COMMON SENSE
TM

TM
Officers
President
Robert Frolichstein, MD FAAEM
President-Elect
Vicki Norton, MD FAAEM
Secretary-Treasurer
Phillip A. Dixon, MD MBA MPH FAAEM CHCQMPHYADV
Immediate Past President
Jonathan S. Jones, MD FAAEM Board of Directors
Heidi Best, MD FAAEM
Laura J. Bontempo, MD MEd FAAEM
Eric Brader, MD FAAEM
Kimberly M. Brown, MD MPH FAAEM
Frank L. Christopher, MD FAAEM
Fred E. Kency, Jr., MD FAAEM
Robert P. Lam, MD FAAEM
Kevin C. Reed, MD FAAEM
Robert E. Suter, DO MHA FAAEM
YPS Director
Haig Aintablian, MD FAAEM
AAEM/RSA President
Katy Wyszynski, DO MS
CEO, AAEM-PG
Ex-Officio Board Member
Mark Reiter, MD MBA MAAEM FAAEM
Executive Director
Tamara Wagester, CAE
Executive Director Emeritus
Kay Whalen, MBA CAE
Common Sense Editors
Edwin Leap II, MD FAAEM, Editor
Yash Chavda, DO MBA FPD-AEMUS FAAEM, Assistant Editor
Mel Ebeling, MD, Resident Editor
Stephanie Burmeister, MLIS, Managing Editor
Articles appearing in Common Sense are intended for the individual use of AAEM members. Opinions expressed are those of the authors and do not necessarily represent the official views of AAEM or AAEM/RSA. Articles may not be duplicated or distributed without the explicit permission of AAEM. Permission is granted in some instances in the interest of public education. Requests for reprints should be directed to AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202, Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
Mission Statement
AAEM fights for high-quality patient care delivered by board-certified emergency physicians and champions a fair and equitable workplace for emergency physicians through advocacy and education.
Vision Statement
We aspire to and champion a future in which:
1. The integrity of the doctor-patient relationship is upheld by emergency physicians with full control over their own practices, free of outside interference.
2. Every individual, regardless of race, ethnicity, sexual identity or orientation, religion, age, socioeconomic or immigration status, or physical or mental disability has unencumbered access to high-quality emergency care.
3. Emergency medicine is solely practiced by physicians who are board-certified or board-eligible through either the American Board of Emergency Medicine (ABEM) or the American Osteopathic Board of Emergency Medicine (AOBEM).
4. Every emergency physician’s personal and professional well-being is supported through fair and equitable practice environments and due process.
5. Residency programs and graduate medical education are free from harassment and discrimination.
6. The Academy continues to provide its members with high-quality, cutting-edge emergency medicine education.
7. The Academy supports the establishment and recognition of emergency medicine globally as an independent specialty.
Membership Information
Fellow and Full Voting Member (FAAEM): $595* (Must be ABEM or AOBEM certified, or have recertified for 25 years or more in EM or Pediatric EM)
Associate: $195 (Limited to graduates of an ACGME or AOA approved emergency medicine program within their first year out of residency) or $295 (Limited to graduates of an ACGME or AOA approved emergency medicine program more than one year out of residency)
Fellow-in-Training Member: $95 (Must be graduates of an ACGME or AOA approved emergency medicine program and be enrolled in a fellowship)
Emeritus Member: $295 (Please visit www.aaem.org for special eligibility criteria)
International Member: $195 (Non-voting status)
Resident Member: $80 (voting in AAEM/RSA elections only)
Transitional Member: $60 (voting in AAEM/RSA elections only)
International Resident Member: $80 (voting in AAEM/RSA elections only)
Student Member: $40 (voting in AAEM/RSA elections only)
International Student Member: $30 (voting in AAEM/RSA elections only)
Pay dues online at www.aaem.org or send check or money order to: AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org

President’s Message: Value =
24
Balancing Residency and New Parenthood
states, “Hospitals must make money to stay in business.” But, how do they make this money?
valuable. We just need to recognize it ourselves
In 2026, the American Board of Emergency Medicine (ABEM) will introduce a new certifying exam, replacing the long-standing oral board exam. These changes aim to create a fair, more comprehensive evaluation that aligns with real-world clinical practice. With the shift to a new format, many candidates and educators are eager to understand the rationale behind these updates and what they mean for the future of our specialty. To explore the motivations driving these changes, the impact on candidates, and how the new exam aims to ensure fairness, accessibility, and relevance, Dr. Mary Unanyan sat down with the President of ABEM Dr. Diane Gorgas for an in-depth discussion on the future of certification in emergency medicine.
15
of the Competent Emergency Physician in Media: How “The Pitt” Rewrites the Narrative


When millions of viewers see an emergency team leading resuscitations, managing traumas, nailing airways, performing nerve blocks, having hard goals-of-care discussions, or quietly regrouping after a loss, does the perception of the emergency physician evolve? Dr. Chavda explores the perception of emergency physicians and how the hit show “The Pitt” has helped change that.

While interventions to improve emergency care have historically focused on clinical outcomes, mounting evidence suggests that addressing the perception of care—specifically, perceived wait times—may hold untapped potential for improving patient satisfaction without major systemic overhaul. The waiting room should not be viewed as separate from care. It is the beginning of the patient journey, argue the authors.
When Dr. Kristen Hancock found out she was pregnant during residency, she knew it would be challenging but, she’s not the only one. More and more residents are choosing to start families during training. And while the challenges are real, the support systems we build within our programs, departments, and among each other can make all the difference.
26
Young Physicians Section: Avoiding Burnout Through Career Diversification

With over half of the emergency medicine physician workforce experiencing burnout, as early career attendings, it is imperative that we invest early in our ourselves to ensure we maintain the job satisfaction that allows for career longevity. Dr. Jack Allan admits this investment starts as more work but it grows into a diversification of job roles which will protect you from burnout in the long run.
Robert Frolichstein, MD FAAEM

