the launch, she has added various treatments to the clinic’s menu including LaseMD Ultra, Manual Lymphatic Drainage and the Signature Belgravia Facial.
Aesthetic practitioner Dr Caroline Hall has announced the launch of her new clinic, located in Richmond, North Yorkshire. Clinic services include injectables such as botulinum toxin,
dermal fillers, polynucleotides and skin boosters, as well as Neogen treatments. Dr Hall commented, “Over the last decade I have worked hard to build a safe and reputable clinic with high standards, and I’m absolutely thrilled to open my second clinic just outside the beautiful village of Richmond – which will uphold the same standards and reputation that my first clinic, R&R Aesthetics, is known for.”
If you’re opening a new UK clinic soon, let us know at editorial@aestheticsjournal.com
A new training event for medical aesthetics professionals, the A-List Cadaveric Dissection and Facial Anatomy Masterclass, will take place from June 12 to 14.
Located at the Royal College of Surgeons in Edinburgh, the event is a surgeon-led training experience designed to redefine clinical understanding within medical aesthetics, with a focus on deep anatomical exploration to support safer, more precise practice.
The organisers share that the A-List programme delivers live cadaveric dissection in small guided groups, providing practitioners with the opportunity to study structures at surgical depth and translate those learnings directly into aesthetic application.
The course features aesthetic nurse practitioner Julie Bass Kaplan and plastic surgeon Mr Jory Kaplan, who will cover advanced surgical principles with practical relevance for injectors, aesthetic practitioners and specialist nurses.
Aesthetic nurse prescriber Lisa Waring, founder of the event, commented, “The A-List Cadaveric Masterclass, guided by aesthetic nurse practitioner Julie Bass Kaplan, places scholarship-funded education at the heart of medical aesthetics. This non-profit initiative offers 30 sponsored places, enabling clinicians to study surgical-depth anatomy safely. We champion education, access and patient-first outcomes, reinforcing integrity in our field.”
Skincare

Available through aesthetic distributor AestheticSource, skincare company Senté has unveiled an antioxidant-rich vitamin C serum.
According to the company, Senté Defense C Serum protects at a cellular level, delivering high-potency vitamin C deep into the skin to help fight UV damage, pollution, inflammation and visible signs of ageing.
Clinical research featuring 16 female subjects, found that after 12 weeks of using the vitamin C serum, 88% of participants reported improved skin clarity and a more youthful glow, while 94% said their skin appeared brighter and more radiant.
Lorna Bowes, CEO of AestheticSource, commented, “We are thrilled to introduce Senté Defense C Serum to our portfolio. This innovative formulation offers visible results and powerful antioxidant protection, while remaining gentle enough for sensitive skin. It’s a valuable addition to the Senté range, delivering effective, clinically proven solutions that support skin health and natural radiance.”
AestheticSource will be exhibiting at ACE on March 13-14. Turn to p.20 to register.
Peptide Product

Skincare company Medik8 has introduced its Niacinamide Peptides serum.
Available through aesthetic distributor Healthxchange, the product aims to visibly refine the pores, reduce blemishes and enhance skin cell renewal. Medik8 shares that the serum features 10% niacinamide, crystalide peptide, hyaluronic acid and n-acetyl glucosamine.
In a clinical study conducted over four weeks on 30 participants, the serum produced a 35% reduction in visible blemishes and 26% reduction in visible pore size in four weeks. In a separate four-week clinical trial using 83 participants, 100% showed a healthier skin barrier within one week, and 94% agreed the serum was gentle on the skin.
Simone Shoffman, education and clinical director at Healthxchange, commented, “Medik8’s Niacinamide Peptides launch represents exactly the kind of results-driven innovations we’re proud to bring to our professional partners. We’re delighted to support its rollout across the professional channel and anticipate strong enthusiasm from practitioners looking to elevate their patients routines.”
Healthxchange will be exhibiting at ACE on March 13-14. Turn to p.20 to register.
Medical aesthetics company Laboratoires FILLMED UK has appointed aesthetic practitioner Dr Gráinne Ryan as clinical trainer for the Republic of Ireland.
The company shares that Dr Ryan is the founder and lead practitioner at Dr. Gráinne Ryan Medical Aesthetics clinic in Killarney, County Kerry and brings with her several years of clinical experience in medical aesthetics alongside her background as a dental surgeon.
According to Laboratoires FILLMED UK, Dr Ryans new role will see her educating practitioners in safe, evidence-based injectable techniques, while upholding the highest ethical and safety standards to promote responsible and patient-focused aesthetic practice.
Scott Julian, Laboratoires FILLMED business unit director UK&I, commented, “We are delighted to welcome Dr Ryan as a clinical trainer for FILLMED in the Republic of Ireland. Her expertise, dedication to patient care and passion for education make her an invaluable addition to our training network, and we look forward to the impact she will bring to supporting and inspiring practitioners across the region.”
Laboratories FILLMED will be exhibiting at ACE on March 13-14. Turn to p.20 to register.
Medical device company iSMART Developments has announced a new collaboration with L’Oréal Groupe.
Developed in partnership with L'Oréal, iSMART Developments has created an LED Face Mask and LED Eye Mask featuring both red light at 630 nm and near-infrared light at 830 nm.
Sue D'Arcy, CEO and founder of iSMART Developments, commented, "Working alongside a global leader like L'Oréal allows us to accelerate the impact of clinically engineered light-based solutions on an international stage. This is a significant step forward not only for iSMART, but for the wider evolution of science-led, professional-grade skin technologies."
Training Courses
Training provider Aesthetic Training Hub has been introduced as a new provider of CPD-accredited education tailored to individuals within the aesthetics field.
Founded by nurse practitioner Emily Watson, the organisation shares that it was established in response to concerns around variability in early-stage aesthetic training. Aesthetic Training Hub further states that its programmes are designed to prioritise patient safety, ethical practice and clinically sound foundations.
Alongside the launch, the company has introduced a digital platform which outlines foundation and advanced training pathways in injectables and skin health. Courses include Skincare and Skin Health, Business and Mentoring Programme and Foundation Dermal Filler.
Watson commented, “Meaningful change within medical aesthetics starts at the beginning. By prioritising safe, ethical and structured training from day one, we can positively influence patient outcomes and the future of the specialty.”
Appointment

Aesthetic device company Cutera has appointed Rebecca Gannon as practice development manager for Ireland. In this role, Gannon will lead clinical education and commercial workshops, while providing ongoing support to clinics to optimise both clinical outcomes and business performance, according to Cutera. Gannon brings experience as an advanced skin and laser therapist, with a strong clinical background in delivering treatments including chemical peels, dermaplaning and microneedling, shares Cutera.
Gannon commented, “Having spent a number of years within the aesthetics field, I’ve seen first-hand the impact that the right technology, training and support can have on a clinic’s success. Cutera truly stands out for its innovation, integrity and genuine partnership with its patients, and I’m incredibly proud to now be part of that journey.” Cutera will be exhibiting at ACE on March 13-14. Turn to p.20 to register.
New book debuts called Aesthetic Man
Paul Olavesen-Stabb, CEO of aesthetic manufacturer MÖ Scandinavia Group, has released a book aimed at encouraging men to take care of their mind, body and skin. Olavesen-Stabb commented, “Aesthetic Man incentivises men to consider the way they think and act, especially when it comes to skincare. Brain power, strength, flexibility of joints, memory, libido and skin condition can all deteriorate with age, and a man can take firm and decisive action to hold off these negative changes for as long as possible.”
Cavendish Clinics ceases operations in John Lewis stores
Aesthetic clinic chain Cavendish Clinics has confirmed that all its clinics operating within department store chain John Lewis have ceased trading with immediate effect. In a statement online, the clinic has said it is unable to honour any outstanding appointments or pre-paid treatment packages. The company shares it has directed all enquiries and requests for refunds of pre-paid treatments to payment card providers. Cavendish Clinics further notes that the Fitzrovia Clinic is a separate legal entity and is unaffected by this change.
W-Wellness secures strategic funding Wellness platform W-Wellness has announced the completion of its latest funding round, which includes strategic investment from DMG Ventures. According to the company, engagement with the platform is soaring, with site users up more than 250% in the past six months, while subscriptions have grown over 8,300% year-on-year. Sophie Woodward, co-founder and CEO of W-Wellness, commented, “Our phenomenal growth in 2025 reflects both the scale of unmet need and the trust our community has placed in our expert-led approach.”
Mr Lorenzo Garagnani receives an MBE
Mr Lorenzo Garagnani, consultant orthopaedic hand and wrist surgeon at Guy’s and St Thomas’ NHS Foundation Trust, has been awarded an MBE for his services to children with hand and upper limb differences. Working at the Trust for a decade, he has led specialist surgery, research into less invasive techniques and volunteering initiatives. He also helped establish the UK’s first clinical genetics hand surgery and therapies clinic, improving integrated, patient-centred care across all ages.


























Aesthetics investigates the risks and repercussions of inappropriate weight-loss prescribing
An ITV News investigation has revealed that young people with a healthy body mass index (BMI) are using artificial intelligence (AI) and basic photo-editing tools to obtain prescription weight-loss medication online.1
To explore how easily these systems could be bypassed, an ITV reporter used basic editing software to enlarge their face, waist and body before sending the image to several online pharmacies. Within a week, three separate pharmacies approved the reporter for weight-loss medication, with prescriptions subsequently issued.1 ITV found that this was not an isolated incident, as three additional women were also approved for weight-loss medication, sometimes using only a single edited image.1 Following the investigation, the General Pharmaceutical Council (GPhC) has confirmed that all three pharmacies have been inspected. Two were found to not meet the GPhC’s standards, while one remains under investigation.1
This has caused concern in the aesthetics specialty, with the findings highlighting wider consequences beyond online prescribing, particularly for aesthetic practitioners who are increasingly seeing the effects of rapid weight loss in clinic.
Under General Pharmaceutical Council (GPhC) guidance, before prescribing weight-loss medication, the prescriber must independently verify a person’s weight, height and/or BMI to support safe decision-making.2 The guidance also requires two-way communication between the prescriber and the patient for all online prescribing. However, this consultation does not have to take place face to face; remote consultations are permitted for weight-management medicines, provided the prescriber has sufficient information to prescribe safely.2,3
This approach differs from the prescribing of botulinum toxin and other non-surgical cosmetic medicines, where remote prescribing is not permitted under the GPhC, General Medical Council (GMC) and Nursing and Midwifery Council (NMC) guidance, and a face-to-face consultation is required.4,5,6 Pharmacist and founding director of the Complications in Medical Aesthetic Collaborative (CMAC) Gillian Murray
says that the priority is ensuring that the guidance is being followed, which comes down to enforcement, inspection and clear consequences for pharmacies.
“If something goes wrong, the prescriber must be able to justify that the information they relied upon was sufficient. In the current landscape, particularly with the increasing use of AI, relying on minimal or low-quality information creates clear patient safety and medicolegal risk,” says Murray.
Murray and aesthetic practitioner Dr Victoria Manning, who offers GLP-1 medication in her clinic, both believe it is not appropriate to provide weight-loss injections without clinically seeing the patient face to face. Dr Manning says, “The GPhC’s action against pharmacies approving edited images shows regulators are serious about safeguarding. We should expect similar scrutiny in aesthetics as the Care Quality Commission and GMC focus on patient selection and informed consent.”
Dr Manning and Kimberley Cairns, psychologist aesthetic consultant and Joint Council for Cosmetic Practitioners (JCCP) trustee, warns that many individuals who manipulate online systems to access GLP-1 drugs later reappear in aesthetic clinics.
Cairns says, “These individuals may try to address perceived flaws that are psychological rather than cosmetic.”
Dr Manning emphasises that saying ‘no’ is sometimes the most important clinical decision to make. “It protects patients, practitioners and the integrity of medical aesthetics as legitimate medical practice,” she says.
In light of the findings from the investigation, Dr Manning believes, “We’re dealing with patients who’ve demonstrated they’ll manipulate systems to get what they want, making informed consent complex and outcome satisfaction unlikely.” Dr Manning notes that, beyond standard red flags, fixation on filtered images, ‘perfect’ features and a difficulty recognising positive outcomes can signal serious concern. “After 20-plus years, I trust gut feeling. If something feels off – I won’t proceed,” says Dr Manning. Cairns explains that for these patients, clear referral pathways are essential for pausing, deferring or declining treatment. She adds
that access to a multidisciplinary team (MDT) support, including prescribers, psychological practitioners, GPs, dermatologists and specialists in eating disorders, hair, and safeguarding, is essential.
Cairns explains that failing to recognise indicators of BDD or significant body-image vulnerability is not a minor oversight.
“In today’s landscape – shaped by GLP-1-related body change, AI-distorted self-image and increasing regulatory scrutiny – such omissions may constitute a safeguarding failure,” she says.
Dr Manning suggests that for all aesthetic consultations, practitioners should routinely use validated screening tools such as the body dysmorphic disorder questionnaire (BDDQ) and gather a comprehensive history of the patient, covering recent weight loss – including GLP-1 use.7 Murray adds, “These medicines should not be viewed as transactional. Prescribing them properly requires a wider clinical assessment and appropriate follow-up.”
Cairns adds that practitioners have an opportunity to strengthen their attunement to patients’ emotional needs.
“Compassionate listening, gentle curiosity and thoughtful documentation create a safer, more supportive environment,” she says, adding that front-of-house teams often identify early signs of distress or urgency.
Cairns says, “Practitioners should decline treatment when psychological risk outweighs cosmetic benefit. Treating the area of obsession does not improve BDD and may worsen symptoms.” She notes that behavioural presentation matters as much as verbal reports. Signs of distress, impulsivity, agitation or overinvestment in appearance – and any mismatch between what a patient says and how they present – should prompt further exploration.
Murray believes these medicines are here to stay, and in light of the investigation’s findings, regulators including the NMC and the GMC, should strengthen prescribing guidance, with stricter guidance applied to online pharmacies.
Cairns concludes by saying, “Psychological literacy becomes an untapped currency in clinical practice – strengthening safety, improving outcomes, and protecting both patients and practitioners.”



Every year, it becomes harder to decide which education is genuinely worth your time. Between online courses, social media ‘tips’ and brand-led training, it can be difficult to know what will really move the needle in your day-to-day practice – and what will not. Most medical aesthetics practitioners want the same things: to feel confident with the patients sitting in front of them, to work safely, to build a sustainable clinic and to stay current without being pulled in a hundred directions. The real challenge is finding education that is practical, unbiased and aligned with the stage you are at in your career.
The Aesthetics Conference & Exhibition (ACE) is designed with that in mind. On March 13-14 at the Business Design Centre, Aesthetics will host two days of focused learning, live demonstrations and honest discussion shaped around different experience levels – so you can select sessions that match your stage of practice, whether you are just starting out, consolidating your skills, working at an advanced level or running a busy clinic.
At the beginning: build safe, solid foundations
For practitioners new to aesthetics, ACE is an opportunity to get the basics right from the start.
Beginner-friendly talks break down treatment planning step by step, show you how to approach common indications and emphasise consent, communication and setting realistic expectations.
The In Practice Theatre is especially useful at this stage because it focuses on the realities of starting out in aesthetics – from understanding the basics of clinic life to building good habits early on. Sessions such as Building a Successful Aesthetic Career, brought to you by our Starting Strong in Aesthetics partner Cosmetic Courses, are designed specifically for those at the beginning of their journey. You can also learn how to present your work professionally in Before & After Done Right: Creating Images That Grow Your Aesthetic Practice, and gain practical insight into key business issues with talks like Real-Life VAT Lessons: Veronica Donnelly narrates Dr Sophie Shotter’s VAT Case. In Practice companies will also be taking to the stage, allowing you to get advice from the solution and service providers that make advancing your business.
In the Aesthetic Business Blueprint masterclass chaired by Rick O’Neill, topics include clinic profitability, cybercrime, patient funnels and non-salesy selling, helping you understand how successful clinics really operate. For beginners, this mix of clinical context, business fundamentals and risk


awareness makes the In Practice Theatre a valuable place to build confidence in the non-clinical skills that underpin safe, sustainable practice.
The Association Zone is designed to give practitioners direction and reassurance. Here, you can speak directly with professional bodies about registration, recommended standards, guidance on safer practice and how current regulation affects you as a new practitioner. It is a chance to ask the ‘big picture’ questions about doing things properly from day one. Within this Zone is the Association Theatre, featuring speakers from the leading specialty groups, bodies and associations. Each talk will explore key topics and trends from the last 12 months and provide guidance on how these can impact and improve your practice.
Intermediate: refine techniques and expand your toolkit
Once you have mastered the basics and are treating patients regularly, the next challenge is consistency and confidence in more complex cases.
Intermediate practitioners will benefit from sessions that focus on full-face treatment planning, layering modalities and managing more nuanced presentations in the Aesthetics Mastery Theatre. Live demonstrations highlight the details that make a difference – from product
choice and injection depth to movement assessment and patient selection. Companies you can learn from include:
· BeautyEurope
· DermaFocus (Lunchtime Takeover Sponsor)
· Evolus
· Healthxchange
· IBSA
· Merz Aesthetics
· S.Thepharm
At this stage in your career, you may also be exploring new devices or treatment categories. The Innovation Forum is ideal for testing the waters – you can see what is emerging, ask questions and decide whether a technology is right for your patient base before investing. Discover the latest advancements from:
· AestheticSource
· Arthrex
· AesthetiCare
· BTL Aesthetics
· Cure Medical
· Dermapenworld (Innovation Forum Sponsor)
· Fotona UK
· Hydrafacial
· iiaa
· Klira Clinical
· Sciton
· SkinCeuticals
· Sofwave
· SR Biotech (Idenel)
Alongside the theatres, Stand Seminars on the event floor give you practical insights into new products and devices, helping you make informed investment decisions based on clinical performance and commercial potential.
Advanced: challenge your thinking and lead your field
Experienced practitioners already at the top of their game will find plenty of content designed to stretch their thinking. Advanced sessions in the Allergan Aesthetics Auditorium explore approaches to skin health across ages and genders, practical strategies for facial and neck rejuvenation post-weight loss, and advanced treatment planning for specific patient groups. Join leading experts including Mr James Olding, Dr Apul Parikh, aesthetic nurses Alice Henshaw and Julie Scott, Dr Jonquille Chantrey, Mr Taimur Shoaib, Dr Nestor Demosthenous, Dr Sophie Shotter, for in-depth talks on pharmaceutical-induced weight loss, and multiple injectable demonstrations. Advanced practitioners can also explore next-level injectable skills in The Aesthetics
Challenge: Pushing the Limits of Cannula Mastery, taking place in the Aesthetics Mastery Theatre at 14:10 on day 2. Here, you can experience an immersive live demonstration where three experienced injectors, including Mr James Olding and Dr Jordan Faulkner, perform their chosen treatments using hyaluronic acid dermal fillers Juvéderm, Revanesse and Belotero. Chaired by Mr Dalvi Humzah and Dr Beatriz Molina, it will cover areas such as periocular rejuvenation, mid-face shaping and lower-face contouring, the session focuses on anatomical landmarks, safe access points, depth control and strategic product placement, with live critique from a specialist panel.
The new Cutting Edge Theatre is where practitioners can look beyond current practice and into the future: regenerative approaches, novel combination treatments, emerging scientific data and innovative business models. These sessions are ideal if you are already highly skilled and want to stay at the forefront of the specialty. Companies include:
· Croma Pharma
· Cutera
· Galderma
· VIVACY
Clinic owners and managers: focus on strategy and sustainability
ACE is not just for medical practitioners, but also for the people who help keep the business running. Clinic owners, managers and those planning to open their own clinic have a dedicated home in the In Practice Theatre, with associate sponsors Phorest and Zenoti. Here, the emphasis is not just on what happens in the treatment room, but on everything that surrounds it: marketing, team structure, patient journey, pricing, compliance and risk management.
Sessions cover topics such as:
· Spotting Eating Disorders in the Age of Weight-Loss Injectables with Kimberley Cairns
· Aesthetics Business Blueprint: The High-Performance Clinic – Systems, Standards and the Staff Behaviours that Print Money with Rick O’Neill
· The Consultation Blueprint: Turning First Visits into Long-Term Treatment Plans with Alison Colville
· Create, Engage, Book: The Ultimate AI Workflow for Aesthetic Clinics with Richard Gibbons

Event director Shannon Kilgariff gives top tips on making the agenda work for you
Whatever your level, a little planning will help you get more:
• Be honest about where you are now – beginner, intermediate, advanced or clinic owner – and choose most of your sessions in that band.
• Add one “stretch” session slightly above your current level to inspire growth.
• Prioritise sessions that address your current challenges in clinic.
• Aim for a balance of clinical, and business content so you leave with a rounded plan for your next steps.
• Leave short gaps between sessions to jot down key takeaways and decide what you will implement in the first week back. Make sure to visit the stands on the exhibition floor during this time!
• If you are attending with colleagues, divide and conquer: cover different sessions, then share notes afterwards.
• Use the Aesthetics Connect app and smart badge to build your schedule, capture content and follow up with speakers and brands after the event.
Wherever you place yourself on the beginner–advanced spectrum, there is a clear educational path waiting for you – and the next step in your aesthetics journey is only a session away.
View the full educational programme online and start planning your journey!