As I write this message, I have been home from the Mediterranean Emergency Medicine Conference (MEMC) for about two weeks. It was a great experience talking to other emergency physicians throughout the world and learning from them. There are many things that are done differently and many that are the same. I am not really talking about the clinical stuff but more the process and environment in which emergency medicine is practiced. One thing that struck me is that emergency physicians throughout the world share a common bond. We devote our careers and a good portion of our lives to the belief that we are obliged to do what is best for our patients. That means we sacrifice. We sacrifice our time and effort with our own education and teaching others. We sacrifice special, sacred time with those we love so that we can care for our patients on weekends and holidays. We sacrifice in so many ways—for the good of our patients. This bond we share is strong, and we need to acknowledge it and lean on it. The strength of this bond will allow us to arise above our differences, whether those differences be cultural, racial, socioeconomic, or geopolitical.
One of my duties during the conference was to give an update on the state of EM in the USA during an International EM track where numerous
emergency physicians from around the world informed the audience of the state of EM in their country. It was a great track and fascinating to hear some of the same struggles our specialty went through in the early days—are you really more than a triage doctor? Can I trust what you do/ say? The hospital won’t really support us, etc. Ultimately, it was very encouraging as I saw that our specialty has blossomed in many parts of the world into the essential, incredibly valuable specialty that it is.
I have been a physician and emergency physician for a long time. I am a PGY 33. I have seen a lot of changes in EM over the years, and I have never been more proud of our specialty.
Let me tell you why. I will approach this from a business perspective more than a clinical perspective, as that has been the focus of most of my career. The value equation as it applies to healthcare has been defined differently. I like the following:
Value = Quality (think outcomes and capability) + Service (think patients treated and their experience) Cost
[A]dmissions accounts for a large percentage of their total revenue. We drive that revenue. We are therefore obviously valuable to the hospital balance sheet…Precisely because we are valuable, we are being exploited and manipulated.”
There is a lot of work to do against one of the strongest adversaries ever—greed. Fight or submit?”
We are incredibly valuable to our system. Let’s look at a single hospital. More than half, sometimes more than 75%, of admissions come through the ED. Hospitals must make money to stay in business. The way they make money is from admitted patients. Ultimately, a lot of their revenue is from surgeries and other procedures, but admissions accounts for a large percentage of their total revenue. We drive that revenue. We are therefore obviously valuable to the hospital balance sheet. Our value does not stop there. Perhaps even more valuable but harder to calculate is the value we provide by being excellent physicians. Our patients are increasingly complex. There were a lot of babies born in the US in the late 40s, 50s, and 60s. Those people are now 60-80 years old. Obviously, an aged population will be more medically complex, but add to that many patients are surviving illnesses and injuries that would have claimed their life even a few decades ago. It is common for us to treat patients with multiple serious, now chronic diagnoses. They arrive with acute exacerbations of their chronic illness or an acute illness or injury complicated by their chronic disease. These are tough, clinically challenging patients. As a specialty, we have embraced this complexity. We have honed our skills and provide expertise to accurately diagnose and begin treatment for these patients. That saves lives. That shortens the length of stay in the hospital, which allows more and more patients to be admitted. We are incredibly valuable. That is great, and we love it. That should make us proud.
At the same time as I am proud of my specialty, as I look to the future, it is with some trepidation. Precisely because we are valuable, we are being exploited and manipulated. That value is recognized by insurance companies (denominator), hospitals (numerator, sometimes denominator), physician employment companies, or contract management companies (both numerator and denominator). The results of this situation are that there are too many emergency medicine residency programs, more physicians than ever are in employment models that give them little or no control over their practice, and burnout is at record high levels and threatens the longevity of our careers.
In the last 10 years or so, a lot of new EM programs have been established. Why is this happening? Imagine if you are a large hospital system in the US. You recognize the value of emergency physicians and emergency departments and want to continue to benefit from the physician and departments with minimal investment. The valuable commodity is the emergency physician. You want to make sure there is always an adequate supply of these physicians, and you want to control them—start making them. If there are too many? That’s okay it drives down cost.
The same reasoning explains the explosion of emergency physicians that find themselves in employment scenarios that provide them with little control over their practice. Those that employ emergency physicians don’t acknowledge their value (hide the collection data) and make it hard for them to leave (non-competes).
Every study or survey about burnout in recent years that I have seen shows EM at or near the top. It is very concerning, and I believe it will shorten the career of the average emergency physician. This is obviously bad for that individual but also our specialty. We are losing physicians and their expertise at the peak of their careers.
There is hope. AAEM has been fighting to expose the harmful effects of corporatization for decades. People are starting to listen. The media and the legislature are interested in our story. We are an executive producer in an upcoming documentary, Suck it up Buttercup, that dramatically tells the story of the harmful effects of corporatization on physicians and, importantly, patients. There is a lot of work to do against one of the strongest adversaries ever—greed. Fight or submit?
Ultimately, I think we will be fine because we are so valuable. We just need to recognize it ourselves and demand to be recognized for the value we bring. That won’t help you on your next shift. It will help if you understand that you are valuable. That you are an expert. You save and positively impact lives every day. Cherish that and lean on it. That is valuable in something bigger than corporate medicine. This world is better because of what you do.
Yash Chavda, DO MBA FPD-AEMUS

This September, “The Pitt” took home the Primetime Emmy for Outstanding Drama Series. Noah Wyle earned his first Emmy after multiple nominations, winning Outstanding Lead Actor. Katherine LaNasa joined him, taking home Supporting Actress. Thirteen nominations total: writing, directing, acting, technical. Something struck a nerve—not just with critics, but with anyone who’s ever watched a medical show and thought, that’s probably not how it really is…
For emergency physicians, this one feels different. It’s the first time in a long while that a series has said, clearly and without apology: we are not supporting characters. We have our own powerful stories.
For decades—aside from the original “ER”— our specialty has commonly been flattened into a trope: the harried hallway doc, sprinting from curtain to curtain, stabilizing long enough for “the real doctors” to take over. “Grey’s Anatomy” centered the surgeons. “House” rolled its eyes at every specialty, but especially us. Those portrayals stuck in popular culture and, honestly, in a few hospital hallways too.
“The Pitt” takes that shallow stereotype and quietly buries it. Set in a gritty, high-acuity urban hospital, the show lets emergency physicians anchor the story. Its characters make difficult diagnoses, perform critical procedures, and manage complex patients from undifferentiation to disposition.
One storyline features the team diagnosing and draining a pericardial effusion with tamponade under ultrasound guidance before consultants
The push-and-pull between specialties becomes commentary on how medicine actually happens: fast, imperfect, and interdependent.”

even arrive. Another shows emergency physicians using ultrasound-guided nerve blocks for fractures. Yet another captures the rapid recognition of a retrobulbar hematoma and immediate decompression without waiting for ophthalmology—something real-world evidence tells us can save vision. Scenes like these remind viewers that emergency medicine is deep, decisive, and capable.
Yes, there’s friction with consultants. Always will be.
One case in “The Pitt” stood out: a patient with blunt chest-wall trauma, possible rib fractures. On bedside ultrasound, the intern reported no obvious hemopneumothorax. A surgeon cracked a grin: “We trust the CT more than your ultrasound skills.” The surgery resident wants to give opiates for pain meds, but the EM senior performs a serratus-anterior block for pain relief. Later, the CT shows a tiny pneumothorax. As the patient’s oxygenation worsens, the intern—thinking it’s lung contusions—starts BiPAP without looping in the senior, converting a small pneumo into a tension. The aggravated senior rushes in, decompresses, places a pigtail.
In “The Pitt”, that sequence doesn’t feel engineered for drama—it feels possible. Errors can happen, nobody bats a 1000, especially in training, but must be used as measures for improvement, not punishment. It captures what it means to practice in a world where decisions must come before consensus, before backup, before the data set is perfect.
The show doesn’t frame that urgency as arrogance; it frames it as necessity. Because that’s what it is. Waiting is a luxury we don’t always have.
Older dramas used consultant clashes for spectacle—raised voices and slammed doors. Here, the moments feel truer, the banter realistic. The push-and-pull between specialties becomes commentary on how medicine actually happens: fast, imperfect, and interdependent.
One of “The Pitt”’s most striking qualities is how it allows its doctors to be both skilled and scarred.
Television medicine often drew a hard line: if an ER doc was emotional, they couldn’t also be competent. If they cared too deeply, it clouded their judgment. This show rejects that. Its
physicians carry fatigue, grief, and self-doubt— but those emotions coexist with authority and expertise. They don’t diminish it; they deepen it. Every emergency physician knows that feeling—the cases that replay in your head while you drive home, the patient you couldn’t save but can’t quite let go. “The Pitt” doesn’t overplay that weight; it acknowledges it. It treats emotional reality as part of professional reality.
Recently, a major newspaper ran a story dissecting a tragic patient outcome—an unexpected death after discharge, breakdowns across crowded systems. The headline written for shock value and clicks, but inside the profession it read differently. To those of us who live in those rooms, the pieces can feel quietly vindictive. A diagnosis not even two independent pathologists could make. They name names, flatten context, and turn uncertainty into accusation. What’s framed as transparency can land as punishment.
Emergency medicine already lives at the edge of uncertainty. Every shift is a collision of incomplete data, ticking clocks, and emotional exhaustion. We make irreversible calls while the story is still unfolding. When those same nights are replayed in the media as moral failure, it reopens old wounds. That’s secondary trauma layered on top of the first.
We know the cost. Emergency physicians have among the highest rates of burnout,
depression, and suicide in medicine. So when “The Pitt” opens its first episode with a doctor standing on the hospital roof—alone, drained, and nearly undone—it reads as recognition. Dr. Abbott teeters at the edge, then steps back after talking to Dr. Robby. Hours later, he’s back during an mass casualty incident—leading multiple resuscitations with calm precision. That juxtaposition—fragility and competence side by side—is why the show hits so hard. It mirrors the quiet resilience that defines so much of this field.
In a cultural moment where emergency physicians are too often portrayed only through tragedy or litigation, a show that humanizes without indicting feels almost radical. It gives the trauma we feel a mirror.
Some have pointed out that the show centers physicians and nurses, leaving less space for the rest of the team—ED pharmacists, respiratory therapists, techs, and others. That’s fair. Those roles are absolutely vital and add value to the ED. But not every ED has that level of support; many of us have managed BiPAP setups ourselves or adjusted infusions without a pharmacist nearby. I’ve worked in a Level One Trauma Center where I was doing my own EKGs and IVs. It is highly unlikely “The Pitt” is ignoring those team-members to purposefully ignore their contribution. It’s a story about physicians, the training they undergo, the experiences they share, and the lessons they carry. “Grey’s Anatomy” and other shows rarely
highlight surgical techs and other staff either. This show’s focus just lets the emergency physician step into the light for once.
From
Television shapes perception more than we like to admit. Patients, students, policymakers— they all carry those portrayals with them. For years, “just the ER doc” has meant expendable. “The Pitt” challenges that. It shows emergency physicians as decisive, deeply knowledgeable, capable of holding chaos together when everyone else is still paging back. It pairs intellectual rigor with emotional realism, without tipping into melodrama.
Emergency medicine isn’t triage dressed up as drama. It’s where medicine meets the unknown—where life and death are negotiated in real time by people who rarely get credit for how much that costs them.
So when millions of viewers see an emergency team leading resuscitations, managing traumas, nailing airways, performing nerve blocks, having hard goals-of-care discussions, or quietly regrouping after a loss, something shifts. The story changes. The perception evolves.
And maybe, just maybe, the next time someone says, “You’re just an ER doc,” they’ll hesitate— because now, thanks to “The Pitt,” they’ve finally seen what we do and who we really are.