Patients want real results that look natural, not overdone. Matrix™ by Candela delivers skin renewal that evolves with every age, concern, and tone, helping you build loyalty and grow revenue in one seamless system. Treat, tighten*, and transformwithout compromise.**






Special Feature
Upper Arm Laxity
Three practitioners discuss the pathophysiology of skin laxity and evaluate treatment modalities aimed at optimising both aesthetic appearance and functional outcomes
Weight loss can result from a variety of interventions. For example, lifestyle modifications including diet and exercise promote gradual, sustained fat loss.1 Bariatric surgery on the other hand results in rapid, significant weight reduction via restriction or malabsorption mechanisms.2 More recently, glucagon-like peptide-1 (GLP-1) receptor agonists have emerged as effective pharmacologic treatments. They work by binding to GLP receptors to trigger the effects of the GLP-1 hormones, with participants in clinical trials losing 15-20% of their baseline body weight.3,4
While these approaches are transformative in reducing adiposity, the rapidity and extent of weight loss can contribute to skin laxity due to diminished dermal support.5
The use of GLP-1 therapies and bariatric interventions means practitioners are now seeing more patients with significant weight loss and unanticipated skin laxity – particularly of the upper arms – presenting in routine aesthetic practice.4
In this feature, oral and maxillofacial surgeon Ms Yuliya Diedyk-Gusarova, aesthetic practitioner Dr Aggie Zatonska and consultant plastic surgeon Mr Adrian Richards examine the therapeutic options for managing upper arm laxity in patients post-significant weight loss.
Skin laxity following excessive weight loss is primarily due to deterioration of the skin’s elasticity, which compromises its structural support and leads to an overwhelmed excess skin envelope.6 Chronic stretching of the skin causes depletion of collagen and degradation of elastin fibres, resulting in dermal thinning and reduced recoil capacity.7
The degree to which this manifests varies between individuals depending on factors such as age, genetics, the duration of obesity and the rapidity of weight loss.8 Clinically, this condition often presents as redundant skin folds, commonly seen in the arms, and can have significant aesthetic and functional consequences – including intertrigo, discomfort during physical activity and psychological distress.9,10
Dr Zatonska describes the upper arm as a distinctive anatomical region that demonstrates ageing differently from other body areas due to its unique structural characteristics.11 “It ages differently from other anatomical regions because of thinner skin and reduced structural support,” explains Dr Zatonska, adding that the dermal layers here are thinner, with relatively little subcutaneous fat, which causes laxity and crepiness to become visible earlier.12 “There is limited subcutaneous fat, which makes changes more visible and distressing for patients, especially when the area is exposed,” she notes.12
Dr Zatonska explains, “The mechanism of weight loss does not alter the final clinical presentation, but it impacts how quickly the ageing becomes apparent.”13 She continues on to say that GLP-1 receptor agonist–induced weight loss is noted to cause a more abrupt fat loss, often without accompanying exercise.13 “This results in skin unable to accommodate the sudden volume reduction,” she adds.13
In addition to fat loss, muscle atrophy can also occur unnoticed. “Loss of both adipose tissue and muscle removes critical structural support, accelerating skin laxity in the upper arm,” notes Dr Zatonska.14 Ms Diedyk-Gusarova emphasises that understanding this balance between skin laxity, remaining fat and muscle tone is critical for proper assessment.
Ms Diedyk-Gusarova highlights that patients with significant upper arm laxity following weight loss are not a homogeneous group. “Careful patient selection, realistic goal setting and a clear understanding of anatomical limitations are essential when considering aesthetic treatment for post-weight loss upper arm laxity,” she says. Common contraindications for most aesthetic treatments in this area may include pregnancy, breastfeeding, uncontrolled hormonal imbalance and known allergies.15,16
Assessment and consultation
Mr Richards highlights that the timing or cause of weight loss both affect the assessment of upper arm laxity. He explains that rapid weight loss can cause thinning and loosening of subcutaneous tissue and skin, often leading to excess skin. “We generally prefer our patients to wait at least three to six months following weight loss to enable us to fully assess the skin area. Generally, a slower weight loss regime is better for reducing ultimate skin excess,” he notes.
Ms Diedyk-Gusarova explains that age and lifestyle are also key considerations. “Patients between 20-50 respond more favourably to non-surgical treatments, particularly before significant hormonal changes,” Ms Diedyk-Gusarova adds.14,17
Diet, sleep quality and physical activity are integral to treatment success. Ms Diedyk-Gusarova notes, “Healthy tissue requires adequate nutritional and metabolic support.”18,19
Dr Zatonska explains that comprehensive medical history taking is essential in her consultations, particularly with the increasing prevalence of GLP-1 use. “Once GLP-1 therapy is identified, I discuss the dose, duration and inform patients about its effects on skin ageing and muscle mass,” she notes. Her physical assessment includes visual examination, palpation and evaluation of muscle function by asking patients to contract their upper arm muscles. “Assessing muscle contraction helps determine muscle strength and its support of the overlying skin. Where muscle function is intact, treatment may focus primarily on skin quality; where weakness or atrophy is evident, muscle stimulation becomes an adjunct,” adds Dr Zatonska.
Ms Diedyk-Gusarova notes, “A subset of patients present with mild-to-moderate laxity characterised by reduced dermal quality and compromised tissue support rather than true excess skin.” In these cases, she notes that non-surgical treatments aimed at improving tissue quality, extracellular matrix integrity and dermal firmness may offer visible improvement and may delay or complement surgical intervention. Regarding skin quality evaluation, Mr Richards states, “Before any surgical intervention we will assess the skin quality by using the pinch test. If necessary, this might include the use of ultrasound to delineate the fat pads in the area. We have a catalogue of before-and-after images of patients with similar procedures and different skin qualities, which helps us advise patients on likely outcomes.”
Dr Zatonska notes, “Crepiness and textural degradation are the primary patient concerns.” Plastic surgeons use the Teimourian classification system to grade upper arm laxity from one to four for surgical decision-making. 20 While useful, Dr Zatonska emphasises that in non-surgical aesthetic practice, treatment is generally directed toward patients with Grade 1 to 2 laxity – representing minimal to moderate skin laxity. “The grading system aids surgical planning but has limited relevance in non-surgical settings, where we treat mostly mild to moderate laxity,” she explains.
Hormonal factors
Hormonal status is also an important consideration. Dr Zatonska highlights that perimenopausal and menopausal changes reduce collagen and elastin synthesis, accelerating skin ageing. “Patients often address facial ageing first, then notice upper arm laxity that feels disproportionate to their facial treatments,” she says. 21
Ms Diedyk-Gusarova adds that hormonal imbalance can also affect treatment outcomes and is considered a relative contraindication until stabilised.
“Hormones significantly influence fibroblast activity and dermal regeneration, so they must be factored into both treatment planning and expectation management,” she notes. 22
Both practitioners emphasise transparency. “Non-surgical treatments improve hydration, texture and crepiness, but they do not replicate surgical lifting,” Dr Zatonska stresses. 23 Open discussion of achievable outcomes and referral pathways is essential to patient satisfaction.

Before After



When to refer for surgical interventions
Following a thorough assessment, patients can be stratified into those appropriate for individual non-surgical intervention, those who may require a combination of modalities, and those for whom surgical brachioplasty is indicated.
For patients with relatively minor skin excess, Mr Richards notes that a surgical consultation would be appropriate to discuss treatment options. He adds that this could include skin tightening treatments such as Renuvion combined with liposuction. “This has the advantage of having minimal scars,” he adds.
Mr Richards says, “These techniques can be effective where there is sufficient residual elasticity and limited redundancy.”15 However, if skin excess is more pronounced and can’t be tightened with skin-tightening procedures, Mr Richards notes, “Excisional surgery is required to remove the redundant tissue, with an associated scar along the inner aspect of the arm.”
He emphasises that referral does not equate to immediate surgery. “A consultation – including virtual consultations – allows patients to discuss concerns, review clinical photographs and understand the full range of options available to them,” he adds. This process mirrors standard surgical pathways across other body contouring procedures.
Dr Zatonska explains that treatment strategies are individualised and frequently combination-based, addressing multiple aspects of tissue ageing, volume loss and dermal weakness. She notes that modality selection depends on skin quality, degree of laxity, downtime tolerance and lifestyle factors, saying, “We often combine treatments to optimise outcomes rather than relying on a single device or injectable.”25
Ms Diedyk-Gusarova advocates a biological, staged approach rather than aggressive mechanical intervention. “The challenge is not just laxity, but reduced fibroblast activity and dermal matrix quality. My goal is to reactivate fibroblasts and stimulate healthy collagen, elastin and hyaluronic acid (HA) production for gradual, stable improvement,” she says.26
In Dr Zatonska’s practice, ultrasound-based technology forms the foundation of treatment, explaining, “Ultrasound energy safely stimulates collagen and elastin with minimal downtime, making it well suited for upper arm skin tightening. In my clinic we use Sofwave.”27 She adds, “Sofwave offers the benefit of no social downtime but may have limited efficacy in patients with significant laxity,” noting that “Clinical improvement typically becomes apparent only after several months.”28 For patients with muscle depletion, Dr Zatonska incorporates EMSCULPT NEO as an adjunct This device combines high-intensity focused electromagnetic (HIFEM) energy with radiofrequency to induce muscle contractions, effectively improving muscle tone and body contour.29 “Muscle stimulation supports functional strength recovery, particularly following rapid weight loss, but it complements – not replaces – exercise, she notes. She adds that muscle stimulation protocols generally begin with six treatments spaced between 10-14 days apart.29
For patients preferring non-energy-based treatments, she offers LPG endermologie, a mechanical massage technique known to enhance circulation, stimulate fibroblast activity, and improve skin texture and firmness over time.30 “It promotes lymphatic drainage, circulation and mild tightening, though it requires commitment to multiple sessions, at a minimum of 10 sessions, starting at one to two a week,” she adds. When to comes to mechanical stimulation therapies, Dr Zatonska explains that LPG requires a high number of treatment sessions, representing a considerable time commitment, with improvements that are often subtle.31
In cases with significant photodamage or permanent lines, ablative CO2 laser resurfacing may be considered where downtime is acceptable. “Laser resurfacing is reserved for advanced textural and pigmentary changes and is not indicated for mild crepiness alone,” Dr Zatonska adds. In her practice, this approach is performed using the SmartXide CO2 system. Recovery typically involves approximately two weeks of healing.32
Ms Diedyk-Gusarova cautions against excessive thermal injury in compromised tissue. “We can stimulate fibroblasts biologically rather than through aggressive burning. Understanding tissue biology allows us to achieve regeneration without unnecessary trauma,” she says. Dr Zatonska notes, “Ablative CO2 laser resurfacing is associated with greater downtime and procedural discomfort and carries a higher risk of post-inflammatory hyperpigmentation, particularly in darker skin types.”33
Biostimulatory HA injectables can play a supportive role in improving dermal quality and hydration. In her practice, she uses Profhilo Body for this purpose. Dr Zatonska frequently combines this approach with ultrasound treatments (Figure 3&4). “Profhilo offers early improvements in hydration and texture, while ultrasound drives longer-term collagen remodelling. The synergy delivers both immediate and progressive benefits,” she explains.34 Dr Zatonska cautions that, “Profhilo can be associated with bruising, treats a relatively small surface area per syringe, and requires ongoing maintenance every four to six months to maintain results.”34 “In my practice, the initial course of Profhilo Body consists of two treatments spaced one month apart,” says Dr Zatonska.
Ms Diedyk-Gusarova employs a sequential regenerative protocol, beginning with enzymatic skin optimisation before introducing biostimulatory agents (Figure 1&2). She typically starts with enzymatic treatments, designed to break down dysfunctional collagen fibres, preparing tissue for subsequent interventions. In her practice, this includes PB Serum HA High, which contains enzymes such as collagenase to prepare the skin for subsequent interventions. After reassessment, she may incorporate amino acid replacement therapies such as Jalupro HMW, which contains a rich profile of amino acids and high molecular weight non-crosslinked HA. Building on this approach, Ms Diedyk-Gusarova adds that amino acid replacement therapy usually requires one to three sessions spaced two weeks apart. Ms Diedyk-Gusarova highlights that while non-surgical treatments offer valuable regenerative benefits, they have inherent limitations. She explains, “Enzymatic therapies are primarily preparatory; they improve tissue quality but do not address significant skin excess or volume.”33 Ms Diedyk-Gusarova adds, “Platelet-rich plasma (PRP)-based regenerative treatments are an option.” She notes that PRP may be combined in alternating sessions with HA to further stimulate dermal regeneration. One example she uses is ReganLAB Cellular Matrix, which combines 2ml of non-crosslinked high molecular weight HA with PRP. She explains that this treatment is used to support cellular activity and extracellular matrix restoration. When discussing limitations, she describes it as a “Regenerative adjunct whose outcomes vary with patient biology and cannot replace surgery in advanced laxity cases.”36 Once tissue is optimally primed – generally after two to three months of treatment – she introduces biostimulators such as calcium hydroxylapatite (CaHA) or poly-D,L-lactic acid (PDLLA)-based products, such as Lenisa, to induce controlled collagen neosynthesis rather than immediate mechanical tightening. “On well-prepared tissue, the risk of complications is minimal and results are more predictable, often requiring a single session for lasting effect,” she says.37 Ms Diedyk-Gusarova explains that follow-up treatments every six months maintain the improved dermal matrix and hydration of the skin.
Biostimulators – including PDLLA and CaHA – work by stimulating collagen production overtime. She cautions, however, that these treatments do not replace surgical excision when there is true skin redundance.37


3&4: A 43-year-old female patient shown at baseline and 16 weeks after a combined biostimulatory treatment protocol. This comprised one session of PB Serum HA High, three sessions of Jalupro HMW at two-week intervals, followed by the RegenLAB Cellular Matrix system one week later, and completed with a single Lenisna session. Images courtesy of Ms Yuliya Diedyk-Gusarova.
Dr Zatonska and Ms Diedyk-Gusarova agree that non-surgical treatments for upper arm laxity have favourable safety profiles when patients are carefully selected and protocols adhered to. Common side effects depend on the treatment but often include transient bruising, swelling, mild sensitivity or temporary discomfort, particularly following enzyme treatments, which can cause localised swelling lasting up to two days.37
Ms Diedyk-Gusarova emphasises that ongoing weight loss requires regular maintenance treatments to prevent worsening, rather than to improve results further. “It’s about controlling the impact of weight fluctuations on skin and volume changes, maintaining tissue quality and functional support,” she notes.
Dr Zatonska recommends Sofwave ultrasound treatments be maintained annually to sustain collagen remodelling. However, for patients undergoing significant weight loss, she advises more frequent touch-ups – potentially every six months – until the patient reaches their goal weight. “It’s not simply about maintaining initial results but managing ongoing tissue changes, fat depletion, and the natural effects of ageing, especially in peri- and postmenopausal women,” she explains.
For mechanical stimulation therapies, Dr Zatonska notes, “Maintenance sessions typically occur every four to six months. For patients continuing to lose weight or unable to maintain exercise routines, additional sessions may be scheduled intermittently to preserve muscle tone and functional support.”
Dr Zatonska recommends that maintenance treatments for Profhilo are carried out every four to six months to sustain and prolong improvements in skin quality.
Adhering to patient goals
Practitioners emphasise that while non-surgical treatments for upper arm laxity offer meaningful improvements in skin quality and contour, their efficacy is limited by the extent of tissue redundancy and individual patient factors. “Ongoing maintenance is essential to preserve results, particularly in patients experiencing continued weight fluctuations,” says Ms Diedyk-Gusarova. Patients with significant or progressive skin excess, or those with functional impairment, should be promptly referred for surgical evaluation to ensure optimal outcomes. Dr Zatonska emphasises that clear communication regarding realistic expectations and treatment limitations is fundamental to patient satisfaction and long-term success.

THE FIRST PROVEN REGENERATIVE BIOSTIMULATOR, WITH RESULTS YOU CAN SEE AND FEEL.

Dr Ed Robinson discusses opportunities, limitations and the emerging role of ultrasound guidance in regional nerve blocks
Demand for injectable and energy-based facial aesthetics continues to rise, alongside patient expectations for comfort, efficiency and safety. Effective analgesia is therefore central to contemporary aesthetic practice. While topical anaesthesia and simple local infiltration remain commonplace, regional nerve blocks offer a more sophisticated approach that can improve patient experience, reduce treatment interruptions and preserve tissue planes for precise work, particularly in multi-layer regenerative and ‘stacked’ treatment plans. In anaesthesia, peripheral nerve blocks are well-established as a cornerstone of multimodal analgesia, reducing opioid requirements and improving patient satisfaction compared with systemic opioids alone.1 A landmark meta-analysis of continuous peripheral nerve blocks (CPNB) demonstrated superior analgesia and fewer opioid-related side-effects versus opioid-based regimens across multiple surgical populations.1 More recently, high-quality trials and meta-analysis have shown that scalp and facial nerve blocks significantly reduce pain scores, opioid use and emergence agitation after surgical cranial and nasal procedures, without an excess of serious complications.2-7
In parallel, there has been growing interest in adapting these techniques to the aesthetic setting, from perioral rejuvenation and lip augmentation to high-intensity focused ultrasound (HIFU) and fractional laser resurfacing.2,8,9
It is, however, important to note that head and neck nerve blocks are specialist procedures with a steep learning curve and potentially serious complications. Practitioners must undertake supervised, in-person education (ideally with cadaveric and ultrasound components), work within local governance frameworks and confirm that their medical indemnity explicitly covers these techniques.
A peripheral nerve block involves depositing local anaesthetic (LA) close to a named nerve or plexus to temporarily interrupt sensory and/or motor conduction in its distribution. Unlike field infiltration, which is placed into the tissues of the target area, a nerve block targets the nerve proximal to its terminal branches, anaesthetising a larger region with a relatively small volume of LA.2,8
In perioperative medicine, single-shot and continuous nerve blocks are used for:
· Pre-emptive and postoperative analgesia (e.g. orthopaedic, breast, abdominal and cranial surgery).
· Opioid sparing, with multiple reviews showing reduced opioid consumption and related adverse effects.1,10,11
· Improved haemodynamic stability, particularly in surgeries where noxious stimuli are highly localised, such as craniotomy pinning and scalp incision.3,12,13 For cranial surgery, three separate high-level evidence syntheses (systematic reviews and meta-analysis) now support the use of scalp blocks to reduce postoperative pain scores for up to 48-72 hours, prolong time to first rescue analgesia and decrease opioid requirements, without a corresponding increase in neurological or systemic complications.2-4
In the aesthetics context, the same physiological principles apply: by blocking key sensory branches of the trigeminal and cervical plexus, we can provide dense analgesia over broad aesthetic units (forehead, temple, mid-face, perioral region, scalp), while avoiding the tissue distortion and unpredictable spread associated with repeated intradermal infiltration.
Benefits of head and neck nerve blocks in non-surgical aesthetics
Head and neck nerve blocks have several benefits in non-surgical aesthetics, for both the patient and the practitioner.
Superior pain control
Randomised trials and meta-analyses in cranial and nasal surgery consistently demonstrate lower pain scores, reduced rescue analgesia and better early recovery with scalp and facial blocks compared with systemic analgesia or local infiltration alone.2-7,13,14 Extrapolating this evidence to aesthetics to include injectables and energy-based devices, where the same sensory territories are targeted but with a less invasive approach, it is reasonable to expect at least equivalent, and often superior, patient comfort.
Combined sessions
For a craniotomy, a scalp block can provide clinically meaningful analgesia for four to 12 hours depending on the agent and concentration used.3,4,15 In aesthetics, this translates into the ability to combine multiple procedures (e.g. full-face biostimulator injections, radiofrequency (RF) microneedling and broadband light or laser modalities) within one visit, without the patient “fatiguing” from escalating discomfort. It is important to note that combination treatments should nevertheless be selected sensibly with the potential side effects of the treatments and clinical judgement should be used.
Higher satisfaction and retention
Facial nerve blocks have been associated with high patient satisfaction in surgical literature, with success rates of 70-90% in achieving adequate anaesthesia and good patient-reported experience.2,8,16 Given the strong link between procedural comfort, perceived professionalism and word-of-mouth referrals, reliable analgesia can support both clinical outcomes and practice growth.
Avoiding issues with topical anaesthetic creams
Topical anaesthetics are effective for many superficial laser, medical and
cosmetic dermatological procedures and injectables, including botulinum toxin injections and dermal fillers, but they are not without drawbacks:17-23
· Contact dermatitis and irritant reactions are well documented, particularly with eutectic lidocaine/prilocaine preparations on compromised skin prior to aesthetic treatments.23-29
· Creams can alter skin impedance and laser-tissue interaction, particularly for ablative CO2 and other water-targeting lasers, leading to less predictable energy delivery.30
· Occlusive, thickly applied creams may act as a barrier, prompting some laser protocols to limit or avoid them, especially in fractionated or low-fluence regimes.30,31 By relying on regional blocks instead of heavy topical anaesthetic, clinicians can avoid these issues and maintain more consistent optical coupling between the laser handpiece and bare epidermis.29,32,33
Benefits to the practitioner
Preservation of tissue planes and surface landmarks
Landmark-guided and ultrasound-guided nerve block techniques typically require smaller total volumes of LA, away from the target treatment site, than extensive field infiltration. This minimises oedema and distortion in the tissue being treated, for example, the vermilion border, nasolabial fold and tear trough, where millimetres matter.8,23 This makes structures easier to delineate and reduces procedural difficulty compared to local infiltration. The advantage of infraorbital blocks in avoiding distortion of the mid-face soft tissues compared with local infiltration has been specifically highlighted.8 Improved precision and workflow
When patients are comfortable, injectors can work more deliberately and systematically rather than chasing the patient’s pain responses with ad hoc infiltration. Surgical data show that facial nerve blocks reduce intraoperative opioid requirements, facilitate haemodynamic stability and shorten PACU stay in septorhinoplasty and rhinoseptoplasty.6,7,34 In aesthetics, this often translates to fewer pauses, less “back-and-forth,” and the ability to maintain a clear mental map of product placement across the face.
Reduced interruptions due to discomfort
Better baseline analgesia reduces the need to stop RF microneedling, HIFU, subcision or multi-pass laser to allow patients to catch their breath.35,36 In my own practice, this has been particularly impactful for stacked protocols combining platelet-rich plasma (PRP), PNs and fractional non-ablative lasers in a single sitting.
Relatively few aesthetic clinics currently offer formal regional anaesthesia as part of their standard workflow. Being able to explain and safely deliver scalp and facial blocks, within robust consent and safety frameworks, provides a point of differentiation that resonates strongly with needle-averse or procedure-naïve patients. Recent reviews in facial and periocular aesthetics emphasise that regional blocks are emerging as a core element of advanced clinic-based practice, rather than a niche anaesthetic technique.9 These blocks can be performed with ultrasound-guidance, the use of which is increasing in aesthetics practice, which enhances accuracy and efficacy of these blocks.16
The following sections summarise anatomy, distribution and general principles. They are not intended as procedural instructions for unsupervised performance. Volumes, approaches and needle handling must be learned in person from experienced clinicians and adapted to local guidelines and ultrasound findings.
Scalp block
A scalp block is typically a multi-nerve blockade targeting branches of the ophthalmic (V1), maxillary (V2) and mandibular (V3) divisions of the trigeminal nerve, plus contributions from the cervical plexus.2 The core components for aesthetic work on the upper face and hairline include:2
· Supratrochlear and supraorbital nerves – Terminal branches of the frontal nerve (V1) emerging at or just above the superior orbital rim. They supply the medial (supratrochlear) and central/lateral (supraorbital) forehead and anterior scalp to the vertex.
· Auriculotemporal nerve – A branch of V3 that travels with the superficial temporal vessels anterior to the ear, innervating the temporal scalp, tragus and superior auricle.
Anatomical reviews and ultrasound studies show that the supraorbital notch/foramen varies laterally but is usually aligned with the medial limbus or medial third of the pupil in primary gaze, whereas the supratrochlear nerve exits more medially near the corrugator origin.2,8 The auriculotemporal nerve typically runs just posterior or superior to the superficial temporal artery as it crosses the zygomatic arch.2,8
Distribution: When the block is successful, patients experience numbness over the forehead, anterior and lateral scalp, temple and parts of the upper auricle. There are limited studies to demonstrate the widespread use of these techniques,
however, in my own practice it is ideal for:37
· Hairline and frontal scalp regenerative work (PRP, exosomes, PNs)
· Temple filler and biostimulators
RF microneedling
· Certain focused ultrasound e.g. Ultherapy and HIFU protocols along the upper third
In neurosurgical literature, complete scalp block (including occipital branches) provides robust analgesia for pinning and incision, with meta-analyses demonstrating reduced pain scores and opioid requirements post-craniotomy.3-5,15
Infraorbital nerve block
The infraorbital nerve is a terminal sensory branch of the maxillary division (V2) of the trigeminal nerve. After traversing the infraorbital canal, it exits via the infraorbital foramen approximately 6-10mm below the infraorbital rim, usually aligned with the medial limbus or mid-pupillary line.8,38 It provides sensation to:
Lower eyelid and malar region
· Lateral nose and upper lip
· Ipsilateral maxillary incisors, canines and premolars, and part of the first molar root StatPearls and facial block reviews highlight its utility for mid-face trauma, nasal procedures and perioral surgery, as well as cosmetic interventions involving the tear trough, nasolabial fold and upper lip.8,16
In septorhinoplasty, combined infraorbital and infratrochlear blocks significantly reduce post-operative pain, analgesic use and emergence agitation compared with controls, with haematoma and oedema being the main reported minor complications.6,7 Randomised trials show similar benefits in nasal and cleft-related surgery, including reduced opioid consumption and improved early recovery.13,34
Distribution:
· Tear trough, medial cheek and mid-face filler
· Non-surgical rhinoplasty (combined with external nasal block)
· Upper lip rejuvenation and lip filler (when paired with mental block)
· RF microneedling and fractional laser over the mid-face
Mental nerve block
The mental nerve is a terminal branch of the inferior alveolar nerve (V3), emerging from the mental foramen below or just anterior to the second premolar, typically halfway between the alveolar crest and the inferior border of the mandible.9,10 It divides into branches supplying:
· Skin of the chin
· Lower lip and labial mucosa
· Anterior buccal gingiva from midline to premolars
Mental nerve blocks provide anaesthesia for soft-tissue work on the lower lip and chin, as well as for various dental and laceration repairs.9,10 Systematic reviews comparing mental/incisive nerve blocks with inferior alveolar nerve blocks for endodontic procedures suggest similar anaesthetic efficacy with potentially fewer neurosensory complications.39,40
Distribution:39,40
· Lower lip filler and peri-oral lines
· Chin augmentation, marionette lines and prejowl sulcus
· Subcision, RF microneedling and ultrasound-based therapies in the mental region
Superficial cervical plexus block (cervical plexus block)
The superficial cervical plexus arises from the anterior rami of C2–C4, giving rise to several purely sensory branches:41
· Lesser occipital (posterolateral scalp)
· Great auricular (ear, angle of mandible, parotid region)
· Transverse cervical (anterior neck)
· Supraclavicular (lower neck, upper chest and shoulder)
A superficial cervical plexus block aims to deposit LA in the fascial plane along the posterior border of the sternocleidomastoid muscle, where these branches emerge.41
Distribution:
· Submental lipolysis and tightening
· Lower face and neck RF microneedling or fractional laser
· Thread lifting along the jawline and lateral neck
Because of its proximity to deeper cervical structures and the risk of inadvertent phrenic nerve involvement with deeper injections, ultrasound guidance and adherence to superficial techniques are particularly important.
Zygomaticotemporal nerve block
The zygomaticotemporal nerve is a branch of the zygomatic nerve (from V2). After exiting the orbit via the zygomaticotemporal foramen, it traverses the deep temporal fascia to supply the anterior temporal region and part of the lateral forehead.2,8,16
Blocking this nerve can supplement a traditional supraorbital/ supratrochlear scalp block, particularly for:
· Temporal hollowing correction and temple filler
· Temporal hairline PRP/PN injections
High-density RF or focused ultrasound in the temporal zone
Zygomaticofacial nerve block
The zygomaticofacial nerve, another branch of the zygomatic nerve (V2), emerges through the zygomaticofacial foramen on the lateral cheek, anterior to the zygomatic bone, and supplies sensation over the malar eminence.2,8
In aesthetics, zygomaticofacial block can be useful where:
· Aggressive RF microneedling or fractional laser is planned over the lateral cheek
· Peri-malar biostimulator or filler treatments cause focal tenderness
It is often combined with infraorbital and zygomaticotemporal blocks to create a comprehensive mid-face and temporal field of analgesia.
External nasal nerve block
The external nasal nerve (external nasal branch of the anterior ethmoidal nerve), from V1 exits between the nasal bone and upper lateral cartilage, supplying the dorsum and tip of the nose.2,8,42
When blocked in combination with infraorbital and sometimes infratrochlear branches, this provides dense anaesthesia of:
· Nasal dorsum and tip
· Columella and soft triangle
This is particularly helpful for:
· Non-surgical rhinoplasty
· PRP or PN injections to the dorsum and soft triangle
· Laser or RF resurfacing of the nasal bridge
Other commonly used facial blocks
Several additional blocks are relevant to advanced aesthetic practice and are well-described in surgical and anaesthetic literature:2,8,16
· Supratrochlear and supraorbital blocks as stand-alone techniques – often sufficient for forehead skin boosters and biostimulator work.
· Maxillary (V2) nerve block via infrazygomatic or greater palatine approaches – occasionally used by oral and maxillofacial surgeons for extensive mid-face surgery, but generally beyond the scope of routine clinic-based aesthetics.
· Inferior alveolar nerve block – extensively used in dentistry; however, it carries a small but real risk of persistent neurosensory deficit, and is less commonly required in aesthetic practice given the effectiveness of mental blocks.11,12
Formal training and a clear governance framework are essential before integrating these into an aesthetic service.
The role of ultrasound in facial nerve blocks
Ultrasound has transformed regional anaesthesia over the past two decades. Multiple meta-analyses across body regions have shown that ultrasound guidance increases block success rates, reduces the required LA volume and lowers the risk of vascular puncture compared with landmark or nerve-stimulator techniques.14,46
A recent integrative review focusing on facial and periocular aesthetic procedures concluded that ultrasound-guided facial nerve blocks:9
· Provide more precise anaesthesia
· Reduce intra- and post-operative complications
· Enhance patient comfort and satisfaction
· Help standardise teaching and sonoanatomy-based training
Similarly, a large multicentre cohort study and subsequent commentary reported very low complication rates (0.4%, with a single episode of local anaesthetic systemic toxicity (LAST) and no long-term sequelae) across 2,700+ ultrasound-guided nerve blocks performed in emergency departments. The authors argue that such blocks should be considered a standard component of multimodal analgesia when appropriately resourced.13,47
A 2025 systematic review of ultrasound-guided nerve blocks in emergency care found an odds ratio of approximately 0.17 for complications compared with standard care, reaffirming the safety advantages of real-time imaging.48
While high-quality randomised trials in purely aesthetic populations are still very limited, extrapolation from craniofacial surgery and growing observational data in aesthetic practice support the use of nerve blocks for:
Scalp and hair-related treatments
Peri-oral rejuvenation and lip filler
Under-eye and mid-face treatments
High-energy devices (face)
Subcision and scar work
Combination or ‘stacked’ aesthetic treatments
Evidence and emerging practice in aesthetics
Ultrasound technique
· PRP, PRF, exosomes and PNs20,37 Mesotherapy and microneedling
· High-energy devices along the frontal hairline
· Perioral rhytid reduction, smoker’s lines, marionette lines
· Upper and lower lip augmentation43
· Biostimulators, skin boosters, regenerative treatments such as PNs44
· RF microneedling and fractional laser resurfacing of the lower eyelid and malar region35
· RF microneedling, fractional lasers, HIFU/Ultherapy
· Particularly over bony prominences and thin skin (forehead, temples, peri-orbital skin, upper lip, jawline)
· Subcision of tethered acne scars, rolling scars or post-surgical scars45
· Complex sessions combining toxin, 35 dermal fillers, biostimulators, microneedling, PRP/PNs and energy-based modalities across multiple facial zones
· Reviews on facial and periocular aesthetics increasingly highlight these indications, especially in the context of ultrasound guided approaches9,16
While detailed protocols are beyond the scope of this article, key principles for ultrasound-guided facial blocks include:8,9,14,16
· Landmark-first, ultrasound-confirmed: Identify the approximate location of the foramen or nerve trajectory using surface anatomy. Then confirm with a high-frequency linear probe, optimising depth and focus to visualise the bony contour, foramen and adjacent vessels.
· In-plane needle approach: Use the non-dominant hand to hold the probe stable. Advance the needle in the longitudinal axis of the probe so that shaft and tip are continuously visible, avoiding vessels and maintaining a safe distance from the nerve itself.
· Perineural, not intraneural, injection: The goal is to deposit a small volume of LA around the nerve or foramen, watching for circumferential spread without nerve swelling. High-pressure injection or nerve expansion should trigger immediate cessation.
· Dose titration and spread assessment: Start with the minimum effective volume, adding only if necessary as spread is confirmed; this is especially important when multiple facial blocks are planned in a single session.
In aesthetics, ultrasound also provides the additional advantage of real-time visualisation of filler deposits, vascular structures and previous threads or implants, potentially enhancing overall procedural safety when combined with regional blocks.49
Contraindications to head and neck nerve blocks
Contraindications can be divided into absolute and relative, recognising that risk-benefit assessments must be individualised.
Typically a tailored scalp block: supraorbital, supratrochlear, auriculotemporal ± occipital branches.
Combined infraorbital + mental nerve blocks can provide near-complete circumoral anaesthesia while preserving lip architecture.
Infraorbital block ± zygomaticofacial and zygomaticotemporal nerve blocks.
Nerve blocks over the main sensory branches in the treatment field allow higher treatment densities and more consistent coverage without compromising tolerability.
Regional blocks tailored to scar location, e.g. infraorbital for mid-face, mental for chin, to enable more aggressive and thorough release.
Blocking the main sensory branches (regional facial nerve blocks) improves tolerability, supports treatment efficiency and may reduce the number of separate visits.
High-quality randomised trials in purely aesthetic populations remain limited, but extrapolation from craniofacial surgery and growing observational data support the expanding use of nerve blocks in aesthetic facial and periocular practice.
Absolute contraindications
Absolute contraindications include:50
· Documented allergy or severe hypersensitivity to local anaesthetic agents
· Patient refusal or inability to provide informed consent.
· Active infection at or near the planned injection site. Lack of appropriate training, equipment or monitoring.
Relative contraindications
Relative contraindications include:37
Coagulopathy or patients on anticoagulants/antiplatelet therapy. While superficial facial blocks generally have low bleeding risk, guidelines for regional anaesthesia and neuraxial procedures should inform individual decisions.
· Pre-existing neuropathy in the distribution of the target nerve. There is theoretical concern about exacerbating deficits or complicating post-procedural assessment.
· Severe anatomical distortion (prior surgery, radiation, scars) that obscures landmark recognition or ultrasound visualisation.
· Systemic comorbidities increasing risk from LA systemic toxicity (cardiac arrhythmia, hepatic failure).
Systematic reviews of mandibular nerve block complications underscore that, although serious nerve injury is rare, persistent paraesthesia and dysaesthesia can occur and often have a medico-legal impact.11,12 Such considerations must be incorporated into aesthetic consent and risk counselling.
Local and regional complications include:11,12
Pain, bruising or haematoma at the injection site
· Oedema and transient tissue distortion
· Inadvertent intravascular injection (with risk of LA systemic toxicity)
· Inadvertent intraneural injection or nerve trauma: transient or persistent paraesthesia, dysaesthesia or, rarely, motor deficit
· Infection, including cellulitis or abscess formation
· Temporary weakness of nearby motor branches (e.g. marginal mandibular branch with cervical plexus or mental block approaches)
Systematic reviews and large observational series in both dental and regional anaesthesia settings suggest that clinically significant nerve injury following peripheral nerve blocks is rare, but possible, and likely multifactorial (direct trauma, intrafascicular injection, neurotoxicity).11,12
Systemic complications include:
· LAST: central nervous system symptoms (tinnitus, metallic taste, agitation, seizures) progressing in severe cases to cardiac arrhythmias and cardiovascular collapse.51
· Allergic-type reactions, though true amide LA allergy remains very uncommon.
Large contemporary series of ultrasound-guided nerve blocks performed in the emergency department report overall complication rates of 0.4-5%, with very low rates of serious events and no long-term harm in most cohorts.13,48
Aftercare advice
After any head or neck block, patients should be advised to avoid hot drinks, chewing or biting hard foods until lip and chin sensation has fully returned (to prevent accidental biting, burns or trauma). They should also refrain from manipulating treated areas excessively while numb, and expect temporary numbness or altered sensation lasting as long as the LA duration. Patients should be advised to report immediately any persistent numbness, pain, swelling or signs of infection.52
When combined with energy-based or injectable treatments, standard post-procedure instructions (sun avoidance, skincare modification, infection precautions) should be reinforced once the block has regressed and the patient can adequately perceive warning symptoms.
Risk mitigation strategies
Key strategies supported by regional anaesthesia literature include:6,13,14,52
· Using ultrasound guidance wherever feasible to visualise nerves, vessels and spread of LA
· Employing incremental injection with frequent aspiration, avoiding high opening pressures or patient reports of paraesthesia during injection
· Keeping within safe maximum dose limits for the chosen LA, adjusting for patient weight and comorbidities
· Working within the limits of one’s competence
An efficient process
Head and neck nerve blocks, adapted from anaesthetic and craniofacial surgery practice, offer compelling benefits for modern medical aesthetics. There is a growing evidence base including multiple recent systematic reviews and meta-analyses which supports their ability to provide superior analgesia, reduce systemic analgesic requirements and improve patient comfort across scalp, nasal and facial procedures.2-7,9,13,16
Ultimately, head and neck nerve blocks should be regarded as specialist procedures. They belong in the hands of clinicians who have completed robust, in-person training in anatomy, ideally sonoanatomy and complications management, and whose indemnity explicitly covers their use in aesthetics. When implemented within that framework, they can underpin a more comfortable, precise and efficient approach to non-surgical facial rejuvenation.
Complete the multiple-choice questions and email memberships@aestheticsjournal.com to receive your CPD certificate!
1. Which of the following is the primary advantage of regional facial nerve blocks over extensive local infiltration in aesthetic practice?
2. The infraorbital nerve block most reliably anaesthetises which of the following regions?
a. Lower risk of local anaesthetic systemic toxicity
b. Greater duration of anaesthesia in all cases
c. Reduced tissue distortion while anaesthetising a larger area
d. Elimination of the need for informed consent
a. Entire nasal dorsum and tip
b. Lower eyelid, upper lip and ipsilateral maxillary premolars
c. Lower lip, chin skin and mandibular incisors
d. Posterior scalp and upper cervical region
a. Patient taking a low-dose direct oral anticoagulant
3. Which of the following is an absolute contraindication to a superficial facial nerve block in clinic?
4. Large contemporary series and meta-analyses suggest that ultrasound guidance for peripheral nerve blocks is associated with which of the following outcomes compared with landmark techniques?
5. Which statement best reflects current evidence regarding topical anaesthetic creams and laser procedures?