Emergency medicine already lives at the edge of uncertainty. Every shift is a collision of incomplete data, ticking clocks, and emotional exhaustion. We make irreversible calls while the story is still unfolding.”
AAEM established its Foundation for the purposes of (1) studying and providing education relating to the access and availability of emergency medical care and (2) defending the rights of patients to receive such care and emergency physicians to provide such care. The latter purpose may include providing financial support for litigation to further these objectives. The Foundation will limit financial support to cases involving physician practice rights and cases involving a broad public interest. Contributions to the Foundation are tax deductible. Levels of recognition to those who donate to the AAEM Foundation have been established. The information below includes a list of the different levels of contributions. The Foundation would like to thank the individuals below who contributed from 9/1/24 to 9/1/25.
Contributions $1000 and above
Frank L. Christopher, MD FAAEM
Fred Earl Kency, Jr., MD FAAEM FACEP
Peter G. Anderson, MD FAAEM
Robert A. Frolichstein, MD FAAEM
Robert P. Lam, MD FAAEM
Contributions $500-$999
David W. Lawhorn, MD MAAEM
Eric D. Lucas, Sr., MD FAAEM
Glenn I. Goodwin, DO FAAEM
Julianne Wysocki Broadwater, DO FAAEM
Leonard A. Yontz, MD FAAEM
Travis J. Maiers, MD FAAEM
Contributions $250-$499
Alex Alers Fuentes, MD FAAEM
Andrew P. Mayer, MD FAAEM
Benjamin D. Walrath, MD MPH FAAEM FAEMS
Brian Phillip Doyle, MD FAAEM
Charles Chris Mickelson, MD FAAEM
David C. Crutchfield, MD FAAEM
Deborah D. Fletcher, MD FAAEM
Eric M. Sergienko, MD FAAEM
Eric W. Brader, MD FAAEM
Garrett Clanton II, MD FAAEM
James J. Schlesinger, DDS MD
Jamie J. Adamski, DO FAAEM
Jeffery M. Pinnow, MD FAAEM FACEP
Jeffrey A. Rey MD, MD FAAEM
John H. Kelsey, MD FAAEM
Jonathan D. Apfelbaum, MD FAAEM
Jonathan W. Riddle, DO
Joseph T. Bleier, MD FAAEM
Joshua J. Faucher, MD FAAEM
Karl A. Nibbelink, MD FAAEM
Kathleen P. Kelly, MD FAAEM
Kevin Allen, MD FAAEM
Kian J. Azimian, MD FAAEM
Laura J. Bontempo, MD MEd FAAEM
Lauren LaRoche, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Mark D. Thompson, MD FAAEM
Mark I. Langdorf, MD MAAEM FAAEM
MHPE
Mary Ann H. Trephan, MD FAAEM
Michael Luszczak, DO FAAEM
Nate T. Rudman, MD FAAEM
Oscar A. Marcilla, MD FAAEM
Patrick A. Aguilera, MD FAAEM
Phillip L. Rice Jr., MD FAAEM
Rosa K. Gigliotti, MD FAAEM
Salvador Villanueva, MD FAAEM
Steven Schmidt
Taylor G. Fletcher, MD FAAEM
Contributions $100-$249
Alexander Tsukerman, MD FAAEM
Alexandra Terskiy, MD PhD
Amanda Dinsmore, FAAEM
Ameer Sharifzadeh, MD FAAEM
Andrew Wilson, FAAEM
Ari Davis, FAAEM
Azalea Saemi, MD FAAEM
Benjamin Kober, DO FAAEM
Brendan P. Sheridan, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Brian Zimmer, DO FAAEM
Bruce E. Lohman, MD FAAEM
Carlos F. Garcia-Gubern, MD FAAEM
Chad J. Hansen, MD FAAEM
Christopher M. Tanner, MD FAAEM
Daniel P. Shand, MD FAAEM
Daniel T. McDermott, DO FAAEM
David L. Justis, MD PhD
David R. Hoyer Jr., MD FAAEM
Don L. Snyder, MD FAAEM
Douglas P. Slabaugh, DO FAAEM
H. Edward Seibert, MD FAAEM
Ilan Kaye, FAAEM
Jada Lane Roe, MD FAAEM
Jalil A. Thurber, MD FAAEM
Jeffrey B. Thompson, MD MBA FAAEM
John R. Matjucha, MD FAAEM
John Tobias Nagurney, MD MPH FAAEM
Jorge L. Infante, MD FAAEM
Julian G. Mapp, MD MBA MPH FAAEM
Justin P. Anderson, MD FAAEM
Kathleen Hayward, MD FAAEM
Kathryn Getzewich, MD FAAEM
Katrina Kissman, MD FAAEM
Keith D. Stamler, MD FAAEM
Kesah DeLisio, MD FAAEM
Kevin C. Reed, MD, FACHE, FAAEM
Kevin S. Barlotta, MD FAAEM
LaShell K. LaBounty, DO
Laura Cazier, MD FAAEM
Lawrence A. Melniker, MD MS MBA FAAEM
Marianne Haughey, MD MAAEM FAAEM
Mark A. Antonacci, MD FAAEM
Mark A. Newberry, DO FAAEM FPD-AEMUS
Mary Jane Brown, MD FAAEM
Matthew B. Underwood, MD FAAEM
Matthew W. Porter, MD FAAEM
Matthew William Carman, MD FAAEM
Michael L. Martino, MD FAAEM
Michael Timothy Schultz, MD FAAEM
Nicholas Boyko, DO, FAAEM
Paul W. Gabriel, MD FAAEM
Ramon H. Nunez, MD FAAEM
Regan Wylie, MD FAAEM
Robert Bruce Genzel, MD FAAEM
Robert E. Gruner, MD
Robert J. Feldman, MD FAAEM
Saba A. Rizvi, MD FAAEM
Sarah B. Dubbs, MD FAAEM
Scott D. Reiter, MD FAAEM
Scott P. Marquis, MD FAAEM
Sean Wilkie, MD
Stephanie Eden, MD FAAEM
Stuart M. Gaynes, MD FAAEM
Vinicius Knabben, MD
Vishal Patel, FAAEM
William E. Swigart, MD FAAEM
William K. Clegg, MD FAAEM
William Peter Kehr, MD FAAEM
William T. Freeman, MD FAAEM
Contributions up to $99
Alexander Guendel, MD FAAEM
Alexandra C. Doan, MD
Andy Doan
Anthony Catapano, DO FACOEP FAAEM
Brian Gacioch, FAAEM
Brian Knight
Caitlin E. Sandman, DO FAAEM
Chaiya Laoteppitaks, MD FAAEM
Dan M. Mayer, MD FAAEM FACEP
David I. Arbona-Calderon, MD FAAEM FACEP FAEMS
Donald L. Slack, MD FAAEM
Dylan M. Hendy, DO FAAEM
Eric J. Schwiger, DO FAAEM
Florence M. Nju Epse Fongang, MD
Gabriel Ochoa, MD FAAEM
Jennifer A. Martin, MD FAAEM
Jon J. Carpenter, MD
Justin L. Berkowitz, DO FAAEM
Laura Harvey, DO FAAEM
Lawrence Mendiola, DO FAAEM
Marc D. Squillante, DO FAAEM
Marc J. Dumas, MD FAAEM
Michael O’Neil, MD FAAEM
Michael Slater, MD FAAEM
Moath Amro, MD
Morgan E. Hanlon
Nancy Conroy, MD FAAEM
Neil Gulati, MD FAAEM
Patrick W. Daly, MD FAAEM
Rian Pillitteri, MD FAAEM
Ryan Horton, MD FAAEM
Sachin J. Shah, MD FAAEM
Sarat Chandra Uppaluri
Scott Beaudoin, MD FAAEM
Shelly Birch, FAAEM
Stephanie A. Ayala, DO
Tabitha Williams, FAAEM
Tatiana Nunez, MD
Tina F. Edwards, FAAEM
Vanessa C. Hannick, MD FAAEM
Vincent K. Huynh, DO
Virgle O. Herrin Jr., MD FAAEM
Yeshvant Talati, MD