b. Previous rhinoplasty with altered anatomy
c. Documented amide local anaesthetic allergy
d. History of migraine with aura
a. Higher risk of vascular puncture but better analgesia
b. Lower success rate but reduced LA volume
c. Higher success rate and reduced risk of vascular puncture
d. No measurable difference in efficacy or safety
a. They have no role in aesthetic laser practice and should be avoided
b. They always increase laser efficacy by hydrating the epidermis
c. They can reduce pain but may cause skin reactions and alter laser–tissue interaction in some settings
d. They completely eliminate the need for eye protection during laser treatment
Answers: C,B,C,C,C
Dr Edward Robinson is an NHS anaesthetics doctor based in Cheshire. He specialises in skin and hair rejuvenation treatments and treating the male face. He is an associate member of BCAM and a key opinion leader for Arthrex and Sciton.
Qual: MBBS, BSc (Hons)
Dr Ahmed El Muntasar presents an overview of strategies for addressing post-weight
Significant weight loss, whether achieved through lifestyle modification, bariatric surgery or pharmacological interventions such as glucagon-like peptide-1 (GLP-1) receptor agonists, is increasingly common in clinical practice 1 While the metabolic, cardiovascular and psychological benefits of weight reduction are well recognised, many patients experience an unintended aesthetic consequence – loose, lax or poorly recoiling skin.¹
For aesthetic practitioners, this represents a growing and complex challenge. Weight loss alone does not reverse the structural and biological changes that occur within the skin and subcutaneous tissues. Collagen degradation, elastin disruption and volume loss may persist long after weight stabilisation, leading to dissatisfaction despite otherwise successful health outcomes.² As awareness of aesthetic treatments increases, clinicians are seeing a rising cohort of post-weight-loss patients seeking non-surgical solutions. To manage these concerns effectively, it is essential to understand why rapid weight loss is occurring, how it affects skin biology and how treatment strategies can be tailored safely and realistically.
The increasing prevalence of rapid weight loss reflects a convergence of medical, lifestyle and societal factors.
Pharmacological interventions, particularly GLP-1 receptor agonists, have significantly altered the landscape of weight management. Originally developed for glycaemic control in type 2 diabetes, these agents are now widely prescribed for obesity due to their effects on appetite suppression, delayed gastric emptying and enhanced satiety. A clinical trial has demonstrated substantial and sustained weight loss over relatively short timeframes, often exceeding that achieved through lifestyle modification alone.³
Bariatric surgery remains another major driver. Procedures such as gastric bypass and sleeve gastrectomy commonly result in dramatic weight loss within the first 12-18 months post-operatively. While these interventions offer clear metabolic and survival benefits, the pace and magnitude of fat loss frequently exceed the skin’s capacity for adaptive remodelling.⁴
Lifestyle-driven weight loss has also evolved. Increased public awareness of obesity-related health risks, alongside structured dietary programmes, intermittent fasting and intensive exercise regimens, has led some patients to pursue aggressive weight-loss strategies. When weight loss occurs rapidly or without adequate nutritional support, dermal repair mechanisms may be compromised.⁵
Societal and aesthetic pressures further contribute. Social media and the normalisation of dramatic before-and-after transformations can promote unrealistic expectations regarding the speed and appearance of weight loss, often without consideration of its physiological impact. Understanding these drivers allows aesthetic practitioners to contextualise post-weight-loss concerns and plan realistic, staged interventions.3-5
Skin laxity following significant weight loss reflects a complex interaction between intrinsic and extrinsic factors.
Intrinsic factors
Intrinsic ageing plays a central role. With increasing age, fibroblast number and activity decline, resulting in reduced synthesis of collagen types I and III and degradation of elastin fibres essential for skin recoil.⁶ Dermal thickness decreases and the extracellular matrix becomes increasingly disorganised, limiting adaptive capacity.⁷
Genetic variation influences baseline skin quality and elastic recovery, while hormonal changes – particularly reduced oestrogen levels – are associated with accelerated collagen loss and impaired wound healing.⁷ These intrinsic factors help explain why older patients often experience more pronounced laxity for equivalent degrees of weight loss.
Extrinsic factors
Extrinsic contributors frequently compound intrinsic ageing. Prolonged mechanical stretching during periods of obesity leads to irreversible collagen and elastin damage. When fat loss occurs rapidly, these fibres may be unable to reorganise effectively.³
The speed of weight loss is particularly important. Rapid fat reduction, commonly seen with GLP-1 therapy or bariatric surgery, may outpace the skin’s biological capacity for remodelling, resulting in deflation and redundancy.³ Ultraviolet exposure accelerates dermal degradation via oxidative stress, while smoking impairs fibroblast function and microvascular perfusion.⁷ Nutritional deficiencies, particularly inadequate protein intake, further compromise collagen synthesis during weight loss.⁵
Clinically, laxity varies by anatomical region. Facial laxity often presents as mid-face deflation, malar fat pad descent, jowl formation, jawline blunting and cervical skin redundancy, contributing to a tired or aged appearance.² Body laxity is typically characterised by redundant, poorly recoiling skin with reduced tensile strength. Abdominal laxity may manifest as pannus formation and horizontal skin folds; upper arm laxity as circumferential excess and triceps deflation; thigh laxity as medial creping and friction-related discomfort; and breast or chest wall laxity as deflation and ptosis.⁴
Importantly, severity does not correlate solely with the amount of weight lost but reflects the cumulative burden of intrinsic ageing, duration of obesity, baseline skin quality and the pace of weight reduction.1-5
Post-weight-loss skin laxity is rarely attributable to a single anatomical change. Evidence increasingly supports layered, multimodal approaches that address multiple tissue depths and biological processes simultaneously.8,9
Energy-based devices (EBDs)
Energy-based technologies, including radiofrequency and ultrasound, stimulate neocollagenesis and tissue contraction through controlled thermal injury. Clinical studies demonstrate improvements in skin firmness and elasticity, particularly in mild to moderate laxity.8,9
Downtime varies by modality and treatment intensity. Non-ablative treatments are typically associated with transient erythema, oedema or tenderness resolving within days. More aggressive protocols may cause short-term swelling or sensory changes, particularly in areas of minimal subcutaneous fat. Importantly, collagen remodelling occurs over weeks to months, requiring appropriate patient counselling.⁸ However, EBDs offer limited benefit in severe redundancy.
Biostimulatory injectables
Biostimulatory agents such as poly-L-lactic acid (PLLA) and calcium hydroxylapatite (CaHA) stimulate endogenous collagen production. PLLA induces gradual fibroblast activation, while CaHA provides both immediate scaffolding and longer-term biostimulation.¹⁰
In post-weight-loss patients, conservative dosing is essential. Reduced soft-tissue support increases the risk of nodularity or contour irregularity if excessive volumes are used. A staged approach with reassessment between sessions supports safer, more natural outcomes.¹⁰ Due to their delayed onset, biostimulatory injectables are not suitable for patients seeking immediate lifting effects.
Skin boosters and regenerative therapies
Skin boosters typically contain non-crosslinked or lightly crosslinked hyaluronic acid, improving hydration, elasticity and dermal turgor without volumisation. Clinical studies demonstrate improvements in skin quality and texture.11,12
Regenerative therapies, including polynucleotides and platelet-based treatments, promote fibroblast activity, angiogenesis and extracellular matrix repair. These treatments optimise the dermal environment, enhancing response to energy-based and biostimulatory modalities when layered appropriately.13,14 However, skin boosters do not correct true skin laxity and require ongoing maintenance.
Active infection, pregnancy, connective tissue disease, implanted electronic devices (specific to energy-based treatments) and unrealistic patient expectations should be carefully considered before proceeding with any of these interventions.15
Integrating lifestyle, medical and procedural approaches
Holistic optimisation should begin at consultation and continue throughout treatment. Adequate protein intake, micronutrient sufficiency, resistance training, smoking cessation and photoprotection all support collagen synthesis and tissue repair.16
An ideal post-treatment care routine focuses on supporting biological recovery rather than immediate visible change: hydration, nutrition, sun protection, activity modification and appropriate treatment spacing. Psychological support may be beneficial for patients adjusting to post-weight-loss body changes.¹
Treating patients using
Aesthetic treatment does not need to be deferred until GLP-1 therapy has ceased. Conservative, staged treatments can be initiated during ongoing weight loss, focusing on skin quality and collagen stimulation. More definitive contouring may be reserved for periods of weight stabilisation.³ Collaboration with prescribing clinicians supports safe, coordinated care.
Safety, patient selection and managing expectations
Knowing when not to treat is central to ethical practice. Severe skin redundancy, functional impairment, untreated nutritional deficiencies, unstable weight or unrealistic expectations are indications to defer or decline non-surgical treatment.⁴
Potential complications include prolonged oedema, bruising and sensory changes following energy-based treatments; nodularity or contour irregularities with biostimulants; and dissatisfaction when expectations are misaligned.8,10,11 Conservative dosing, appropriate spacing and thorough consent mitigate risk.
A patient with 25-30% weight loss over 12 months on GLP-1 therapy and mild–moderate facial laxity might undergo ( Table 1 ). This approach allows biological adaptation and expectation management.4,8,10
Phase 1 Weeks zero to six
Phase 2 Weeks eight to 20
Phase 3 Six months+
Assessment and optimisation
Biostimulation and hydration
Review and escalation
Comprehensive assessment, nutritional optimisation, skincare programme, one to two energy-based treatment sessions
Conservative biostimulatory treatments with adjunctive skin boosters
Reassessment, refinement treatments or surgical referral if required
Table 1: Suggested treatment sequencing strategy for post-weight-loss patients.4,8,10
referral pathways and multidisciplinary
Non-surgical treatments are unlikely to be effective in severe redundancy characterised by hanging pannus, circumferential folds or persistent ptosis. Assessment should include weight history, BMI trajectory, duration of obesity, medical history and functional symptoms such as intertrigo or mobility limitation.⁴ Best practice involves a multidisciplinary approach, particularly after massive weight loss. Collaboration with nutritionists, psychologists and physical therapists supports tissue repair, functional recovery and psychological wellbeing.15 Timely surgical referral should be framed as appropriate escalation rather than treatment failure.
Skin laxity following significant weight loss is an increasingly common presentation in aesthetic practice. Effective management requires understanding the drivers of rapid weight loss, the biological basis of laxity and the limitations of individual modalities.
By integrating lifestyle optimisation, layered non-surgical treatments, multidisciplinary care and appropriate surgical referral, practitioners can deliver safer, more effective and more sustainable outcomes. Personalised assessment and realistic expectation management remain the cornerstones of post-weight-loss aesthetic care.

Dr Ahmed El Muntasar is a UK-trained GP and aesthetic physician with extensive experience in non-surgical facial and body rejuvenation. He has a particular interest in skin quality, regenerative medicine and multimodal approaches for complex aesthetic presentations, and regularly contributes to clinical education and research.
Qual: BSc, MBChB, MSc, MRCGP

*Allergan Aesthetics, an AbbVie company is the headline sponsor for the ACE and has part-sponsored this event. This includes provision of a stand, speaker programme, mentors, and topic input into some mentoring sessions. Allergan Aesthetics has had no influence or involvement over the content or topics covered in other parts of the agenda of the ACE main event.









From lingering redness to stubborn veins, patients are seeking advanced treatments to restore clear, healthy-looking skin. Cutera’s vascular technologies empower you to address a wide spectrum of conditions with precision and confidence.

Vascular concerns can present in many ways:
Diffuse Redness
Rosacea
Telangiectasia
Periorbital veins
Cutera’s platforms are designed to target both superficial and deeper lesions, making them versatile solutions for providers.




Trusted by leading experts across the UK & Ireland


Leg veins
Cherry angiomas
And more.




“excel V+ is the workhorse of our clinic and an essential device for treating vascular concerns. It allows us to safely and effectively target everything from broken capillaries to facial redness, and it is particularly ideal for managing rosacea, delivering consistent and reliable results for our patients”
Dr Nestor & Nurse Amanda, The Mayfield Clinic



Nurse prescriber Claire Amos explores how medical aesthetics can play a vital role in skin cancer surveillance
Skin cancer is among the most commonly diagnosed cancers in the UK. Melanoma mortality has increased by 148% since the early 1970s, although rates have remained broadly stable over the past decade.1 Since the early 1990s, the incidence of non-melanoma skin cancers has risen by 169%, with a further 14% increase projected between 2023 and 2025 (data pending release).2
Although melanoma mortality is projected to decline by approximately 11% between 2024 and 2026 (data pending release), the overall burden of disease remains substantial.1
In England alone, more than 224,000 skin cancer diagnoses – including both melanoma and non-melanoma skin cancers – were recorded in 2019, representing a 26% increase compared with 2013.3
These significant numbers reflect multiple factors, including increased recreational sun exposure, tanning bed use, an ageing population and greater awareness and screening.4 Whatever the drivers, the outcome is clear-skin cancer is both common and rising, creating a growing burden on healthcare.
Within this landscape, medical aesthetic clinics occupy a uniquely advantageous position in recognising suspicious lesions. Unlike many other healthcare encounters, aesthetic consultations involve:
· Close inspection of the skin under magnification and strong lighting.
· Frequent follow-up appointments, giving practitioners a longitudinal view of changes.
· Patient openness about appearance, as they can be more willing to point out pigmentation or lesions in this setting than in a GP consultation.
As professionals committed to patient safety, aesthetics practitioners have both the privilege and responsibility to
notice, document and refer when a lesion looks suspicious.
The majority of UK cases are basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs).1,2 They can cause significant local tissue destruction and morbidity if left untreated.5 SCC carries a metastasis risk of around 3-4%, and even without spread, both types can disfigure and/or impair function when diagnosis is delayed.6
By contrast, melanoma is less common but far more dangerous. It is responsible for more than 80% of all skin cancer deaths, despite making up a minority of diagnoses.1 Five-year survival in melanoma can exceed 95% when detected at an early stage, but falls dramatically once the disease has spread.7 Early recognition and referral are therefore critical.8
There are several risk factors connected to developing skin cancer including ultraviolet exposure, skin type and ethnicity, age and genetic factors.
Ultraviolet exposure
Cumulative ultraviolet (UV) exposure remains the strongest modifiable risk factor for both melanoma and non-melanoma skin cancers.9 Intermittent, intense sun exposure – particularly leading to sunburn – is more strongly associated with melanoma, while chronic, cumulative exposure underlies most BCC and SCC cases.9,10 Indoor tanning is also a significant contributor; the International Agency for Research on Cancer (IARC) classifies tanning devices as Group 1 carcinogens, with first use before age 35 increasing melanoma risk by 75%.11
Skin type and ethnicity
Individuals with fair skin, light hair and light eye colour (Fitzpatrick skin types I-II) are at greatest risk due to lower epidermal melanin protection.12 Although people with darker skin types (Fitzpatrick IV–VI) have a lower incidence, they are often diagnosed later, with more advanced disease and worse outcomes.13 In these patients, lesions are more likely to appear on acral sites such as the palms, soles and nail beds.13
Age and sex
Incidence increases with age, reflecting cumulative UV damage.5,9 Non-melanoma skin cancers are most common in patients over 60, whereas melanoma is more frequent in younger adults compared to most other cancers.14-16 In the UK, melanoma rates are higher in women under 50, but by age 60, incidence is greater in men.17
Genetic and familial factors
A family history of melanoma increases risk two- to three-fold.18 Certain genetic syndromes, such as familial atypical multiple mole melanoma (FAM-MM) syndrome, confer especially high lifetime risk.18 Mutations in tumour suppressor genes such as CDKN2A and p53 have also been implicated in melanoma and SCC, respectively.18,19
Immunosuppression
Patients who are immunosuppressed – including organ transplant recipients, individuals with human immunodeficiency virus (HIV) or those on long-term immunosuppressive therapy – face markedly elevated risks, particularly of SCC.20 A comprehensive review of data from multiple sources reports up to a 65-fold increase in SCC incidence in transplant patients compared with the general population.20
Occupational and environmental exposures
Occupations involving outdoor work (e.g. farming, construction) are associated with higher risks of both melanoma and non-melanoma cancers due to prolonged UV exposure.9,21 Other environmental contributors include arsenic exposure and ionising radiation, though these account for a minority of cases.22
Recognising suspicious lesions
There are several ways aesthetic practitioners can assess suspicious lesions.
Common presentations in aesthetic settings
In aesthetic practice, lesions often come to attention when patients highlight them as appearance concerns, or when practitioners identify them incidentally during treatment
Skin Cancer
consultations. These may range from pigmented macules and keratotic plaques to nodules, ulcers or erythematous patches. While many are benign, a proportion represent skin cancers or precancerous conditions such as actinic keratoses.23
Patients often misattribute lesions to ‘age spots’ or ‘sun damage,’ or are unaware of changes in hard-to-see sites such as the scalp and ears.24 Studies confirm that delayed recognition contributes to later-stage diagnoses and poorer outcomes.7,16
The ABCDE rule for melanoma
For pigmented lesions, the ABCDE criteria remain a cornerstone of early detection:
· A – Asymmetry: one half does not match the other.
· B – Border irregularity: edges are ragged, notched or blurred.
· C – Colour variation: shades of tan, brown, black, red or white within the same lesion.
· D – Diameter: greater than 6mm, though smaller melanomas do occur.
· E – Evolving: any change in size, shape, colour or new symptoms such as bleeding or itching.
These criteria are widely validated as predictors of melanoma risk and remain recommended by international guidelines.25 The “ugly duckling” sign – where one mole looks different from a patient’s other naevi –also helps to highlight suspicious lesions.26
Red flags for non-melanoma skin cancers
There are several red flags aesthetic practitioners should be aware of when assessing patients.
Basal cell carcinoma (BCC)
BCC typically presents as a pearly papule or nodule, often with surface telangiectasia. Lesions may ulcerate, bleed or develop a rolled border, historically described as a ‘rodent ulcer.’27 BCCs arise most commonly on sun-exposed areas such as the face, scalp and neck. While they rarely metastasise, untreated lesions can invade locally and cause considerable tissue destruction.27
Squamous cell carcinoma (SCC)
SCC often presents as a scaly, crusted or keratotic nodule or plaque, which may ulcerate. Lesions can be tender or painful and are often indurated on palpation.6 SCCs may also develop in chronic inflammatory lesions, or in chronic ulcers. SCC carries a higher risk of metastasis than BCC, particularly when large, poorly differentiated
or arising in high-risk anatomical sites such as the lips or ears.6 Early recognition and referral are therefore crucial.
Actinic keratoses (AK)
AK appear as rough, scaly patches that are sometimes easier felt than seen. They occur on chronically sun-damaged areas such as the forehead, scalp and backs of the hands.23 AKs are considered premalignant, with a small but real risk of progression to SCC over time.23 Their presence also signals significant cumulative UV damage and an elevated overall risk of skin cancer.
Anatomical considerations
Aesthetic treatments often involve the face, scalp, décolletage and hands – the very areas where BCC and SCC are most common.6,15 After conducting the ABCDE analysis, practitioners should examine adjacent skin, use magnification and lighting, and document lesions photographically for comparison.28,29 If a suspicious lesion is identified, it should be referred to the GP for onward referral via the two week wait pathway.
Addressing potential skin cancers sensitively is essential. Evidence shows patients value transparency and safety-led care.24 Suspicious lesions should never be treated aesthetically without medical evaluation. The National Institute for Health and Care Excellence (NICE) guidelines recommend urgent two-week referral for suspected melanoma or SCC, and routine referral for BCCs and persistent AKs.8
Tools and technologies
Once practitioners have done the ABCDE ruling and initial assessment of a suspicious lesion, other tools and technologies can be implemented to confirm a suspected diagnosis.
Dermoscopy
Dermoscopy significantly improves detection of malignant lesions compared with the naked eye.29 Dermoscopy can be used routinely to triage patients. For example, BCC may display arborising vessels and translucency under dermoscopy – features that raise suspicion and guide referral. While not diagnostic in itself, dermoscopy provides aesthetic practitioners with an invaluable triage tool to support patient safety. It is important to note that dermoscopy is a specialist clinical skill and it takes hundreds of supervised hours of experience to gain expertise. Aesthetic practitioners should not be using dermoscopy unless adequately trained.
Digital photography
Sequential photography allows detection of subtle lesion changes over time.28,30 In practice, this is particularly valuable for patients with multiple atypical naevi. Photographic comparison across months can reveal changes in size, colour or symmetry that might not be apparent in a single consultation. This approach, whether through standardised clinical photography or digital dermoscopy systems, has been shown to improve early detection of melanoma in high-risk patients.28,30 Aesthetics practitioners should not be providing mole monitoring services without appropriate supervision by a consultant dermatologist. Any suspicious moles should be referred to the GP.
Platforms such as Map My Mole (a digital mole mapping teledermatology service) provide rapid consultant-level review. Practitioners can capture dermoscopic or clinical images in clinic and upload them securely for assessment, often receiving a report within hours. This model shortens the time between suspicion and specialist input, reducing anxiety for patients and enabling prompt escalation where necessary.31
Emerging tools such as reflectance confocal microscopy (RCM) and artificial intelligence (AI)-based lesion classification show promise but are not yet mainstream in aesthetic settings.32,33 RCM offers near-histological resolution for equivocal lesions, while AI systems are being trialled in smartphone applications to flag suspicious moles. At present, these technologies remain primarily in research or specialist dermatology use where the professional is trained in confocal image interpretation, but they highlight the future potential for enhanced lesion detection.
Education is central to prevention. A public survey of 2,163 adults revealed that in 2023, only half of UK adults felt confident recognising skin cancer signs, and fewer consistently use sun protection.34 Training programmes such as Melanoma and Skin Cancer Early Detection (MASCED), delivered by Skcin, significantly improve practitioner confidence.35
When a suspicious lesion is identified, prompt referral is essential. Early escalation ensures appropriate specialist assessment,
A 49-year-old woman attended my clinic for an aesthetic consultation for general skin ageing concerns. During skin assessment, I identified a pigmented lesion with asymmetry, irregular borders and recent colour change. Using dermoscopy and photography, I uploaded images to Map My Mole on a Friday afternoon. By Saturday morning, I received a consultant report with a working diagnosis of melanoma.
I immediately contacted the patient, who saw her GP on Monday. A two-week wait referral was initiated, and by Friday she had been seen in dermatology. Histology confirmed melanoma, which was surgically excised. This case demonstrates:
Early recognition in aesthetics: the patient had not considered the lesion suspicious.
Value of teledermatology: rapid turnaround expedited diagnosis.
Importance of communication: follow-up ensured timely action.
Impact on outcomes: prognosis is closely tied to tumor thickness at diagnosis.36
reduces delays to diagnosis and directly influences clinical outcomes, particularly for melanoma and high-risk squamous cell carcinoma. For aesthetic practitioners, recognising the limits of scope and prioritising patient safety is critical; lesions of concern should not be treated cosmetically but referred through established medical pathways via NHS GPs and dermatologists. Clear communication, documentation and
adherence to referral guidance helps protect patients, support early intervention and reinforce trust in aesthetic practice as part of a wider healthcare ecosystem.
The rising incidence of skin cancer in the UK places pressure on healthcare services and highlights the urgent need for early detection across all patient-facing specialties.
Medical aesthetics, often perceived purely through an appearance-focused lens, is uniquely positioned to contribute to this effort.
Understanding risk factors – from UV exposure and fair skin types to immunosuppression and family history – allows clinicians to remain especially vigilant in high-risk groups. Recognising the clinical hallmarks of melanoma, BCC, SCC and AKs ensures suspicious lesions are not dismissed or, worse, treated with aesthetic interventions without medical evaluation.

Claire Amos is a registered nurse, independent prescriber and clinical director of CLK Medical Aesthetics in Bridgend. She holds a first-class honours degree and a postgraduate diploma in clinical aesthetics, with more than 15 years of expertise in facial rejuvenation techniques and ethical, evidence-based treatments. Amos also leads Safer Aesthetics Training Academy. Qual: RN, NIP, BSc (Hons) PgDip


FOR HEALTHCARE PROFESSIONALS ONLY
Azzalure® is indicated for the temporary improvement in the appearance of moderate-to-severe glabellar lines seen at maximum frown and/or lateral canthal lines seen at maximum smile in adult patients under 65 years, when the severity of these lines has an important psychological impact on the patient1
*Results from comparative efficacy and safety studies of a single treatment of AboBoNT-A compared with placebo in patients with moderate to severe glabellar lines. The primary end point was reduction to mild or no glabellar lines 30 days after injection of Azzalure.2-4 †AboBoNT-A was first approved for therapeutic use in December 1990 and aesthetic use in April 2009.5-7
References: 1. Clinical Trials. Clinical trials.gov. Study NC!01308060. A Multi-Center Study Of CD07743 for the Improvement of Lateral Canthal Lines (CROW’S FEET). Available at: https://clinicaltrials.gov/study/NCT01308060. Last accessed December 2025. 2. Galderma (UK) Ltd. Azzalure® Summary of Product Characteristics. February 2024. 3. Monheit G, et al. Dermatol Surg. 2020;46:61–69. 4. Brandt F et al. Dermatol Surg. 2009;35:1893–1901. 5. Monheit GD, Pickett A. Aesthet Surg J. 2017;37:S4–11. 6. Kassir R, et al. Dermatol Ther (Heidelb). 2013;3:179–89. 7. Ipsen Biopharmaceuticals, Inc. and Galderma Laboratories, L.P. Dysport® Prescribing Information. September 2023
© 2026 Galderma S.A. All rights reserved. GB-ALD-2500019 | January 2026



Help your patients achieve a natural look they are satisfied with, thanks to Azzalure® anti-wrinkle powder for injection.1,2
Proven reduction of glabellar and lateral canthal lines at 30 days, compared to placebo, with results possible after 2 days*2-4, backed by over 2 decades of trusted experience.†4-7




Aesthetic nurse practitioner Megan Hope explores C-section scar management using radiofrequency and polynucleotides
Caesarean section (C-section) delivery has become one of the most common surgical procedures performed in the UK. National data indicates that between 38% and 42% of all births between 2022 and 2023 in England were delivered via C-section, representing a substantial increase over the past two decades.1 Provisional NHS and audit data suggest that rates continue to rise, driven by a combination of maternal age, medical complexity, patient choice and evolving obstetric practice.2 Globally, similar trends are observed, with the World Health Organization in 2021 reporting a sustained increase in C-section deliveries across both high- and middle-income countries.3
While C-section delivery is often clinically necessary and life-saving, it inevitably results in permanent surgical scarring. For many women, this scar extends beyond a purely physical outcome, influencing body image, comfort, function and psychological wellbeing long after the immediate postnatal period.4 As awareness of long-term scar outcomes grows, medical aesthetic practitioners are increasingly consulted to address both the appearance and symptom burden associated with C-section scars. Advances in energy-based devices and regenerative medicine such as polynucleotides (PNs) and radiofrequency (RF) microneedling have expanded the scope of non-surgical scar management, allowing clinicians to intervene in scar remodelling with greater precision. Understanding the biological and psychosocial context of C-section scarring is essential in delivering safe, effective and patient-centred care.
This article will explore the latest developments in non-surgical management of C-section scars, examining both the biological processes involved and the evolving role of medical aesthetic treatments in improving patient outcomes.
Pathophysiology of
C-section scarring
C-section scars result from a planned surgical incision through multiple tissue layers, including skin, subcutaneous fat, fascia and uterine muscle.5 The most
commonly employed approach in the UK is the low transverse (Pfannenstiel) incision, which is associated with improved cosmetic outcomes and reduced risk of hypertrophic scarring when compared with vertical incisions.5 Despite refinements in surgical technique, scar formation is an inevitable consequence of wound healing.
Cutaneous wound repair occurs through three overlapping phases - inflammation, proliferation and remodelling.6 The inflammatory phase begins immediately following tissue injury and typically lasts several days, during which platelet aggregation and cytokine release initiate fibroblast recruitment and angiogenesis. The proliferative phase generally spans days to weeks post incision and involves deposition of predominantly type III collagen to restore tissue integrity. In the final remodelling phase – which may continue for up to 24 months – collagen fibres reorganise into stronger type I collagen, and vascularity gradually reduces.7
Disruption or dysregulation of the normal wound-healing process can result from factors such as infection, tension on the wound, poor blood supply or genetic predisposition, leading to pathological scarring. Clinically, C-section scars may present as hypertrophic, atrophic or adherent. Hypertrophic scars are raised but confined to the wound edges, atrophic scars appear sunken and adherent scars are tethered to underlying tissues. Associated symptoms can include pruritus, altered sensation, pain or restricted movement.8 Adhesions between superficial and deeper tissue planes are particularly relevant in abdominal scarring and may contribute to chronic discomfort and functional limitation.9
Although surgically distinct from striae distensae, C-section scars share important similarities in dermal pathology. Stretch marks are characterised by disrupted collagen and elastin architecture, reduced fibrillin expression and impaired fibroblast activity; features that may also be observed
in mature surgical scars.10 Both conditions reflect compromised dermal integrity and altered wound-healing responses.11 These shared mechanisms have informed the crossover of treatment modalities, with technologies originally developed for striae increasingly applied to surgical scars. Treatments that stimulate neocollagenesis and dermal remodelling are therefore of particular interest in C-section scar management.
The psychological impact of C-section scarring is increasingly recognised within maternity and women’s health literature. Studies have shown that dissatisfaction with surgical scars may negatively affect body image, self-esteem and sexual confidence, particularly during the postnatal period.12,13 For some women, the scar serves as a persistent reminder of a traumatic or unexpected birth experience, potentially contributing to anxiety, low mood or post-traumatic stress symptoms.13 Patient dissatisfaction is not solely driven by visual appearance. Sensory changes, pain, tethering and loss of bodily autonomy are frequently cited concerns.14 Medical aesthetic practitioners should therefore adopt a trauma-informed, patient-centred consultation approach, ensuring that treatment goals are realistic and aligned with the patient’s physical and emotional priorities. When dissatisfaction with surgical scars significantly affects mood, self-esteem, or daily functioning in the postnatal period, referral for psychological support should be considered. Mild distress may be managed in primary care, but persistent anxiety or depression warrants timely assessment and intervention by specialist perinatal mental health services.15
Topical treatments are often recommended in the early stages of scar formation because they can help optimise the wound environment, maintain hydration and reduce abnormal collagen deposition.16
Silicone gels and sheets remain the most evidence-based option, with systematic reviews demonstrating modest improvements in hydration, erythema and scar pliability.16 Downtime is minimal, with patients able to continue normal activities immediately.17
Evidence for other topical agents, including vitamin E and botanical extracts, remains limited and inconsistent, particularly in established surgical scars.18 As such,


topical therapy alone is unlikely to produce meaningful improvement in mature C-section scars.
Energy-based devices
Energy-based devices have become a cornerstone of aesthetic scar management. RF devices deliver controlled thermal energy to the dermis, leading to collagen denaturation followed by neocollagenesis, elastin production and improved tissue elasticity.19 One notable clinical study supports the use of RF in improving scar texture, colour and pliability, with a favourable safety profile across a range of skin types. Early work demonstrated that RF energy can enhance dermal collagen remodelling and improve scar characteristics in treated areas, with relatively low risk of adverse events.20 Additional clinical evidence from fractional microplasma RF technologies shows significant improvements in scar colour, thickness and pliability in non hypertrophic post burn scars, with high overall response rates and no severe adverse events reported in a prospective cohort of 95 patients.21 Fractional RF approaches have similarly been shown to improve scar assessments using validated tools like the Patient and Observer Scar Assessment Scale (POSAS), underscoring their potential utility in scar management.22 RF treatment is generally suitable for mature, closed C-section scars, particularly in patients without active infection or open wounds. Contraindications include pregnancy, implanted electronic devices (e.g. pacemakers), active skin malignancy or uncontrolled systemic disease. Patients should be counselled on expected outcomes and the potential need for multiple sessions.23 Most patients experience
mild redness or swelling for one to three days, but can resume usual activities shortly after treatment.24
Laser and microneedling Fractional laser and microneedling technologies similarly induce controlled dermal injury, stimulating wound repair pathways and collagen remodelling. Patient suitability varies; fractional lasers are effective for improving texture and pigmentation but carry a higher risk of post-inflammatory hyperpigmentation (PIH), especially in darker skin types. They are generally avoided in pregnancy, recent retinoid use, active infection, inflammatory dermatoses, or in patients with implanted electronic devices. Microneedling has a favourable safety profile across most skin types, with lower dyschromia risk, but should be avoided in active infection, inflammatory skin disease, keloid-prone patients or immunosuppression.25 It is not without potential complications: common side effects include redness, discomfort, dryness or peeling, and there is a small risk of infection, pigmentary change or other adverse events when improperly performed.26 Both modalities may be combined with topical agents or platelet-rich plasma (PRP) to enhance outcomes. Treatment selection should be guided by scar maturity, skin type, patient tolerance and practitioner expertise, with appropriate counselling on expected outcomes and the potential need for multiple sessions. Erythema and peeling typically last five to seven days, requiring brief social downtime.27
Regenerative injectables, including PNs and PRP, represent an evolving area in scar management. PNs have been shown to enhance fibroblast proliferation, angiogenesis and extracellular matrix regeneration, supporting tissue repair at a cellular level.28 When combined with energy-based treatments such as RF, a common approach is to perform the energy treatment first to induce controlled dermal injury, followed by regenerative injectable administration either immediately or within a few days to optimise fibroblast activation and tissue remodelling.27 Typical treatment intervals range from four to six weeks, depending on scar maturity and patient response.
Emerging evidence suggests that such combination strategies may enhance clinical outcomes compared with either modality alone. Injection site erythema or mild swelling may occur for 24-48 hours, but routine activities can continue.29 However, current studies are limited by small sample sizes, heterogeneous protocols and short follow-up periods, and robust, large-scale trials are needed to establish optimal regimens.
A 37-year-old female patient presented five years post-partum following her own independent research into regenerative aesthetic treatments, specifically injectable PNs and RF microneedling. Her primary motivation was to address long-standing textural skin concerns rather than pursue camouflage-based or surgical interventions. During consultation, a detailed discussion was held regarding combination treatment strategies and the synergistic role of biostimulatory injectables and energy-based devices in improving scar quality and dermal architecture.
A shared decision-making approach was adopted, with the agreed treatment plan focusing on two primary concerns: post-pregnancy stretch marks (striae alba) affecting the lower abdomen, and a residual C-section scar.
On clinical examination, the C-section scar was mature, pale and flat, with residual firmness and textural irregularity but no evidence of hypertrophy or keloid tendency (Figure 1). Stretch marks were consistent with striae alba, demonstrating dermal thinning, reduced elasticity and altered skin quality. No active inflammation was present. Despite natural improvement over time, the patient reported ongoing emotional discomfort and reduced confidence when exposing her abdomen, highlighting the psychosocial impact of post-surgical and post-pregnancy scarring.30
Treatment selection should also consider contraindications, including active infection, inflammatory dermatoses, pregnancy and implanted electronic devices, and whether combination approaches with regenerative injectables are planned to enhance outcomes.31
Injectable PNs were selected as an adjunctive regenerative therapy to biologically support tissue repair. PNs stimulate fibroblast proliferation, enhance extracellular matrix synthesis, improve dermal hydration and elasticity and exert antioxidant and anti-inflammatory effects.32 When administered immediately following RF microneedling, PNs may take advantage of increased skin permeability
and an activated wound-healing cascade, optimising regenerative signalling.33
Alternative options, including topical therapies, fractional laser resurfacing PRP and surgical scar revision, were considered but not selected due to limitations in penetration, downtime and variability of outcomes or patient preference.
3D Aesthetics Dermaforce RF microneedling was selected as the primary energy-based modality due to its ability to deliver controlled thermal energy into the dermis, stimulating neocollagenesis and elastin remodelling. 34 This modality is particularly effective for mature scars and striae alba, where collagen reorganisation and dermal thickening are required rather than pigment correction alone.
PhilArt (Croma Pharma) was selected due to its strong safety profile, high-purity, highly polymerised PNs (PN-HPT technology), supporting data and tissue tolerability. The product contains 40mg of PNs in 2ml (20mg/ml), providing consistent, standardised regenerative support. PhilArt has a well-established safety profile, with high-purity, highly polymerised polynucleotides (PN-HPT technology) minimising the risk of local or systemic adverse reactions. Clinical and preclinical data indicate good tissue tolerability, with injection-site reactions typically limited to mild, transient erythema or swelling that resolve spontaneously. 35
RF microneedling was delivered using a progressive treatment strategy, with gradual escalation of both needle depth and energy parameters across sessions in order to maximise dermal remodelling while minimising adverse effects. The maximum needle depth reached was 2.5mm, reflecting the need to access the reticular dermis, where both mature scar tissue and striae alba are primarily located. A study demonstrated that effective treatment of scars and stretch marks requires penetration beyond the superficial dermis, with depths of approximately 1.5-2.5mm shown to be optimal for stimulating collagen reorganisation and dermal thickening. 36
Depth escalation was undertaken progressively to allow controlled mechanical and thermal stimulation while reducing the risk of excessive inflammation, discomfort or PIH.
Adjustable-depth RF microneedling enables precise targeting of dermal layers and is particularly suited to mature scars, where collagen disorganisation rather than pigment alteration is the primary pathological feature. 37
Energy settings were selected to deliver sufficient thermal energy to induce collagen denaturation, a critical precursor to neocollagenesis within the wound-healing cascade. RF energy generates heat within the dermis while sparing the epidermis, triggering fibroblast activation, new collagen synthesis and subsequent improvement in scar texture and elasticity.³ Progressive energy escalation across treatment sessions has been shown to improve patient tolerance and support cumulative dermal remodelling, aligning with evidence supporting staged RF protocols for scar management. 38
This depth- and energy-controlled approach allowed for effective structural intervention while maintaining a favourable safety profile, particularly important in abdominal skin where dermal thickness and scar architecture may vary. Treatment was delivered over five sessions, each consisting of RF microneedling followed immediately by injectable PN therapy within the same appointment. Sessions were spaced at approximately four-week intervals, in line with evidence supporting staged energy-based treatments to allow for collagen remodelling and tissue recovery. 39 Standardised pre- and post-treatment photography was obtained under consistent lighting, positioning and camera settings to allow objective comparison of clinical outcomes ( Figure 2). Potential adverse effects were discussed in detail as part of the informed consent process. Expected transient effects of RF microneedling included erythema, mild oedema, pinpoint bleeding and short-lived discomfort, with rare risks of infection or PIH.40 PN treatment risks included mild swelling, temporary erythema, localised bruising at injection sites and rare hypersensitivity reactions.41 Comprehensive post-procedure aftercare advice was provided, and the patient tolerated all sessions without complication. This included keeping the area clean and moisturised, avoiding direct sun exposure and applying broad-spectrum sunscreen once erythema resolves. The patient was advised to avoid strenuous exercise, saunas or hot baths for 24-48 hours to reduce the risk of swelling or irritation, and to monitor transient redness, mild swelling or tenderness, which generally resolve within a few days; however, she could contact the clinic at any time if concerned.41 The patient was counselled that while significant improvement was achievable, complete removal of stretch marks or scarring was unlikely. Treatment goals focused on improved texture, tone and skin quality rather than total erasure,
with emphasis placed on regeneration, gradual improvement over time and the importance of completing the full treatment course.
Following a structured treatment course combining RF microneedling and PN therapy, the patient demonstrated marked improvement in stretch mark appearance, dermal thickness and elasticity, alongside a softer, flatter and less conspicuous C-section scar (Figure 2). Subjective patient feedback and objective photographic assessment confirmed significant aesthetic and psychosocial benefit.
If repeating this case, the treatment protocol could be further optimised by extending the number of RF microneedling sessions to allow for additional cumulative collagen remodelling, particularly in areas of established dermal thinning. Introducing supplementary PN treatments at two-week intervals between RF sessions may enhance regenerative signalling during the active wound-healing phase, supporting fibroblast activity and extracellular matrix synthesis. Increasing the overall PN volume across the treatment course could further improve dermal hydration, elasticity and tissue quality, potentially leading to more sustained and pronounced clinical outcomes.
As C-section rates continue to rise, long-term scar management is becoming an increasingly relevant concern within aesthetic practice. Advances in energy-based devices and regenerative injectables now allow practitioners to address both dermal structure and skin quality more effectively.

Megan Hope is an aesthetic nurse practitioner and has a bachelors of science in adult nursing, qualifying in 2017 from Oxford Brooke’s University. She is a key opinion leader for 3D Aesthetics and takes a holistic, patient-centred approach to care, delivering natural, balanced results using injectables and energy-based devices. Hope is the founder of MCH Clinic in Norfolk and codirector of The Nurses Network, with a strong interest in regenerative and evidencebased treatments.
Qual: BSC adult nursing














As medical aesthetics shifts to prejuvenation, clinicians seek technologies that support skin health before visible ageing. Collagen banking is the cornerstone. This article explores why early, repeatable collagen stimulation matters, how RedTouch Pro’s selective wavelength can improve outcomes and deliver results and sustainable growth.
Medical aesthetics traditionally focused on treating visible ageing once it appears. Today, clinical and client expectations are shifting towards earlier intervention and long-term skin health.
From the mid-twenties, collagen production begins to decline steadily.1 By the time ageing becomes apparent, a proportion of collagen has been lost. Collagen banking supports skin structure before damage becomes difficult or costly to correct. This shift created demand for technologies that stimulate collagen safely and repeatedly – without downtime or tissue trauma. This is where RedTouch Pro stands apart: the world’s first laser using a 675nm wavelength to directly target collagen as a chromophore.2
Collagen banking reframes rejuvenation as a long-term strategy rather than short course corrective treatments. It relies on regular maintenance to preserve structure, quality and resilience.
For clinics, this requires repeatable, client-friendly and commercially viable technology. Many traditional energy-based devices stimulate collagen indirectly by heating water in the skin, which can increase discomfort, downtime and limitations on treatment frequency.1 By directly targeting collagen, RedTouch Pro delivers stimulation with minimal collateral damage, supporting prejuvenation while maintaining a positive client experience.3




Why clinic owners are investing in RedTouch Pro

RedTouch Pro is designed for modern aesthetic practices, balancing clinical innovation with real-world business performance. Demonstrated by Dr Aggie Zatonska, Atelier Clinic, “RedTouch Pro is a true innovation and a one-of-its-kind technology that directly stimulates collagen. It has reshaped our approach to prejuvenation, offering a pain-free, no-downtime treatment suitable for a wide range of patients and indications. RedTouch Pro can be used both as a standalone modality and in conjunction with other treatments, as well as for ongoing maintenance, allowing us to create bespoke, preventative treatment plans tailored to individual patient needs.”
A clear point of difference
The exclusive 675nm wavelength makes RedTouch Pro the first laser to target collagen directly, giving clinics a defensible USP in a crowded market.1
High-demand treatments, without downtime
No needles. No anaesthetic. Minimal recovery. Comfortable, walk-in/walk-out treatments are easier to sell, easier to repeat and easier to build into long-term plans.
One device, multiple revenue streams
By combining biostimulation and collagen remodelling in one platform, RedTouch Pro supports prejuvenation and corrective indications, attracting younger prevention-led clients while delivering results for established clients.2,3
Treat more clients with confidence
Adjustable energy levels and multiple treatment modes make RedTouch Pro safe for Fitzpatrick skin types I–V, allowing clinics to treat broader demographics without additional devices.
Predictable costs. Strong margins. Faster ROI
No consumables and fast treatment times, RedTouch Pro offers visibility on running costs and supports scalable, sustainable profitability.
Supporting a range of treatments, including:
· Prejuvenation/collagen banking
· Melasma and pigmentation
· Acne scarring
· Open pores and textural irregularities
· Lines and wrinkles
· Stretch marks
Preventative protocols focus on maintaining collagen reserves and skin quality, while corrective concerns typically involve short treatment courses before transitioning into collagen banking programmes.4 This flexibility allows clinics to support long-term client journeys rather than one-offs.

An early adopter of the RedTouch Pro is Dr Ariel Haus, “At my Harley Street clinic, I only invest in technologies that deliver genuine results with clinical integrity. RedTouch Pro is the first laser I’ve seen that truly targets collagen at its source. My patients value the natural, progressive results – firmer, healthier skin with no downtime – and they appreciate the comfort of the treatment. I chose to partner with Lynton because their innovation is backed by decades of scientific rigour, and RedTouch Pro represents a new gold standard in non-invasive skin rejuvenation.”
From a business perspective, RedTouch Pro integrates seamlessly. Broad client appeal, repeatable protocols and high satisfaction rates support consistent rebooking and long-term treatment plans. As aesthetics continues to move towards prejuvenation, RedTouch Pro allows clinics to preserve skin quality for the future.























