AAEM PAC is the political action committee of the American Academy of Emergency Medicine. Through AAEM PAC, the Academy is able to support legislation and effect change on behalf of its members and with consideration to their unique concerns. Our dedicated efforts will help to improve the overall quality of health care in our country and to improve the lot of all emergency physicians.
All contributions are voluntary and the suggested amount of contribution is only a suggestion. The amount given by the contributor, or the refusal to give, will not benefit or disadvantage the person being solicited.
Levels of recognition to those who donate to the AAEM PAC have been established. The information below includes a list of the different levels of contributions. The PAC would like to thank the individuals below who contributed from 9/1/24 to 9/1/25.
Contributions $1000 and above
Mark S. Penner, DO FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM FACEP
Jeffery M. Pinnow, MD FAAEM FACEP
Julianne Wysocki Broadwater, DO FAAEM
Contributions $250-$499
Eric W. Brader, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Mark D. Thompson, MD FAAEM
Mark E. Zeitzer, MD FAAEM
Robert A. Frolichstein, MD FAAEM
Steven Schmidt
Teresa Camp-Rogers, MD MS FAAEM
Contributions $100-$249
Andrew M. Bazakis, MD FAAEM
Brendan P. Sheridan, MD FAAEM
Brian Phillip Doyle, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Chaiya Laoteppitaks, MD FAAEM
David R. Hoyer Jr., MD FAAEM
Eric M. Ketcham, MD MBA FAAEM FASAM
Garrett Clanton II, MD FAAEM
Ilan Kaye, FAAEM
Jada Lane Roe, MD FAAEM
Jalil A. Thurber, MD FAAEM
Jeffrey A. Rey MD, MD FAAEM
Jeffrey B. Thompson, MD MBA FAAEM
Jorge L. Infante, MD FAAEM
Joseph T. Bleier, MD FAAEM
Julian G. Mapp, MD MBA MPH FAAEM
Justin P. Anderson, MD FAAEM
Kathleen Hayward, MD FAAEM
Kathryn Getzewich, MD FAAEM
Katrina Kissman, MD FAAEM
Matthew B. Underwood, MD FAAEM
Matthew W. Porter, MD FAAEM
Nate T. Rudman, MD FAAEM
Nicholas Boyko, DO, FAAEM
Paul W. Gabriel, MD FAAEM
Peter G. Anderson, MD FAAEM
Ramon H. Nunez, MD FAAEM
Robert Bruce Genzel, MD FAAEM
Rosa K. Gigliotti, MD FAAEM
Sachin J. Shah, MD FAAEM
Sean Wilkie, MD
Stephanie Eden, MD FAAEM
Vinicius Knabben, MD
William T. Freeman, MD FAAEM
Contributions up to $99
Ameer Sharifzadeh, MD FAAEM
Anthony Catapano, DO FACOEP FAAEM
Brian Gacioch, FAAEM
Jennifer A. Martin, MD FAAEM
John Havlick, FAAEM
Justin L. Berkowitz, DO FAAEM
Laura Harvey, DO FAAEM
Lawrence Mendiola, DO FAAEM
Marc D. Squillante, DO FAAEM
Michael Slater, MD FAAEM
Neil Gulati, MD FAAEM
Stuart M. Gaynes, MD FAAEM
Tina F. Edwards, FAAEM
Virgle O. Herrin Jr., MD FAAEM
Contributions $1000 and above
Fred Earl Kency, Jr., MD FAAEM FACEP
Contributions $500-$999
David W. Lawhorn, MD MAAEM
Frank L. Christopher, MD FAAEM
Contributions $250-$499
Alex Alers Fuentes, MD FAAEM
Dale S. Birenbaum, MD FAAEM
Eric W. Brader, MD FAAEM
Jeffery M. Pinnow, MD FAAEM FACEP
Joseph T. Bleier, MD FAAEM
The AAEM Institute for Leadership, Education & Advancement in the Development of Emergency Medicine, Inc. (LEAD-EM) was established after the tragic and unexpected death of AAEM president, Dr. Kevin G. Rodgers.
The Kevin G. Rodgers Fund and the Institute will LEAD-EM just like Dr. Rodgers did. The funds will support important projects such as development of leadership qualities, and clinical and operational knowledge of emergency physicians with a view toward improving and advancing the quality of medical care in emergency medicine, and public health, safety and well-being overall. LEAD-EM would like to thank the individuals below who contributed from 9/1/24 to 9/1/25.
Kian J. Azimian, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Oscar A. Marcilla, MD FAAEM
Robert A. Frolichstein, MD FAAEM
Contributions $100-$249
Ari Davis, FAAEM
Brian R. Potts, MD MBA FAAEM
Daniel P. Shand, MD FAAEM
John R. Matjucha, MD FAAEM
Julian G. Mapp, MD MBA MPH FAAEM
Julianne Wysocki Broadwater, DO FAAEM
Kailyn Kahre-Sights, MD FAAEM
Kathleen Hayward, MD FAAEM
Kevin C. Reed, MD, FACHE, FAAEM
Mark A. Antonacci, MD FAAEM
Matthew B. Underwood, MD FAAEM
Scott P. Marquis, MD FAAEM
William T. Freeman, MD FAAEM
Contributions up to $99
Brandon H. Richardson
Casey Brock Patrick, MD FAAEM FAEMS
David A. Yacynych, MD
Florence M. Nju Epse Fongang, MD
Gerald E. Maloney, Jr., DO FAAEM
Ivan C. Rokos, FAAEM
Jon J. Carpenter, MD
Justin L. Berkowitz, DO FAAEM
Leah C. Harbison, MS
Mary Jane Brown, MD FAAEM
Michael Slater, MD FAAEM
Neil Gulati, MD FAAEM
Robert E. Gruner, MD
Sarat Chandra Uppaluri
Stuart M. Gaynes, MD FAAEM
Tatiana Nunez, MD
Thomas G. Derenne
Virgle O. Herrin Jr., MD FAAEM
Introducing the AAEM and AAEM/RSA Events Calendar — your go-to source for conferences, webinars, workshops, and more. Explore the latest opportunities to connect, learn, and grow in emergency medicine by scanning the QR code.
“Nightmare Corner” in the ED – Louisiana Chapter Division of AAEM (AAEMLa) –October 29, 2025 (Baton Rouge, LA) 2025 Oral Board Review Courses - Late Fall Course Dates: November 18, November 19, November 25 - aaem.org/education/ oral-boards/
13th Annual FLAAEM Scientific Assembly November 21-22, 2025
Four Corners+ Regional Educational Day January 7, 2026 (Virtual)
32nd Annual Scientific Assembly April 11-15, 2026 (Seattle, Washington)
Recommended
Online CME
Rapid Response to Adverse Events of Bispecific Antibodies: Follicular Lymphoma and Diffuse Large B-Cell Lymphoma Emergency Medicine Strategies - https://www. staging.medscape.org/viewarticle/1001569
Online CME
Recognizing Life-Threatening Emergencies in People with VEDS thesullivangroup.com/TSG_UG/VEDSAAEM/
The Difficult Airway Course: EmergencyTM November 14-16, 2025 (San Diego, CA) theairwaysite.com/a-course/ the-difficult-airway-course-emergency/
Explore AAEM CME Online, where we understand the fast-paced nature of emergency medicine (EM) and the need for concise, accessible education. This platform is designed to provide members of the American Academy of Emergency Medicine (AAEM) and AAEM Resident and Student Association (AAEM/ RSA) with top-tier continuing medical education (CME) resources right at their fingertips. Access today!