Mr Lorenzo Garagnani shares his protocol for restoring hydration and elasticity

Ageing hands are among the most visible indicators of age and yet can be frequently overlooked in facial-focused aesthetic practice.1 This is largely due to limited practitioner familiarity with hand anatomy and aesthetic indications, as well as low patient awareness of available treatment options.
Frequently, patients report dissatisfaction with changes in the hands such as skin thinning, crepiness, volume loss, fine lines and dehydration. 2 These changes are largely driven by a combination of environmental damage – such as sun damage, contact with harsh chemicals and exposure to extreme climate – and by ageing and hormonal changes leading to reduced collagen production, impaired skin barrier function, dermal thinning and elasticity loss. 3,4
With the growing preference for more natural, regenerative approaches, polynucleotides (PNs) offer a promising solution for hand rejuvenation. This article explores the anatomical considerations, clinical rationale and technique behind a dual layer PN injections approach.
Hand ageing is driven by both intrinsic and extrinsic factors, and is complicated by the hands’ constant use, which demands outcomes that are subtle, durable and safe. With age, dorsal hand skin becomes thinner and more fragile due to natural tissue ageing, dehydration and cumulative environmental damage.5 Collagen and elastin degradation lead to laxity and fine wrinkling, while a compromised epidermal barrier increases transepidermal water
loss, resulting in dryness and rough texture.6 Clinically, patients present with volume loss, prominent veins and tendons, crepey skin, reduced firmness and diminished skin resilience. 3,4
Treatment is individualised following comprehensive assessment.7 Patients with active or chronic infection, acute inflammation or known allergy or hypersensitivity to injectables are excluded.8 Active infections must be treated medically before any aesthetic intervention.8 Those with inflammatory conditions may benefit from a bespoke skincare plan aimed at reducing local tissue inflammation, carefully tailored to avoid components that could exacerbate the condition.8 Visual evaluation includes vein, tendon and bone prominence, hand contour and presence of muscular wasting.9
Skin quality is further assessed using a pinch test to evaluate hydration, with delayed recoil indicating reduced hydration.10 In such cases, subdermal treatment aimed at improving hydration may be indicated.11 Thinner or lax skin may benefit from a combined dermal and subdermal approach, while well-hydrated hands with crepiness or early thinning may respond to dermal treatment alone to improve firmness, elasticity and texture.11
Several treatment modalities are used for hand rejuvenation:
· Dermal fillers: Dermal fillers restore volume to ageing hands, softening the appearance of prominent veins and tendons. However, they mainly address
Clinical Technique Hand Treatment
volume loss and may be less suitable for crepey or lax skin if hydration and dermal structure are not also improved. Optimal results require careful patient selection, proper injection technique and clear counselling on realistic outcomes and potential side effects.12 Skin boosters: Skin boosters improve skin quality and hydration but may offer limited collagen stimulation unless they contain specific biostimulatory components. Some formulations include calcium hydroxylapatite or similar agents to promote collagen production, whereas standard hyaluronic acid-based skin boosters primarily provide hydration without enhancing collagen synthesis.13
Energy-based devices (EBDs): EBDs (fractional radiofrequency for tightening, intense pulsed light for pigmentation) are also effective when safely combined with PNs to enhance overall results.14 Patients with allergies or hypersensitivities may be considered for non-injectable alternatives, such as EBDs or carefully screened skincare products.8 Key considerations for energy-based aesthetic treatments include patient selection, skin type and anatomical safety.14 In terms of general treatment indications, patients requiring contouring of the hand due to dorsal muscular wasting and intermetacarpal guttering typically benefit from dermal filler injections, whereas patients requiring more superficial skin and subcutaneous tissue rejuvenation with reduction of the creases and improved local hydration can be treated either with traditional skin boosters or with PNs.12-14 Additionally, there are patients requiring biostimulation with increased collagen production. Due to their ability to support fibroblast activity and the ability to enhance extracellular matrix integrity, PNs are the chosen option for the treatment of this specific cohort of patients.10
PNs are emerging as a valuable treatment modality for ageing hands due to their regenerative, reparative and biostimulatory effects on the dermis.15 As regenerative agents, they address underlying dermal health, improving skin texture and hydration, and may be used alone, in combination with other treatments or to prepare the skin for further intervention when required.15 Key considerations for optimal outcomes include thorough assessment of skin quality and age-related changes, appropriate injection technique and depth and clear patient counselling regarding realistic expectations and treatment timelines.15,16 Composed of highly purified DNA fragments, PNs act at a
Clinical Technique
Hand Treatment
cellular level to stimulate fibroblast activity, enhance collagen and elastin synthesis and improve extracellular matrix integrity.15 Ageing hands commonly demonstrate dermal thinning, textural changes, reduced elasticity and increased visibility of tendons and veins.15
Unlike volumising agents, PNs aim to improve overall skin quality by promoting hydration, elasticity and tissue resilience without altering anatomical contours.15 In addition, their anti-inflammatory and antioxidant properties support tissue repair in photodamaged skin.15
Example protocol
Clinical outcomes include improvements in skin firmness and elasticity, hydration and visible reduction in fine creases on the back of the hands, as demonstrated in Figure 1 15
The Skin Booster-Polynucleotide
Anatomically Based (B-PAB) technique is used for dual-layer hand rejuvenation with PN-based products. This combines intradermal needle injections of PNs with subdermal cannula delivery of either a PN-HA combination product or a HA skin booster, to simultaneously restore hydration and improve skin quality.17 This method is adapted from previously described anatomically based injection approaches (B-FAB technique) and allows precise, multi-layered delivery of regenerative products.17
Patients are typically seated upright with their hands flat on a clean surface below heart level to optimise visualisation and ensure even product distribution.18 For those who prefer not to observe the procedure, treatment can be performed with the patient supine. Local anaesthetic cream is applied to the dorsal hand for 30 minutes prior to injection.19
The superficial subcutaneous layer
· Product: Newest (1ml per hand).
· Delivery: 25G cannula.
Plane: Very superficial subcutaneous, in the superficial dorsal subcutaneous lamina (DSL), just beneath the dermis (subdermal injection).17
· Technique: Linear threading through four separate entry points, using a cannula (e.g. a 25G, 40mm or 50mm long – with length based on individual patient’s hand size – cannula placed in the superficial dorsal subcutaneous lamina layer) in the intermetacarpal region on the dorsal hand.17
The dermal layer
· Product: Plinest (1ml per hand).
· Delivery: 30G 4mm needle, allowing superficial delivery.17
Plane: Intradermal (superficial dermis).17
· Technique: Nine bolus injection points are placed over the dorsum of the hand in specific anatomical locations. Inject 0.1ml in each of the eight dorsal points of the hand and 0.2ml in the wrist point.17
Achieving the correct intradermal depth is crucial. The needle should be inserted at a shallow angle, of no more than 45 degrees with the skin surface, advancing only the tip to prevent over-diffusion. The dermis and the superficial dorsal subcutaneous lamina are distinct layers, and each product is injected separately into its respective layer. Both products are delivered in a single session using a two-layer approach.
Results
While hand-specific clinical trials are limited, emerging facial rejuvenation data with PN-HPT offers a solid basis for expected clinical outcomes.17
A 2024 prospective study on 30 patients (with the average age being 40) receiving intradermal PN-HPT injections reported significant improvements in skin tone, firmness, elasticity and radiance, beginning at four weeks and sustained through six months. 20 The treatment was well tolerated with no serious adverse events, and patient satisfaction scores were high. 20 While these results were documented on the face, the mechanism of action, fibroblast stimulation, collagen synthesis and tissue hydration, applies equally to the dorsum of the hands, which experience similar age-related degradation.
Patients typically undergo three to four sessions, spaced three to four weeks apart, with peak results appearing two to three months after the final treatment. Single sessions generally do not produce significant improvement, making multiple treatments standard for both PNs and skin boosters.15 Maintenance treatments every six months help preserve improvements over time.15
Although current data shows benefits lasting up to six months, longer-term studies are needed to confirm sustained PN effects in the hands, which age more rapidly due to constant use and individual activity patterns. 20 As a general recommendation, just like for any other aesthetic procedure, patients should adopt a generally healthy lifestyle, reducing the factors that enhance skin ageing and skin damage. 21

Before After

1: 53-year-old female
After treatment, it is important to minimise risk of infection and optimise healing by following appropriate post-procedure care. Patients are advised to:15
· Avoid strenuous hand use: Includes heavy lifting or any activities requiring load-bearing, gripping, pushing or pulling with the hands for at least 72 hours.
· Refrain from contamination risk activities: Such as gardening, DIY, dishwashing without gloves, or gym/ physical exercise for at least 72 hours, or until injection sites have fully healed.
· Avoid non-sterile topical products: Avoid until the injection sites are fully healed, in order to reduce the risk of injection site infection.
· Avoid immersion in chlorinated water, steam rooms or saunas: Avoid for at least 72 hours, or until injection sites have fully healed, to avoid irritation and reduce the infection risks.
Minimise sun exposure: Apply SPF – minimum SPF 30 – regularly to the hands.
As the hands are in constant contact with surfaces, the risk of bacterial contamination is higher than in other treated areas.15,22 Ensuring sterility during the procedure and maintaining good hygiene post treatment is essential for preventing complications such as infection or irritation.15,22
The dorsum of the hand is a delicate and anatomically complex area with minimal subcutaneous fat, making underlying structures – extensor tendons, superficial veins, arteries and sensory nerves – more prominent and vulnerable. With age, progressive collagen and elastin loss further thins and fragilises the skin. 23
Beneath the dermis lies a thin subcutaneous fat layer divided into three laminas by fascia. The DSL is the preferred plane for PN injections using a cannula, as it lies above the dorsal veins and nerves.24 A fascial layer separates the DSL from the dorsal intermediate lamina (DIL), providing an added safety barrier. Using a cannula rather than a needle in the DSL further reduces the risk of vascular or nerve injury.17,18 The superficial dorsal venous network and dorsal branches of the radial and ulnar nerves are located in the DIL; injections should be avoided in this layer.24
For intradermal injections, a shallow angle and minimal depth are essential to prevent over-diffusion or injury to deeper structures. Superficial subcutaneous placement should remain just beneath the dermis within the DSL to ensure even distribution and safety. Incorrect plane selection or product placement can compromise outcomes and increase the risk of vascular, nerve, tendon or muscular injury, although soft, biocompatible PNs may present a lower risk of vascular compromise than thicker gels.24 Strict aseptic technique is critical due to the hand’s high microbial exposure.
Patient contraindications
PN treatment should be avoided in patients with known allergy or hypersensitivity to fish or any product components.15 Active infection, inflammation or compromised skin integrity at the treatment site are contraindications. Careful patient selection and thorough medical screening are essential prior to treatment.
Potential adverse events
PN-HPT products are generally well tolerated; however, practitioners should remain aware of possible adverse events. Bruising may occur due to proximity to superficial vessels, with incidence similar to other treated areas. 2 Swelling or oedema is typically transient. 22 Rare allergic reactions may occur.15 Some patients report temporary dorsal tension or stiffness following treatment. 22
A thorough understanding of hand anatomy, appropriate injection technique and strict adherence to sterile protocols are essential for minimising complications and achieving safe, consistent outcomes.
This layered PN injection technique offers natural-looking hand rejuvenation,
enhancing a younger and healthier appearance. For patients who have had facial treatments or engage in frequent social interaction, hand rejuvenation can boost self-confidence and complement a holistic aesthetic plan, improving both appearance and the perception of hand function.
However, it’s important to note that current evidence supporting PN hand rejuvenation is largely extrapolated from facial applications. Hand-specific clinical trials are required to confirm efficacy and establish optimal treatment protocols.

Mr Lorenzo Garagnani is a consultant hand and wrist surgeon and a founder of the OrthoPlastic Hand Unit at Guy’s & St Thomas’ NHS Foundation Trust in London, as well as honorary reader at the Faculty of Life Sciences & Medicine of King’s College London. Additionally, he serves as medical director at SE1 Medical Aesthetics in London.
Qual: MBE, OSI, MD, FRCS, PGDip (Aesth. & Well. Med.), PGCert (HCP Exec. Leadership), EBHS Hand Surgery Diploma

For many women entering their 40s and 50s, changes in body composition emerge rapidly and often unexpectedly. As aesthetic professionals, we recognise the multifactorial nature of perimenopausal weight gain – yet for clients, the emotional impact can be profound.
Body contouring and wellness practitioner Jasmina Connelly has built her clinical philosophy around addressing one of the most misunderstood challenges in this demographic – cortisol-driven abdominal fat.1
“In my clinic, most of my clients are mature women navigating perimenopause or menopause,” Connelly says, explaining, “The abdomen is always the primary area of concern. These women are doing everything right, yet the belly feels impossible to shift.”
Understanding cortisol belly
Connelly emphasises that this presentation is rarely a simple consequence of diet or exercise. “So many women at this stage of life are living in a constant state of stress. Chronically elevated cortisol signals the body to store fat around the abdomen – it’s the classic fight-or-flight response,” she notes.2 “If cortisol stays high, the body will not burn that fat, no matter how much they diet.”
Her clinical work begins with a detailed consultation that considers hormonal status, medication, lifestyle, tissue integrity and the patient’s nervous-system baseline. “There is no one-size-fits-all approach. Every plan must be tailored, especially when cortisol is a driving force.”
Device-led precision meets physiological reset
To target resistant abdominal adipose tissue, Connelly relies on the Zemits Abigon Cavitation system, which she describes as her “go-to technology” for stubborn belly fat in perimenopausal and menopausal clients. But she is clear that cavitation alone is rarely enough.
“My secret weapon – the tool that truly transforms results – is pressotherapy,” she says. Connelly elaborates, “It doesn’t just move stagnant fluid. Pressotherapy directly influences the parasympathetic nervous system.3 When clients enter rest-and-digest mode, cortisol finally drops. Then the body can let go of retained fluid and begin using stored fat as energy.”4
Vacuum therapy is incorporated to stimulate circulation and soften fibrotic pockets, followed by radiofrequency later in the programme to address laxity as the circumference reduces.5 The integration of wood therapy and manual sculpting provides additional contour refinement.5
“I see remarkable improvements not only in measurements, but also in digestion, sleep quality and inflammatory symptoms. When the nervous system is regulated, everything changes.”
Case study: A 12-week cortisol-focused belly programme
One recent client, aged 55, underwent a structured 12-week plan designed to support both metabolic and nervous-system balance.
Weekly in-clinic protocol
· Cavitation, vacuum therapy and hands-on sculpting (including wood therapy and Brazilian techniques)
Bi-weekly treatments:
· Pressotherapy and manual lymphatic drainage
Home care:
· Daily dry brushing
· Vibration plate use
· Pressotherapy twice weekly
· Topical fat-burning cream
Lifestyle enhancements:
· Dietary adjustments
· Long walks
· Weekly yoga to reinforce parasympathetic activation
The outcome
A two-dress-size reduction, reduced fluid retention, improved digestion and sleep and a visibly softer abdominal contour.


A shift in aesthetic philosophy
Connelly welcomes the broader specialty move toward holistic, system-informed body contouring. “We’re no longer just reducing inches. We’re supporting women in reclaiming confidence during a vulnerable stage of life,” she says. “Our work becomes meaningful when we recognise the emotional and physiological layers behind every abdomen we treat.”
At Zemits UK, practitioners like Connelly remind us that excellence in body contouring lies not simply in the device but in the clinician’s ability to interpret the body’s stress signals and deliver interventions that restore balance and shape.

Expert insights from Jasmina Connelly
Body Contouring & Wellness Practitioner
| Founder, Roseline
Training Academy | Zemits UK Ambassador


Title: Prospective Single-Site Open-label Study Assessing Safety and Efficacy of Poly-L-Lactic Acid for Temple Volume Loss
Authors: Suleima Arruda, et al.
Published: Journal of Drugs in Dermatology: JDD, January 2026
Keywords: Facial fat, Poly-l-lactic acid (PLLA), Volume loss Poly-l-lactic acid (PLLA) is an injectable biostimulatory filler used for restoring facial fat volume loss. To evaluate the safety and efficacy of injectable PLLA injections for volume loss in the temples using dual plane injections. Assessments included live ratings and ratings of standardized pictures and ultrasound imaging at weeks 4, 8, 12, and 16 by a trained evaluator. At the 8-week follow-up, there was a statistically significant increase in temporal volume and improvement in skin elasticity in PLLA-treated subjects. Treatment was well-tolerated with minimal self-resolving adverse effects. Ultrasound imaging confirmed that the injection plane was free of vasculature, posing no safety risk. Repeated PLLA treatments in the temporal region elicited a global improvement in facial shape, particularly the mid and upper face region. The temple hollowness and facial laxity improved over time with no safety sequelae.
Title: Mental Health Outcomes in Obesity Interventions with GLP-1 Receptor Agonists: Is It Similar to Other Obesity Interventions? A Narrative Review with Systematic Evidence Synthesis
Authors: Darin Osborne, et al.
Published: International Journal of Obesity, January 2026
Keywords: GLP-1 receptor agonists, Mental health, Obesity
This narrative review synthesizes the evidence on the psychological impact of lifestyle, pharmacological, and surgical interventions in the treatment of obesity. Special focus is placed on glucagon-like peptide-1 (GLP-1) receptor agonists, given their rising global use and emerging concerns regarding mental health safety. Studies examining psychological outcomes in patients undergoing lifestyle modifications, pharmacotherapy, or bariatric surgery for weight loss were included. Behavioral interventions consistently showed no harm to mental health and demonstrated modest improvements in depression and mental health-related quality of life. Bariatric surgery was associated with short-to-medium-term reductions in depressive and anxiety symptoms, though long-term benefits were attenuated, with some studies reporting increased suicidality after five years. The GLP-1 receptor agonists (Semaglutide, liraglutide, Tirzepatide) have shown an improvement in patient-reported mental wellbeing in several trials. Concerningly, pharmacovigilance data initially suggested a possible link with suicidality; however, subsequent robust cohort studies and meta-analyses have refuted this association. The current evidence suggests that most weight loss interventions are psychologically safe or beneficial, but long-term data remain limited, particularly for GLP-1 receptor agonists.
Title: A Real-Life Assessment of Injectable Polynucleotides High Purification Technology in Aesthetic Medicine for Skin Rejuvenation
Authors: Lanza Eliana, et al.
Published: Journal of Cosmetic Dermatology, January 2026
Keywords: Polynucleotides, Skin quality, Skin rejuvenation
To assess the real-world performance and safety of Plinest (40 mg/2 mL of PN HPT in a 2 mL pre-filled syringe), a CE-marked class III medical device for skin rejuvenation of the face, neck, and décolleté. This observational clinical data collection involved 66 adult patients, each of whom could receive treatment in up to three areas (face, neck, décolleté). Patients underwent three sessions of intradermal PN HPT injections. A total of 106 questionnaires were collected: 47 for the face, 33 for the neck, and 26 for the décolleté. Performance was evaluated using the Global Clinical Improvement Scale (GCI-S) and Global Aesthetic Improvement Scale (GAIS). Safety was monitored through spontaneous adverse event (AE) reporting. Clinician-reported outcomes showed visible improvement in 100% of facial treatments, with 53.5% rated as “marked” or “excellent.” In the neck and décolleté areas, moderate to significant improvements were observed in over 93% and 88% of cases, respectively. Patient satisfaction ranged from 97% to 100%. No serious AEs occurred.PN HPT demonstrated a favorable tolerability and performance profile in real-life aesthetic practice, supporting its role in improving skin quality and reducing signs of aging.
Title: Cutaneous Sensory Loss After Lipoabdominoplasty: A Prospective Quantitative Mapping Study with Functional and Quality-of-Life Correlations
Authors: Agostino Bruno, et al.
Published: Aesthetic Plastic Surgery, January 2026
Keywords: Abdominoplasty, Quantitative sensory testing, Scarpa’s fascia
This study aimed to prospectively map sensory changes following lipoabdominoplasty and evaluate the influence of Scarpa’s fascia preservation on recovery trajectories and quality of life. A prospective single-center study was conducted on 60 patients (mean age 42.7 years; 93.3% female) undergoing 360-degree liposuction and lipoabdominoplasty. At 1 month, 93.3% of patients exhibited sensory impairment, most pronounced in the infraumbilical medial (Zone 8), suprapubic (Zone 11), and supraumbilical midline (Zone 5) regions. Recovery progressed steadily: residual deficits persisted in 72.5% at 3 months, 55.0% at 6 months, and 21.7% at 12 months. Preservation of Scarpa’s fascia significantly improved sensory outcomes, with better tactile thresholds (Zones 5 and 8 at 6 months, p < 0.05), faster thermal recovery (Zone 11 at 3 months, p = 0.041), and fewer impaired dermatomes at late follow-up (p < 0.05). Cutaneous sensory loss is an almost universal early sequela of lipoabdominoplasty but typically resolves within 12 months. Preservation of Scarpa’s fascia confers measurable neuroprotective effects, reducing long-term deficits and enhancing patient satisfaction.
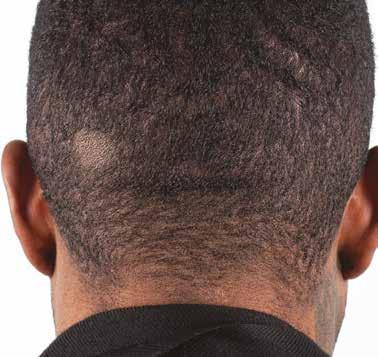
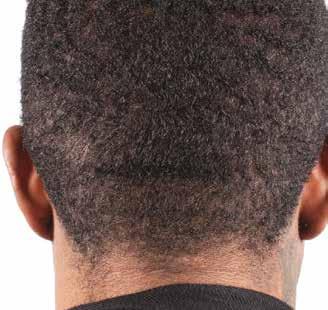
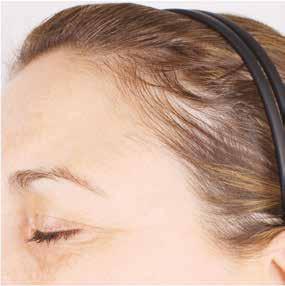


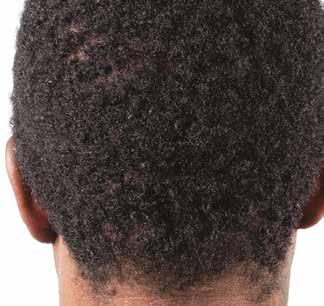






Psychodermatology is the study of the complex, bidirectional relationship between psychological processes and skin health.1-4 It examines how psychological states such as stress, anxiety, self-esteem and body image influence cutaneous function, while also recognising how skin conditions can profoundly affect emotional wellbeing.1,4
In medical aesthetics – where patients seek visible change often closely linked to personal identity – this relationship is particularly significant. Many patients pursue aesthetic treatments not only to alter their appearance, but to improve confidence, self-perception and emotional comfort. This is further supported by research, with studies involving several hundred to over 1,000 participants indicating that approximately 60-70% of aesthetic patients pursue treatment primarily for psychological reasons, such as enhanced self-esteem and social confidence.5,6 When psychological influences are overlooked, treatments may fail to deliver the outcomes patients expect, despite being technically correct.1,4,9,10
Recognising these mind-skin interactions provides aesthetic practitioners with an essential framework to enhance patient care, supporting more holistic treatment outcomes without diminishing the importance of physical dermatology.1
Psychological stress commonly manifests through clinically relevant changes in the skin, particularly during periods of acute or chronic life stress such as bereavement, relationship difficulties, workplace pressure, financial strain or ongoing caregiving responsibilities.
Chronic activation of the hypothalamic –pituitary–adrenal (HPA) axis elevates cortisol and stress-related neuropeptides, disrupting epidermal lipid synthesis, impairing corneocyte cohesion and weakening tight junctions. This results in increased transepidermal water loss, heightened sensitivity, delayed wound healing and a pro-inflammatory cutaneous environment.2,3,7
In aesthetic practice, this physiological dysregulation may reduce treatment efficacy and lead to exaggerated post-procedure responses or slower, less predictable improvement despite appropriate technique.2,3,8 Clinically, this often necessitates more conservative treatment plans, extended recovery periods and closer follow-up, underscoring the importance of psychologically informed treatment timing and expectation management.1,4,8
These effects may present as dull or uneven skin texture, exaggerated erythema, prolonged downtime, increased reactivity or inconsistent responses to standard treatment protocols. While such
outcomes are often attributed to procedural factors alone, they may instead reflect underlying emotional stress influencing skin physiology.2,3,8
Psychological stress also plays a role in pigmentary disorders. Stress-induced neuropeptides, including corticotrophin-releasing hormone and substance P, stimulate melanocyte activity and increase melanogenesis.3 Combined with barrier dysfunction and inflammation, this neuroendocrine disruption can exacerbate conditions such as melasma or post-inflammatory hyperpigmentation, making them more resistant to conventional aesthetic interventions.9
Sustained or recurrent psychological distress may accelerate intrinsic skin ageing. Impaired collagen synthesis, increased oxidative stress and chronic inflammation reduce elasticity and skin resilience, contributing to fine lines and other age-related changes, even in patients with good skincare adherence.2,3,7
Aesthetic practitioners are not expected to diagnose mental health conditions, but psychological awareness during consultations is essential.1,6 Emotional distress can influence skin perception and treatment expectations. Patients may exhibit distress disproportionate to clinical findings, persistent dissatisfaction despite multiple treatments or heightened anxiety focused on minor imperfections.1,4,10
By identifying emotional distress that may influence skin perception, healing and expectations, psychological assessment supports psychodermatological care by aligning treatment decisions with both cutaneous physiology and patient wellbeing.1,4
Leveraging the consultation process
Psychodermatology can be integrated seamlessly into aesthetic consultations through subtle but meaningful shifts in communication. The consultation becomes not only a clinical assessment, but also an emotional one – an opportunity to understand the psychological landscape behind a patient’s aesthetic concerns.11 Consultations often reveal the emotional weight patients carry, and recognising when motivations are emotionally driven or when expectations may be unrealistic is fundamental to safe and ethical practice. While many individuals seek treatment for appropriate and healthy reasons, some may display distress that is disproportionate to the perceived flaw. This may indicate underlying conditions such as body dysmorphic disorder (BDD),
anxiety or depression.4,6 Practitioners are not expected to diagnose these conditions, but they should be trained to recognise potential red flags and respond appropriately.10 In the UK, appropriate training includes psychodermatology CPD, education in body dysmorphic disorder (BDD) awareness and consultation-skills training, alongside familiarity with NHS talking therapies referral pathways. Together, these competencies support safe and ethical aesthetic practice while remaining within professional scope.
Practical steps include:
· Allowing adequate time, typically 30-45 minutes, to explore emotional motivations.
· Asking open-ended questions, such as, “How long have you felt this way about your skin?” or “What would feeling better about your appearance mean for you?”
Observing non-verbal cues, including avoidance of eye contact, visible distress, anxiety or agitation, tearfulness and tense body posture.
· Recording relevant emotional context in treatment notes to support clinical decision-making. This may include documenting observed anxiety or distress, recent life stressors or heightened concerns that could influence expectations, healing or treatment suitability.
Following up post treatment (around the two to four week mark) to evaluate emotional satisfaction, as well as physical outcomes.
Such practices strengthen the practitioner–patient relationship by fostering trust and transparency. Within psychodermatology, the consultation helps identify how emotional state may influence skin function, treatment response and satisfaction, supporting more individualised care.11
Managing patient expectations
Expectation management is a cornerstone of ethical and effective aesthetic practice. Psychological state significantly influences how patients interpret outcomes, meaning technically successful treatments may still be perceived as disappointing if expectations are emotionally driven rather than clinically grounded.8
Patients experiencing heightened stress, low self esteem or body image dissatisfaction may assign aesthetic treatments an unrealistic role in resolving emotional distress. This disconnect often presents as fixation on residual imperfections or repeated requests for further intervention without clinical indication.10
When a patient is visibly distressed, practitioners can use clear, empathetic language to acknowledge emotions while setting realistic expectations. Examples include:
· “I can see how much this is affecting you, and I want to make sure we approach this safely.”
· “From a clinical perspective your skin is healthy, even though it doesn’t feel that way to you.”
· “More treatment at this stage may not give you the outcome you’re hoping for.”
Managing expectations through a psychodermatological lens helps prevent dissatisfaction driven by stress-related skin responses or emotionally inflated outcome expectations, supporting safer and more predictable treatment outcomes.8
Multidisciplinary care and referral pathways
Psychodermatology supports a collaborative approach. Working with psychologists, counsellors, dermatologists or wellbeing professionals ensures that both emotional and physiological contributors to skin concerns are addressed. Referrals should be presented as an extension of care rather than a failure of treatment.1,4
Patients who receive emotional support alongside aesthetic interventions are more likely to engage realistically with treatment plans, adhere to aftercare and achieve higher satisfaction. Studies show improvements in treatment adherence, satisfaction and quality-of-life scores in up to 30-40% of patients when psychological or structured psychosocial support is integrated into dermatological care.1,4,8,10 Integrated care models have been shown to improve outcomes and reduce dissatisfaction in complex cases.1,4,10
Collaborative models may include parallel psychological support alongside aesthetic treatments, staged care prior to procedural escalation or shared decision-making with dermatology or wellbeing professionals.11 Such approaches improve patient engagement, reduce dissatisfaction and overtreatment and strengthen ethical aesthetic practice.1,4,10
Refusing treatment
Refusing treatment is a necessary clinical skill in aesthetic practice and should be viewed as a professional judgement rather than personal rejection. When aesthetic concerns are primarily driven by psychological distress or distorted self-perception, proceeding with treatment risks reinforcing maladaptive beliefs and worsening long-term outcomes.10,11 In these situations, intervention may offer
temporary reassurance but ultimately increases dependency, dissatisfaction and the likelihood of repeated or escalating requests. Clear, empathetic refusal protects both patient wellbeing and clinical integrity.10 Effective refusal relies on structured, transparent communication. Acknowledging the patient’s distress, explaining the clinical rationale for declining treatment and outlining realistic limitations of aesthetic intervention help preserve trust while preventing harm.
Appropriate signposting to psychological or wellbeing support – such as referral to a clinical psychologist, counsellor or structured talking-therapy service – helps ensure care remains ethical, proportionate and patient-centred, whilst aesthetic intervention is unlikely to address the underlying concern.10
Practitioners can navigate this sensitively using the ‘Validate-Reframe-Redirect’ approach. This approach draws on established principles of therapeutic communication and motivational interviewing commonly used in psychodermatology and cosmetic practice.1,6
1. Validate: Acknowledge the patient‘s feelings – “I can see this this is really affecting your confidence.”
2. Reframe: Gently place the concern in clinical context – “From a clinical perspective your skin looks healthy, but I understand the impact this is having on you.”
3. Redirect: Guide the next step – “It might be helpful to speak with someone who can explore these feelings in more depth. I can recommend someone who specialises in this.”
Recognising psychodermatological influences should inform every stage of aesthetic treatment planning. When emotional stress or psychological vulnerability is identified, practitioners must consider not only technical suitability, but also treatment timing, intensity and likely response. Psychological stress disrupts skin barrier integrity, amplifies inflammatory pathways, and impairs wound healing. As a result, aggressive or high-impact interventions – such as ablative or high-energy laser resurfacing, multiple injectable treatments in one setting and combination protocols – carry a greater risk of prolonged recovery, unpredictable outcomes and patient dissatisfaction.2,3,7,8
In practice, this often necessitates a more conservative, stabilising approach. Treatment planning may prioritise barrier repair, inflammation reduction and gradual regeneration rather than immediate procedural escalation. Energy-based devices, injectables or combination treatments may require modification or temporary postponement when stress-related dysregulation compromises skin resilience.2,3,7
Within a psychodermatological framework, adaptation does not imply avoidance of treatment, but appropriate sequencing and individualisation. For example, reduced energy settings or extended intervals for device-based treatments, conservative dosing and staged plans for injectables and simplified protocols emphasising barrier-supportive and anti-inflammatory strategies.2,3,7
Timing is equally important. Performing elective procedures during periods of acute psychological distress increases the likelihood of exaggerated inflammatory responses, delayed healing and dissatisfaction. Allowing time for emotional stabilisation – commonly four to six weeks, with reassessment of both skin and psychological readiness – can improve biological outcomes and patient experience.2,3,7,8
Aftercare should also be adapted, as psychologically stressed patients often benefit from clearer guidance. This includes simple written instructions, explicit healing timelines, clear advice on what is normal versus concerning, closer follow-up with proactive reassurance and expectation management that acknowledges improvement may be gradual and influenced by both physiological and emotional factors.8
This case study illustrates how psychodermatological principles can be applied to treatment planning to support patient safety, realistic expectations and optimal outcomes.
Case presentation
A patient presents requesting combination aesthetic treatment involving energy based devices and injectable treatments for facial erythema and textural irregularity. During consultation, they disclose significant ongoing stress related to recent bereavement and work pressures, alongside heightened skin sensitivity and prolonged downtime following previous procedures.
Choice of treatment
Given the patient’s disclosure of significant psychological stress and a history of heightened post-procedural reactivity, the treatment plan was modified to prioritise low-impact, barrier-supportive skin therapies, with procedural interventions initially deferred. This approach aimed to stabilise skin function and reduce baseline inflammation before escalation.
Timing
Treatment was staged over an extended timeframe rather than initiated immediately. Initial interventions were followed by reassessment at six- to eight-week intervals, allowing adequate time for inflammatory resolution, assessment of healing response, and evaluation of emotional readiness. Elective high-impact procedures were postponed during the period of acute psychological stress.
Treatment intensity
When procedural treatment was introduced, energy-based device therapies were delivered using conservative settings and limited treatment coverage to minimise inflammatory burden. Only one modality was used per session, avoiding combination protocols. Injectable treatments were introduced four to six weeks later, with conservative dosing in targeted areas and a staged approach rather than full-face correction in a single visit.
Aftercare was enhanced with clear written instructions, simplified skincare routines, and barrier-repair and anti-inflammatory products. Healing timelines were explicitly discussed to reduce anxiety and misinterpretation of normal inflammatory responses. Follow-up was arranged earlier than standard practice, with review at one to two weeks to provide reassurance and enable timely adjustment of the treatment plan based on skin response and patient wellbeing.
Building a clinic culture that integrates psychological awareness with dermatological care ensures consistent, compassionate support. From the first point of contact to clinical treatment, every team member contributes to a sensitive and informed patient experience.1,4
Receptionists, therapists and clinical assistants are often the first to observe early signs of patient distress or dissatisfaction. Providing training in empathetic communication and psychological awareness – through structured induction programmes, regular reflective case discussions and scenario-based communication training focused on recognising emotional distress and appropriate escalation – enables staff to respond effectively and identify vulnerable patients at an early stage. Regular reflective meetings, monthly or quarterly case discussions and empathy workshops held once or twice a year provide structured opportunities for staff development. These sessions may include anonymised review of complex cases, recognition of emotional distress, communication and expectation-management strategies, ethical boundary-setting, support for staff wellbeing and clarification of escalation or referral pathways to ensure consistent, psychologically informed care.
Embedding psychological understanding within the practice not only enhances patient care but also elevates staff morale, positioning the clinic as a leader in ethical and holistic care.1,4
Psychodermatology bridges skin health and emotional wellbeing, offering aesthetic practitioners a framework to optimise treatment outcomes and patient satisfaction. By recognising how emotional states manifest in the skin, adapting treatment planning accordingly and engaging in multidisciplinary care when appropriate, practitioners can deliver safer, ethical and effective outcomes.

Dr Saba Raja is an NHS GP, medical director and founder of aesthetic practices in Norwich and Reading, specialising in non-surgical treatments. She has a particular interest in skin health, mental health and women’s health, and advocates for ethical, psychologically informed aesthetic practice and patient-centred care. Qual: MBBS, MRCGP
Business process and innovations manager Danny Chavda shares how sustainable clinic growth comes from structure, visibility and clarity
What would happen if your clinic bookings doubled overnight?
Many aesthetic clinics experience rapid growth, but the real issue is whether that growth is supported by scalable systems or absorbed by individual effort and informal workarounds.
Sector data reflects this gap. The State of Medical Aesthetics report, which surveyed 160 nurses and doctors, found that only 33% of clinicians felt confident building and managing teams, and just 31% had formal training and development plans in place.1 This points to a wider challenge around operational readiness as clinics grow.
As demand rises and governance expectations tighten, informal ways of working become harder to sustain.2 Regulatory guidance increasingly stresses the need for consistent workflows, clear ownership and robust documentation to support safe, scalable growth – particularly around consent, follow-up and record-keeping.3
This article outlines a practical framework for sustainable clinic growth, using structure, clarity and visibility to enable predictable scaling while protecting patient outcomes and team wellbeing – so growth is supported by systems, not constant intervention.
Structure beats intensity
In aesthetic clinics, intensity can manifest as longer days, squeezed diaries and problems solved through effort rather than process. It relies heavily on individual memory, proximity and the constant availability of senior staff to keep things moving.
Structure, by contrast, is built around defined workflows, clear ownership and agreed standards that guide decisions even when the clinic is busy. Work continues consistently regardless of who is on shift, because the system carries the load rather than the individuals within it.
At scale, effort only masks weakness, whereas structure determines outcomes. Growth becomes chaotic not because demand increases, but because it lands on foundations that were never designed to support it, such as undocumented handovers, unclear follow-up ownership or inconsistent record keeping.
A case study of when growth outpaces structure
When a clinic experiences rapid growth, it quickly becomes apparent whether its underlying structure can support that expansion. This was the case for Clinic A, which doubled its revenue in just two months. The clinic began to experience follow-up appointments slipping through the cracks, as responsibility sat ambiguously between practitioners and the front-of-house team. Treatment notes varied significantly between clinicians, making continuity of care and audit review increasingly difficult. In addition, recurring tasks relied heavily on the owner’s memory, creating unnecessary dependency and slowing decision-making.
To restore stability, the team introduced a simple daily operating structure built around clear ownership, sequencing and escalation. In this case, it took the form of a short daily huddle, but it was the structure rather than the meeting itself that made the difference.
This was supported by a visible workflow board, meaning a shared reference point that made patient status, responsibilities, outstanding tasks and risks explicit for the day.
By strengthening the underlying structure through clear ownership and shared visibility of work, the team stabilised operations. Within four to six weeks, errors reduced, patient journeys became more consistent, communication improved and dependency on the owner decreased, without adding staff, software or longer hours. The clinic did not slow down; it stopped leaking energy, and the structure gave growth somewhere to land.
In your next team meeting, identify one recurring issue that is currently solved by ‘working harder’ (staying late, squeezing patients in, last-minute decisions). Ask what simple process, checklist or handover step would prevent it.
Practitioners should use these prompts in reviews or team meetings:
1. Which tasks rely on memory rather than documented workflow?
2. Where does patient experience feel inconsistent between practitioners?
3. If demand doubled next month, where would strain appear first?
4. Which steps repeatedly require clarification?
5. What could be standardised this week to reduce friction? Where tension appears repeatedly, structure is often missing.
In practice, visibility shows up through simple, shared mechanisms that allow work to be seen at a glance. This might include a follow-up tracker visible to both clinicians and front-of-house, a daily patient flow board, or a standardised handover that confirms what has been completed and what remains outstanding.
When work is visible, teams share the same understanding of what has been done, what remains outstanding and what requires attention. In medical aesthetics, visibility plays a critical role across clinical and operational activity.
Visible consent mechanisms, such as a clearly documented consent status within the patient record or on a daily workflow board, ensure that consent is current, verified and confirmed prior to treatment. Clear visibility of follow-ups and escalation steps, such as a shared tracker showing outstanding reviews, complication checks and who is responsible, supports timely complication management and audit readiness.
When workflows live in personal inboxes, handwritten notes or individual habits, safeguards weaken.5 As information fragments, access becomes limited and routine decisions slow down. A visible workflow removes this ambiguity by creating shared reference points, enabling teams to act with greater confidence and consistency.
A case study of when simple tracking steps prevents follow-up failure
In one medium-sized clinic, follow-up responsibility sat ambiguously between practitioners and front-of-house, leading to missed reviews and delayed complication checks. Introducing a shared follow-up tracker clarified ownership and made follow-up status
visible to the whole team. In practice, this took the form of a simple shared list showing patient name, treatment date, required follow-up window, status and named owner. This can be built in a shared spreadsheet, a simple task board (e.g. Notion, Excel or Microsoft Planner), or a physical board updated daily. Similar visibility can also be achieved through daily patient flow boards, standardised handover checklists or clearly designed status markers showing what has been completed and what remains outstanding. The effectiveness came from shared visibility and ownership, not the sophistication of the tool itself.
Within two weeks, missed follow-ups were reduced, with internal tracking suggesting follow-up completion improved from around 70% to over 95%, without any change to clinical protocols.
Practitioner tip
For the next two weeks, track all follow-ups on a shared list that both clinicians and front-of-house can see, including follow-up status and ownership. At the end, compare follow-up completion rates and administrative chasing with your usual baseline.
Prioritising clarity over ambiguity
In aesthetic clinics, clarity refers to the explicit definition of ownership, sequencing and standards within everyday operations. It means knowing who is responsible for each step of the patient journey, what happens next and what ‘good’ looks like, rather than interpretation, memory or informal agreement. In practice, clarity is created through written role expectations, agreed process standards and regular touchpoints such as briefings or short one-to-ones that reinforce ownership over time.
As patient numbers rise, informal coordination breaks down. Ambiguity becomes costly, showing up as delays, duplicated work, missed follow-ups and increasing reliance on senior staff to resolve routine issues. When responsibility, standards and exceptions are explicit, it protects patient safety, strengthens clinical consistency and improves defensible documentation. It also reduces practitioner uncertainty and supports compliance alignment.4 Ambiguity often hides in small, repeatable tasks such as room turnover. When responsibility for cleaning, restocking, documentation and readiness is assumed rather than owned, delays occur and variation increases. Once ownership is defined, performance typically stabilises without further intervention.
A case study of when clarity stabilises daily operations
In one growing clinic, responsibility for post-treatment queries was unclear. Practitioners assumed front-of-house would triage messages, while the admin team believed clinical staff would respond once available. As volume increased, response times lengthened and patients received inconsistent advice. The clinic introduced a simple clarity step which took the form of a written protocol defining who handled first response, when escalation was required and what documentation was expected. Within two to four weeks, response times became consistent, internal clarification reduced and patient confidence improved. Nothing new was added to the workload. The difference came from making ownership explicit rather than assumed.
Choose one routine task, such as handling post-treatment queries. Write down who owns the first response, what must be documented and when responsibility formally passes to someone else.
A common response to operational strain in clinics is to invest in new tools, whether digital systems or physical platforms, in the
hope they will resolve underlying problems. These may include booking and diary software, consent and documentation systems, patient communication tools, reporting dashboards or treatment devices. However, tools do not fix unclear processes they can only formalise what already exists. If a clinic does not have agreed workflows, defined ownership or consistent standards, a system has no reference point to enforce.
For example, introducing new documentation software will not improve record quality if practitioners are recording consultations differently. The system will store those differences more neatly, but continuity of care, audit readiness and follow-up reliability remain unchanged.
Tools work best when they support clear roles, documented workflows and predictable patient journeys. Without these foundations, clinics risk scaling inconsistency rather than performance. In practice, tools are most effective when introduced after structure is defined, not as a substitute for it.
While the principles of structure, visibility and clarity apply across all clinics, how they are implemented will vary with team size and operational complexity.
In small clinics, typically one to three practitioners working closely together, operations often rely on proximity, informal communication and shared memory. At low volume this can feel efficient, and structure does not need to be complex. In practice, a single shared daily list covering patients, follow-ups and outstanding actions can prevent early strain as demand grows. Medium-sized clinics, often involving multiple practitioners and front-of-house staff across overlapping shifts, reach a transition point where informal systems begin to break down. Responsibilities overlap, communication becomes less immediate and assumptions start to creep in. Introducing a short daily huddle, combined with a standardised handover between front-of-house and clinicians, helps maintain clarity, reduce duplication and prevent missed follow-ups without adding unnecessary workload.
In larger clinics, where teams are spread across multiple rooms, days or locations, scale introduces distance between team members, making informal coordination unreliable. Here, structure must substitute for proximity. This typically means formalising roles such as clinical lead and operations lead, standardising documentation templates, and clearly defining escalation pathways. These measures ensure standards, accountability and patient journeys remain consistent regardless of who is on shift.
Across all clinic sizes, sustainable growth depends less on tool sophistication and more on systems that match operational complexity.
Clinics scale through predictability. Sustainable growth emerges from visible workflows, clear ownership, repeatable patient journeys and consistent documentation. When these foundations are in place, practitioners can focus on clinical excellence rather than operational firefighting. Long before a clinic grows, its systems determine whether that growth creates stability or strain.

Danny Chavda is the business process and innovations manager at Church Pharmacy, where he designs and implements operational systems that support safe, scalable growth in regulated healthcare environments. His work focuses on workflow clarity, visibility and governance, helping multidisciplinary teams move from reactive intensity to predictable, resilient operations.