Amanda Dinsmore, MD, Kendra Morrison, DO, and Laura Cazier, MD



Have you ever left a shift, driven home, and found yourself unable to get out of the car?
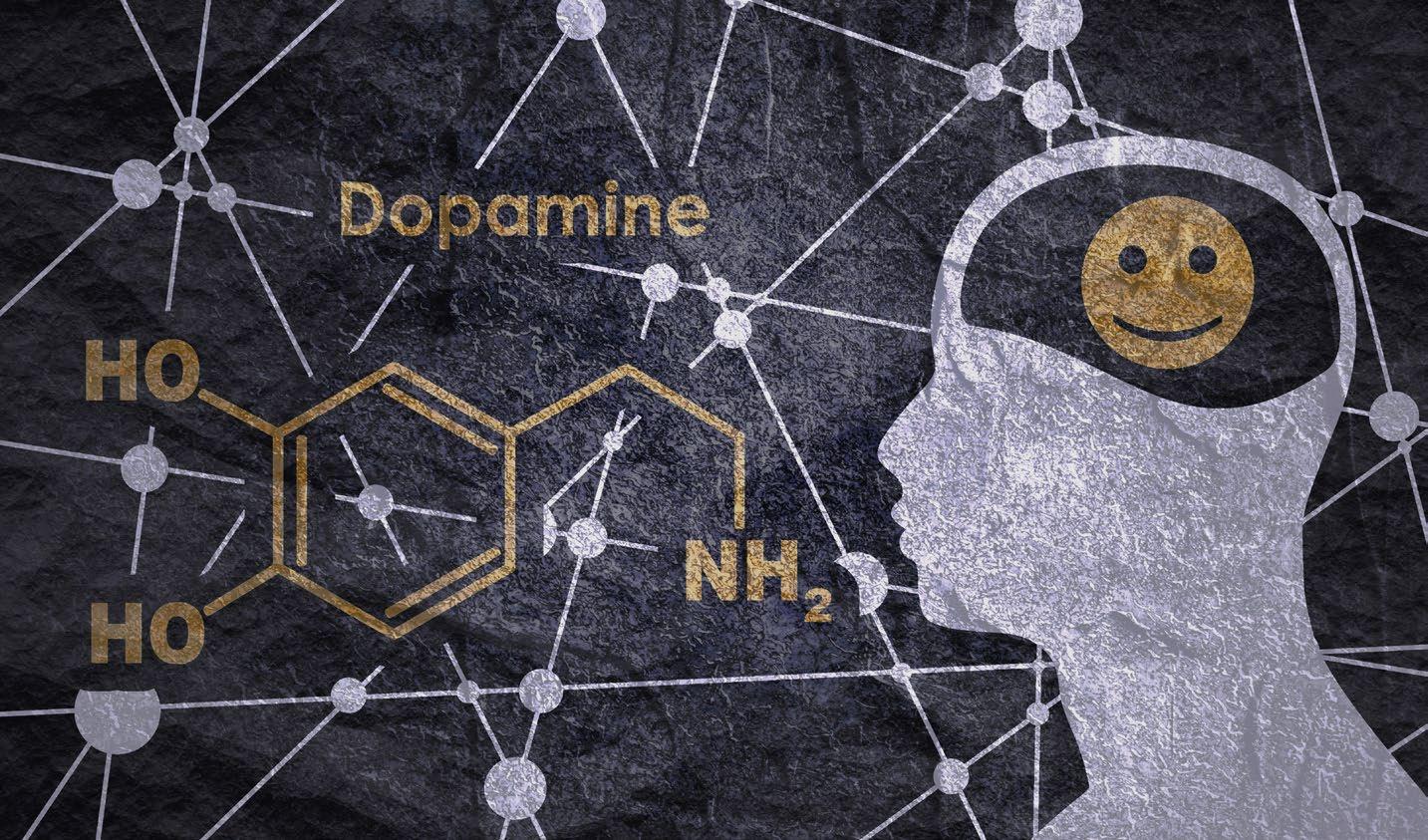
Sometimes for hours? At the peak of my burnout, and even occasionally now, this was me. I called it post-shift zombification: a sense of being drained, detached, and stuck in neutral. I knew it came from overstimulation, but I couldn’t put words to why it felt so consuming. Only later did I learn what was happening in my brain: I wasn’t lazy, and I wasn’t broken. I was experiencing the fallout of a dopamine crash.
Emergency medicine is a specialty built on adrenaline, quick decisions, and the constant hum of uncertainty. But beneath the chaos lies a quieter neurochemical force that shapes how we feel on and off shift: dopamine. More than a “pleasure chemical,” dopamine is the brain’s driver of motivation, reward, and anticipation. For physicians, its effects can be both sustaining and destructive.
Dopamine in the ED: Hooked on Anticipation
When you crack a difficult diagnosis, resuscitate a crashing patient, or land the tube on the first attempt, dopamine is there. It reinforces successful behaviors and motivates you to push through the next challenge. Yet dopamine is triggered less by reward itself and more by anticipation. That’s why the triage board refresh, the vibration of a phone in our pocket, or notification of new lab results can feel addictive in their own right. The uncertainty of “what’s next?” keeps the dopamine system firing.
I called it post-shift zombification: a sense of being drained, detached, and stuck in neutral… Only later did I learn what was happening in my brain: I wasn’t lazy, and I wasn’t broken. I was experiencing the fallout of a dopamine crash.”

Dopamine also helps explain the early thrill of residency. The novelty of each “first”—first intubation, first thoracotomy, first shift running the pod—generates surges of dopamine that reinforce learning. Later in one’s career, when novelty fades, physicians may feel restless or seek out additional responsibilities without realizing that part of what they’re chasing is neurochemical.
Just as dopamine surges during acute events, it falls afterward. Every emergency physician knows the flatness of walking into a quiet home after a chaotic shift or the sense of letdown after a series of dramatic saves. This “dopamine crash” can mimic depression or fatigue, and when layered on top of chronic stress, it contributes to the numbness so many clinicians describe.
Research supports this physiology. In a crossover trial of emergency physicians, urinary dopamine levels were significantly lower during
Dopamine is our friend. We need it. It fuels learning, motivation, and resilience. And it feels great! The challenge is to harness it without letting it hijack us.”
24-hour shifts compared to shorter or control days, and levels still hadn’t recovered by the third day afterward. In other words, the crash isn’t just subjective—it’s measurable, and it lingers.
This may help explain why physicians sometimes feel emotionally blunted or drained well beyond their scheduled shifts. The body’s motivational circuitry is struggling to recalibrate.
Dopamine Off-Shift: Searching for Substitutes
Off-shift, the brain often looks for ways to replace work surges. For some, that means quick hits: scrolling, snacking, alcohol, or late-night streaming. These provide temporary relief but blunt dopamine sensitivity, making baseline life feel less rewarding.
Alternatives include exercise, playing or dancing to music, spending time in nature, or creative hobbies. These activities engage dopamine more sustainably and also activate serotonin and endorphins, which stabilize mood. The difference is important: overstimulation can worsen the crash, while balanced outlets can help the system reset.
Families often notice before we do. Partners may point out irritability or emotional absence; kids sense when we’re physically present but mentally elsewhere. These subtle cues often signal that the dopamine system is out of balance.
Tool
Many emergency physicians rely on caffeine, and some turn to prescribed wake-promoting agents like modafinil during long stretches or post-shift fatigue. These stimulants work in part by increasing dopamine availability in the brain’s reward pathways. That’s why a cup of coffee sharpens focus and why modafinil has been studied in shift work disorder.
But the flip side is that when the stimulant effect wears off, dopamine activity can dip below baseline. In other words, the “crash” after a night of heavy caffeine isn’t just about sleep debt, it’s also neurochemical withdrawal. Over time, reliance on stimulants may deepen the highs and lows of the dopamine cycle.
This doesn’t mean stimulants should be abandoned; caffeine and modafinil are both validated tools for shift work fatigue. But physicians should be aware that they may amplify the very roller coaster we’re trying to smooth.
From Zombie to Human: Recovering from the Dopamine Crash
The good news: dopamine pathways are plastic. With intention, we can reset the system and protect ourselves from slipping into that postshift zombified state. A few strategies:
• Micro-rewards at work: Celebrate the small victories—kind interactions, smooth discharges, teaching moments—not just big saves. This keeps dopamine balanced rather than swinging wildly.
• Novelty with intention: Since dopamine thrives on newness, choose off-shift novelty that restores (new hikes, recipes, hobbies) instead of mindless scrolling that deepens the zombification.
• Grounding practices: Protect sleep, meditation, prayer, or even simple routines like folding laundry. These slower activities quiet the dopamine system, preventing the crash that leaves us foggy and flat.
• Digital hygiene: Treat screens like tools, not slot machines. Screen-free hours or days give your dopamine system a chance to reset, helping you feel human again instead of undead.
• Meaning over hits: Anchor satisfaction in values and relationships rather than in the next dopamine hit. Meaning is the antidote to the zombie state of numbness. Spending intentional time with those we love, including friends (and pets!) helps even out dopamine release and promote a sense of well-being.
• Self-compassion: Self-compassion is key to improving any burnout symptom. “It makes sense that I feel totally checked out. And yet-sitting here in the car isn’t going to help me feel better, so I’m going to get out and do something to take care of myself in a more productive way.”
Continued on page 19 >>
Amy Walsh, MD MDP

When I was 16, I read “The Plague” by Albert Camus. I admired Dr. Rieux so much. I wondered if I was made of the same stuff.
The questions are the same. I knock on the door to room three, but walk right in. I’ve heard this story 300 times: fever, cough, trouble breathing, weakness. Two questions in, knock, knock. “Cardiology on the phone for you…” “Regional on the phone for you…” “Hospitalist on the phone for you…” I step out of the room, peel off the gloves, drag off the face shield, lower the mask below my chin, and untie the gown. I pick up the phone.
When the pandemic started, my tiny rural hospital waited. While I was waiting, I wrote letters.
Dear Friend One,
There is a strange push and pull to life right now, the peace of hands in the dirt and slowness, followed by a frenetic, almost shaking anxiety. Everything changes so fast! We even have easel paper on the wall. Shari scrawls across them in blue Sharpie, bulleted lists, when can you wear an N95 mask, when can you wear a surgical mask, who can get tested, how soon will tests come back. When one sheet is full, she tears it down and tapes the next one up, sometimes four times a day.
I watch what’s happening in New York and Italy. I have wondered if I am the type of person who stays or runs. A small part of me wants to find out.
I hope you get a chance to write back. I’m trying to make the best of this and hoping we can become even closer when this is all over.
If you don’t know what to put in the letter, I’d love to learn:
1. What are you proudest of?
2. Where is your favorite place?
3. What are three values your parents taught you? Mine are self-sufficiency, to try your hardest, to be of service.
We saw refrigerated trucks behind hospitals and pots banging on balconies. We saw New York and Italy stretched beyond breaking while we sat in our ergonomic chairs in ghost towns.
Six months later, the wait was over. We were in the thick of it. It was difficult, but in the comforting way that shared hardship unites people. The system was still set up to mostly support caring for people in the right way.
The next summer, it was “Hot Vax Summer,” the summer everyone else moved on. Many people in our community had omitted the vax part. Younger and younger patients were coming into the hospital sicker and sicker. Delta. We were already exhausted from surge after surge; we had