SEO specialist Jane Nriapia discusses how AI-written content could be undermining practitioners’ online success
To meet growing content demands, many clinics and marketing agencies have turned to AI tools such as ChatGPT to generate website copy and blog articles. While this approach offers speed and efficiency, it carries hidden risks, particularly in medical aesthetics.
Medical Aesthetic is classified by Google as Your Money or Your Life (YMYL) content, covering topics that can directly influence a person’s health, safety or financial wellbeing.¹
As a result, Google applies significantly higher standards of quality, accuracy and trust to websites operating in this space. Content must demonstrate strong Experience, Expertise, Authoritativeness and Trustworthiness (E-E-A-T) to perform well in search and to earn patient confidence.² Failing to meet these standards can harm visibility, damage credibility and erode patient trust.
In March 2024, Google rolled out a core algorithm update known as the Helpful Content Update (HCU), designed to promote content created primarily for users rather than search engines.³ Although Google has not confirmed that the update specifically targeted AI-generated content, it did deprioritise low-quality, generic or unhelpful content.4 These characteristics are commonly associated with AI-written content published without editorial review, clinical oversight or medical input.
Following the update, many website owners, particularly those operating content-driven or ad-supported models, reported steep declines in rankings and organic traffic.⁴ Search engine optimisation (SEO) analysts noted that the volatility was significant enough to disrupt visibility for smaller publishers, with some sites publicly documenting difficulties in maintaining prior traffic and monetisation levels.⁴
Specialty observers emphasised that Google positioned the update to reward first-hand expertise, original analysis and people-first content.⁴
For aesthetic clinics, the implication is clear: websites must align with Google’s evolving definition of helpful, trustworthy content. Anything less risks reduced visibility or digital irrelevance.
E-E-A-T is a framework used by Google’s search quality raters to evaluate content quality.² While it is not a direct ranking factor, it plays an important role in shaping how Google’s algorithms identify reliable information, particularly within health-related topics.
For aesthetic clinics, E-E-A-T applies across all patient-facing pages, not just blogs. Articles and educational content should be written or medically reviewed by individuals with first-hand experience of aesthetic treatments. Credentials should be clearly demonstrated through visible authorship, professional titles, regulatory registrations and references to clinical experience – particularly when discussing outcomes, limitations and patient suitability.
On treatment pages, E-E-A-T is demonstrated through accurate descriptions of indications, contraindications, risks and realistic outcomes. Consultation pages should clearly outline assessment processes, informed consent and suitability criteria. For before-and-after imagery, trust is reinforced through consistent photographic technique, appropriate disclaimers and brief contextual explanations.
Clear, medically accurate content is essential. Poor-quality or misleading information can contribute to patient
misinterpretation, inappropriate self-referral and unrealistic expectations, potentially undermining informed consent and patient safety.
Authority is further supported through practitioner biographies, professional affiliations and transparent clinic information. Trust is reinforced through clear contact details, privacy policies and ethical disclaimers. One practical measure is the consistent use of authorship and medical review statements, such as “Reviewed by Dr [Name], GMC-registered aesthetic practitioner”.
YMYL explained
Google’s YMYL classification applies to content that could impact a person’s health, finances or safety.¹ Because aesthetic treatments fall within this category, clinic websites are subject to heightened scrutiny. Content relating to procedures, prescription skincare or treatment outcomes must be carefully written and rigorously fact-checked. Vague claims, inaccuracies and thin AI-generated copy are not only ineffective from an SEO perspective, but also pose clinical and ethical risks, such as patients misinterpreting treatment suitability or downplaying potential risks. Poorly constructed content may lead to patient misunderstanding, unrealistic expectations or incorrect assumptions about suitability. From a search perspective, Google has become increasingly capable of identifying low-value content. Updates such as the HCU have increased the likelihood that pages lacking originality or expertise will lose visibility.³ Google has also confirmed that indexed pages are not guaranteed to remain indexed indefinitely, and unhelpful pages may be removed from search results entirely.⁵
For clinics, this reinforces a shift from content volume to content quality. Fewer, well-researched articles that are medically accurate and human-reviewed are more effective than publishing at scale. Strategic content planning, supported by clinical oversight, is now essential.
Why search is changing and what this means for aesthetic clinics
AI Overviews represent an early stage of Google’s shift towards a more predictive, answer-led search experience. With the introduction of AI Mode, Google has embedded conversational interfaces into everyday search behaviour.⁶ This marks a move away from the traditional model of ten blue links towards an environment where discovery increasingly occurs within search itself.
For medical aesthetics, this affects how patients discover treatments and clinics. Users researching skin concerns or injectables are increasingly presented with summarised guidance and clinic references within search results. Local competition now extends beyond rankings to include which clinics are surfaced or cited within AI-generated answers.
As users engage more with AI-generated responses, visibility depends not only on rankings, but on how clearly content can be interpreted, trusted and selected by AI systems. Specialty data indicates that organic click-through rates have declined since the rollout of AI Overviews, reflecting a growing tendency for users to obtain answers without visiting websites.⁷
For clinics, this has commercial implications. Reduced click-through rates to clinic websites can limit opportunities to convert visibility into enquiries or consultations, particularly where informational queries are resolved within search. Clinics referenced within AI-driven results may influence patient decisions earlier in the journey, shaping perceptions of expertise and trust.
Practical SEO action checklist for aesthetic clinics
Review all treatment and consultation pages to ensure content is medically accurate, clearly attributed and aligned with current clinical practice.
Make authorship and medical review explicit across blogs and educational content, particularly where treatment outcomes, risks or suitability are discussed. Audit existing content using tools such as Google Analytics 4 (GA4) to identify underperforming pages that may be outdated, vague or no longer meeting quality, regulatory or patient safety standards.
Prioritise content that reflects patient decision-making, including suitability, safety and consultation-focused queries, rather than broad informational topics.
Ensure treatment and location pages are structured with clear headings, FAQs and internal links to support navigation and topical authority.
Use schema markup where appropriate to help search engines interpret page content and support enhanced visibility in rich results and AI-driven features.
Monitor performance regularly using tools such as Google Search Console to identify stagnating or declining content.
Confirm that all published content complies with Advertising Standards Authority (ASA) and Committee of Advertising Practice (CAP) advertising guidance, particularly in relation to claims, outcomes and prescription-only medicines.10
Focus on consistency, accuracy and usefulness rather than publishing content at scale.
This shift demands a rethink of content strategy. Rather than focusing on broad educational topics that AI Overviews often answer directly, clinics should prioritise content reflecting real patient decision-making. Queries such as “Am I suitable for tear trough filler for dark circles?” or “Are polynucleotide treatments safe for melasma?” mirror consultation discussions and are less likely to be fully resolved by AI summaries.
AI Overviews remain less prevalent in local and transactional searches. Patients actively searching for services continue to rely on local organic results, Google Business Profiles and treatment-specific pages. These searches often translate into website visits and subsequent appointment enquiries
To remain visible, clinics should optimise treatment and location pages with commercial intent. They should also create decision-focused FAQs, structure content clearly using headings and schema markup, a form of structured data that helps search engines better interpret page content, and build logical internal links between related pages to support navigation and topical authority.
In response to these changes, many SEO professionals are broadening their approach to visibility as search behaviour fragments across platforms. Increasing emphasis is placed on understanding how users engage with content across multiple touchpoints. Research suggests that brand recognition, trust and consistent visibility are becoming increasingly important as search evolves.⁸
SEO is therefore evolving into a more holistic digital strategy in which search visibility is influenced not only by on-page optimisation, but by broader brand signals, reputation, content quality and user engagement across multiple platforms. Clinics with recognisable names, credible expertise and well-structured content are more likely to earn trust and selection within both traditional search results and AI-generated features.⁹
practices for clinics using AI for content
AI can support marketing activity when used appropriately, particularly for idea generation and content structuring. However, any content representing a medical aesthetics clinic must be reviewed by a human editor with appropriate medical knowledge. Clinics must also ensure all content complies with UK advertising regulation. The ASA and CAP impose clear restrictions on what can be promoted, including prescription-only medicines, exaggerated claims and misleading outcome statements.10 AI-generated content increases the risk of inadvertent breaches if not carefully reviewed.
Human expertise remains essential, even for small teams or independent practitioners. Practical safeguards include documented sign-off processes, clear authorship and review statements, and periodic content audits (for example every three to six months) rather than publishing at scale.
Google Search Console can be used to monitor content performance over time, including impressions, clicks and changes in visibility. Declining or stagnant performance may indicate that content is not meeting quality expectations.11
Ultimately, Google aims to surface reliable, accurate information. Clinics prioritising patient education, clinical accuracy and editorial oversight are more likely to perform sustainably.
SEO in its entirety
In a specialty where trust and safety are paramount, online content should be treated with the same professionalism as patient care. AI can support content creation, but it should not replace clinical judgement or ethical responsibility.
By aligning content with Google’s quality guidelines, complying with advertising regulation and embedding E-E-A-T consistently across their website, clinics can protect their visibility, build authority and earn patient trust in an increasingly competitive, AI-driven search landscape.

Jane Nriapia is the founder of BoutiqueSEO, a Leeds-based agency specialising in SEO for medical aesthetics. With 16 years in digital marketing and hands-on experience in clinics and training academies, she helps clinics grow through ethical, strategic and patient-focused SEO.

Dr Glyn Estebanez shares a day in his life in clinic alongside his work with Allergan Aesthetics, an AbbVie company
A typical working day…
My day usually begins at the gym just after 6am. I am very fortunate and have a gym in my building, which makes my life a lot easier and means I have no excuses for not going. I enjoy callisthenics as I was an international gymnast until I was 21, although I’m no longer as flexible as I once was. I usually train for about an hour before heading back upstairs for a light breakfast, typically consisting of yoghurt with fruit and cereal or a protein shake. As a coffee lover, I always make myself a cortado before heading out the door at 8:15am.
My clinics, Dr Glyn Medispa, are located in both Chester, Cheshire and Fitzrovia, London and my daily commute to the London clinic consists of a short tube journey from White City.
I find that I work best in the mornings, so after arriving at around 9am, I start my day with a full team meeting. This allows my team to brief me on high-profile patients that we will be treating that day, as well as any updates or announcements. I like to prioritise scheduling any major appointments in the morning, so I usually block out enough time for four patients to be seen.
The majority of my patients come to me for facial harmonisation, which usually involves a carefully planned, combination approach rather than isolated treatments. This includes neuromodulators to adjust muscle activity, alongside hyaluronic acid injectables to restore structure and provide support where it has been lost. In addition to this, all patients are assessed by my team and expert colleagues to ensure skin quality is also addressed and improved alongside structural and muscular balance. This integrated approach allows for results that are subtle, progressive and well balanced. The basis of facial harmonisation is that no single change should stand out. I often explain to patients that you should never be able to ‘see’ my work – you should simply look at someone and think they look great, without being able to pinpoint why.
My appointments usually take me right up to lunchtime. My go-to is either sushi, Farmer J or Maui Poke – something healthy and not too heavy.
After lunch, I usually have press meetings, which can take the form of strategy meetings. I also occasionally carry out consultations or follow-up reviews for straightforward cases in the afternoon

too. This usually takes me until 5pm, and if I have time, I like to make some social media content. I’m currently creating a new YouTube series called the Harmonisation Series, which follows six patients with diverse needs undergoing combination treatments. One of the patients featured in the Harmonisation Series presented with a significant structural imbalance of the lower face, alongside skin concerns related to previous acne. Rather than focusing on a single area or treatment, her plan followed a multi-modal approach, addressing muscle dynamics, restoring structural support and improving skin quality. By looking at the face as a whole, this allowed for a more natural and integrated outcome, rather than changes that draw attention to one specific area.
After work, I usually meet friends or loved ones for dinner, and I particularly enjoy sushi restaurants such as Roka, or Lebanese cuisine.
On most clinic days, I’ll usually get home between 7-8pm and my evenings are generally quiet. I like to decompress from the day and do something that allows my brain to switch off – whether that’s reading, watching a documentary or a film.
In regard to products I love to use in clinic, I’m a huge fan of HArmonyCa for biostimulation. It’s the product my patients talk about the most. My favourite area to treat is the lower face, particularly the chin, as in my experience, the chin is one of the most poorly treated areas within our specialty. It often completes the face, but it’s far more complex than many practitioners realise. As a result, it’s common to see patients whose previous treatments don’t quite work in harmony with the chin, and sometimes it feels like the chin was just added on, rather than fully integrated into the face.
work commitments...
Outside of my clinical work, I’m an ambassador for Allergan Aesthetics, an AbbVie company and a faculty member at the Allergan Medical Institute. Education is something I’m very passionate about, so I really enjoy being involved in the Allergan Aesthetics training programmes and attending events.
At the Aesthetics Conference and Exhibition (ACE) 2025, I delivered several talks and chaired sessions on behalf of the company. These included sessions on recognising and preserving patient individuality, my approach to facial harmonisation and chairing discussions around complications management.
I’m also involved in the Allergan Aesthetics PR activities and often treat VIP patients on the company’s behalf. Recently, I have also been working with their international team on products that Allergan Aesthetics will be launching over the next few years, which is really interesting and great to be a part of.
One of the most memorable days in my career was being hand-picked as one of five doctors in the UK to be mentored by aesthetic practitioner Dr Maurício de Maio, the pioneer of modern facial aesthetics and founder of the MD Codes. It was an incredibly intense day of full-face injecting under his direct scrutiny, surrounded by peers and a full camera crew.
This experience was deeply grounding, hugely rewarding and transformative for my practice. I remain very grateful to Allergan Aesthetics for inviting me to be part of it, and it stands out as one of the defining moments of my aesthetics career.
Dr Glyn Estebanez will be a mentor at ACE 2026 on March 13. Turn to p.20 to register free now.
If you could choose a career outside the medical field, what would it be?
I think I would have become a teacher. Do you have a mantra that you stick to?
Life is too short to do something that you are not passionate about! Where is your dream holiday destination?
I’d love to be able to go to the Seychelles and have a private villa on the water.
Visual assessment tools such as mirrors and clinical photography are integral to aesthetic consultations. They are used to enhance objectivity, create shared understanding and support informed consent.1 However, research suggests that visual tools are not psychologically neutral. Mirrors and photographs activate distinct psychological states that influence self-perception, emotional response and aesthetic decision making.1
As patients become more conditioned by selfies, filters and image-based social comparison, understanding how visual tools shape perception is increasingly important as they may affect patient satisfaction and mental state. 2
Mirrors provide a dynamic and familiar representation of the self. Most individuals see their face primarily through mirror exposure rather than photographs, leading to strong familiarity with their mirror-reversed appearance. This familiarity forms the basis of the mere-exposure effect, which suggests that repeated exposure increases preference and perceived attractiveness. 3
The duration of mirror exposure is clinically significant. Brief mirror (around 25 seconds) use allows patients to orient themselves and express concerns naturally. Prolonged mirror use (around 10 minutes), especially of the face, significantly increases negative emotional responses particularly in those with appearance related vulnerability – leading to heightened distress, self-criticism and perceptual distortion.4
Full length mirrors appear to encourage a more holistic psychological state by allowing patients to see themselves as a whole rather than isolating facial features.5 Full length mirrors reduce hyper focus on minor asymmetries and support a more integrated sense of self. This is relevant in consultations where facial treatments risk being psychologically decontextualised from the whole person.
Clinical photographs provide a different psychological function. They are static, highly detailed and unfamiliar, reversing facial orientation and removing movement. It has been shown that patients often prefer mirror-reversed images of themselves and experience discomfort when viewing true photographic representations.6 Photographs activate a more analytical and detached psychological state.7 Therefore, when reviewing photographs patients may develop new concerns that were not present prior to imaging, initiating a cycle of increased self-focussed attention, perceptual distortion and psychological distress.
I believe this presents a concern for aesthetic consultations. Aesthetic patients are already highly visually literate due to their use of image centric platforms such as Instagram, TikTok and Snapchat, meaning consultations now occur within a culture of constant self-observation, idealised facial norms and filtered representations of beauty.
Without psychological awareness, the use of mirrors and photography risks reinforcing appearance anxiety, encouraging over treatment and reducing patient confidence. Dissatisfaction due to perceptual mismatch rather than clinical outcome can lead to complaints and revision requests. Therefore, I believe understanding how visual tools influence psychological states allows clinicians to better manage expectations, improve satisfaction and practice ethically.
It can be argued that mirror and photographs improve objectivity, transparency and informed consent. Of course, this argument has merit, as clinical photography is essential for documentation, outcome assessment and medico-legal protection, while mirrors enable shared observation.
However, psychological research demonstrates that increased visual exposure does not necessarily improve understanding. Without context, visual detail may distort perception rather than clarify it.1,2 Objectivity in aesthetic consultations is not achieved through exposure alone, but through guided interpretation.
In light of the above, I believe clinicians should use mirrors and photographs intentionally. This means recognising that visual tools are active psychological interventions, not just neutral aids. How and when they are used should be consciously planned, not left to habit or clinic routine. The choice of tool, timing, framing and duration of use should be as deliberate as the choice of product or technique.
Therefore, principles be adopted in consultations include:
· Explaining that mirrors and photographs present different representations and may feel unfamiliar3
· Limiting prolonged mirror or photo scrutiny to reduce fixation
· Using full length mirrors where possible
· Beginning with conversation and mirror-based exploration before introducing photographs
· Guiding interpretation by normalising asymmetry and using neutral anatomical language rather than aesthetic judgement By guiding perception rather than merely presenting images, I believe clinicians can support informed decision making without reinforcing insecurity. When patients show significant psychological distress at consultation, appropriate referral for psychological support is indicated to safeguard patient wellbeing and to provide ethical care.
Mirrors and photographs are powerful psychological tools in aesthetic consultations. The type of visual tool used, the duration of exposure and the context in which it is introduced can significantly influence patient perception.
By using visual tools thoughtfully and intentionally clinicians can enhance trust, manage expectations and support clinical outcomes that respect both aesthetic goals and psychological wellbeing.

Dr Arti Singh is a dentist and medical injector based at her clinic New Ash Green Dental & Aesthetics. She also works across Skin Doctors & Skin Matters clinics, with a special interest in advanced injectable treatment.
Qual: BDS, MJDF
Your guide to the unmissable companies at the Aesthetics Conference & Exhibition (ACE)
Key Sponsors
A Awards Finalist
Platinum Brands
3D Aesthetics
4T Medical
Acclaro Corporation
Ace Medicine Ltd
A ACRE
Aesthetic Medical Partnership Ltd
A AestheticSource
Aesthetic Web
A Allergan Aesthetics
A ALLSKIN | MED
A Alma
Amory London Ltd
Arthrex Ltd
Beautology Laser & IPL Services Ltd
CHAEUM PHARMA
BEAUTYEUROPE.EU CO UK Ltd
A BTL Aesthetics
CACI International
A Candela (U.K.) Ltd
Cellap Laboratory UK
Cellcosmet
CellPRP
A Church Pharmacy
Cosmeditech Limited
A Cosmetic Courses
Croma Pharma UK
A Crown Aesthetics
Cutera
A Dermafocus Ltd
A Dermapenworld
Elenzia Limited

EMA Aesthetics Ltd
A Energist Ltd
A Evolus
Fotona UK
A Galderma (UK) Ltd
Genefill UK
Halo IV
Harley Academy
A Harpar Grace International Ltd
Hawksley & Sons
A Healthxchange
Hydrafacial
HYPO21
IBSA UK
SR Biotek
iiaa
A InMode / Cure Medical
Inspire to Outstand
Interface Aesthetics
IVANMED
John Bannon Pharmacy
K-Laser UK
A Klira Pro
Laboratoires Fillmed
LPG Systems UK
Lynton Lasers Ltd
Med-Fx UK
Merz Aesthetics
Nata Training Academy
Neauvia
Novus Medical UK

Opatra
Pabau
PRP PURE LTD
PT DERMIS LABS SOFTWARE
Pure Tone Aesthetics
Quad Aesthetics
REGEN LAB SA
Revolve Medicare
RS Risk Solutions Ltd
S.THEPHARM CO.,LTD.
Sciton UK
A Sculpt Pro Aesthetics
Seriderm UK & Ireland
Shire Leasing PLC
Silhouette Dermalift
skinade
A SkinCeuticals
Smart Group
A SOFWAVE
SOOVIA CARE Ltd.
Spring Thread UK
Teleta
A The Glow Group
A Totally Derma
TSK Laboratory UK
Vivacy Laboratories UK
A WIGMORE MEDICAL LIMITED
You Can Clinic Ltd.
A Zenoti
Zero Gravity Skin
A ZO Skin Health


Introducing the NEW BELOTERO Syringe. Now available for BELOTERO Balance, Intense and Soft. Created to enhance your BELOTERO experience, it features an improved design for optimised precision during injection, while retaining our trusted formula.









Non-detachable rubberised finger and thumb grip.

Colour coding for intuitive ease.


Integrated Luer-Lock for secure needle attachment.
Automated production with tamper-evident and anti-counterfeit safeguards for improved authentication and streamlined handling.




Premium Jewel
Box Design


Enhances brand experience, aids product identification.










Adverse events should be reported. Reporting forms and information for United Kingdom can be found at https://yellowcard.mhra.gov.uk. Reporting forms and information for Republic of Ireland can be found at: https://www.hpra.ie/homepage/about-us/report-an-issue. Adverse events should also be reported to Merz Aesthetics UK Ltd by emailing UKdrugsafety@merz.com or calling +44 (0) 333 200 4143. © 2026 Merz Aesthetics UK Ltd – All rights reserved. MERZ AESTHETICS and the BELOTERO logos are trademarks and/or registered trademarks of Merz Aesthetics UK Ltd in the United Kingdom. Registered in England No. 14506945. Merz Aesthetics UK Ltd, Ground Floor Suite B, Breakspear Park, Breakspear Way, Hemel Hempstead, Hertfordshire HP2 4TZ. www.merz-aesthetics.co.uk M-BEL-UKI-2038 Date of Preparation January 2026 All BELOTERO products referred to in this infographic contain lidocaine, as BELOTERO without lidocaine has been discontinued, with the exception of BELOTERO Revive designed without lidocaine. For your information, BELOTERO lidocaine and non-lidocaine share the same product specifications with the key di erence being the inclusion (or absence) of lidocaine.


Scan the QR code to speak to an Account Manager for more information