When the pandemic started, my tiny rural hospital waited. While I was waiting, I wrote letters.”
some of the highest rates of COVID infections in the country that winter and spring.
“Sure we’ll take him. We’ll have a bed tomorrow…in two days…”
Whatever the diplomatic way of saying, “Fuck if I know when we’ll have a bed,” is.
“Did you ever call and update the family on room four?” asked Emma.
I never knew what I wanted to be when I grew up, not for long anyway: war-zone photographer, FBI agent, attorney crusading for justice. Looking back now, I can see what I wanted to be: a hero.
“Did you ever receive my letter?” I texted to ask Friend Two.
“No.”
I didn’t believe her.
“Hey, can we get together. I have something I’d like to talk to you about.”
She canceled two hours beforehand. She never rescheduled.
“No, do we have a bed for room nine?”
“No, unless we can commit her, we’ll just have to keep calling around every few hours.”
“Room eight wants to know what’s going on!” I hear from across the hall.
“I’ll talk to them once I update room six on her transfer and finally see room three.”
I watch what’s happening in New York and Italy, and I wonder, “Do I have what it takes?”
You will begin to step deeper toward the underworld in these next weeks.
I saw a patient for a problem after a procedure that would get better on its own. I thought he left happy. Two days later, he sent the hospital a letter. He threatened to sue.
“When will room four be able to go to the floor? And can you talk to radiology, that x-ray for two is taking forever.”
“Hey, I’m hosting a story share for my 40th birthday. It’s part of a healing thing I’m doing. It’s really important to me.” Friend Three canceled because it was raining at his campsite, and he wanted to go directly home instead of to my house.
A patient you saw died unexpectedly. We will peer review the case. My heart was a rabbit running from a wolf. It darted unpredictable directions, evaded capture, and out of the blue, at inconvenient times collapsed completely.
Tears shoved at my sinuses and panic scrambled from my chest to any unoccupied small caverns it could find. A nurse, my friend, walked by, “Hi Dr. Walsh, how are you?” I turned and the tears streamed down my cheeks. She stepped back, unprepared as she was for a response that wasn’t “Fine.” I blubbered something. She grabbed me by the shoulders, looked me in the eye, “You’re one of the best doctors here. We all love you,” she consoled. All I had wanted was to feel loved, but it was too little too late.
“Room three’s breathing is getting worse.” I slide the slick, urine yellow gown over my arms and tie it behind my neck. The first red rubber band stretches and falls underneath my bun, the second above it. The blue-violet nitrile gloves slide over my hands and the white cuff of my gown.
“Urgent care is sending someone over and PD is coming with an agitated guy from jail,” a nurse hollers over the counter as I pull up my mask and knock on room three’s door again.
“How are you guys holding up?” I text Friend One. No response. For weeks.
“Thinking of you!”
No response. For weeks.
“Hey, I miss you guys. If I did something to upset you, I’d love to have a chance to clear the air.” No response.
I have wondered if I am the type of person who stays or runs. A small part of me wants to find out.
Beautiful Souls,
You have been called by the Wilds of your Soul, the Ancestors, and the beings of the otherworld, who are courting you to Wales for a Vision Fast Wilderness Vigil this September.
The Descent has begun. You will begin to step deeper toward the underworld in these next weeks.
Eventually, I would travel to Wales for the Vision Fast. Even before we set out on our own, the land and waters called to me. Mist of the waterfall kissed, coated my skin. My toe hovered above water guarding against the harsh cold that makes bones ache. With a deep breath, my toes dipped into gentle, smooth, refreshing, cool, awakening, enlivening. Afterward, out on the rock, a gentle, pleasant prickle caressed my skin as it air-dried. Alive with the smell of green, wet. Once again submerged into my own skin.
As I sat by the water, I felt the call for deep rest. My back rested on earth, rain on skin. I laid, I slept, I curled into a spiral, into deep stillness. Longed for but never granted. As I stood by the water, I found a stone
Continued on page 21 >>

As I sat by the water, I felt the call for deep rest…I returned centered, connected to my desire, planning to slowly and gracefully make my exit from medicine.”
Mary Unanyan, DO
The landscape of emergency medicine is constantly evolving, and so too are the ways in which physicians are assessed and certified. The American Board of Emergency Medicine (ABEM) will introduce a new certifying exam in 2026, replacing the long-standing oral board exam. These changes aim to create a fair, more comprehensive evaluation that aligns with real-world clinical practice. With the shift to a new format, many candidates and educators are eager to understand the rationale behind these updates and what they mean for the future of our specialty. To explore the motivations driving these changes, the impact on candidates, and how the new exam aims to ensure fairness, accessibility, and relevance, I sat down with the President of ABEM Dr. Diane Gorgas for an in-depth discussion on the future of certification in emergency medicine.
MU: The North Carolina center is the same one that anesthesiology uses to host their certifying exam. It sounds like it will be wellequipped to administer the exam.

Dr. Mary Unanyan: Hello Dr. Gorgas, thank you so much for meeting with me. Can you provide a brief overview of the changes made to the ABEM certification process?

Dr. Diane Gorgas: Thank you for the opportunity. Historically, certification for ABEM has been a two-step process. The first is a written medical knowledge clinical reasoning exam called the qualifying exam. The second portion of that was an oral exam which, during COVID, had to move to a virtual oral exam. The first half of certification is not changing at all. Shortly after you graduate from residency, or even while you’re in residency, you will register to take the first part of the certification process, the qualifying exam.
Upon passing the qualifying exam, you will receive a registration for the new certifying exam. We are moving from a virtual oral exam to a certification exam that is new and different. It was never ABEM’s intent to remain virtual but rather return to an in-person format. The virtual format was to allow physicians to become certified during the pandemic as well as the period prior to transitioning to the certifying exam. It is an in-person examination that is going to be held in Raleigh, North Carolina. It’ll be held nine times each year, which will increase the flexibility and scheduling options available for exam candidates. The extra flexibility should be nice for you all, as currently the exam takes place only three times a year.
DG: Yes, it’s a center that’s well equipped for it. The American Board of Anesthesiology also has a certifying exam there. The American Board of Oral and Maxillofacial Surgery and the American Board of Urology hold their exams there as well. It is not just an oral exam testing center. It’s much more of a simulated environment that has capacity for high-volume assessments. We have over 3,000 emergency medicine graduates that are seeking board certification. So, we need a process that can fairly, ubiquitously, and uniformly assess over 3,000 different candidates in a year.
MU: From my understanding, in the COVID era, board certifications for essentially all specialties turned virtual and we are actually one of the last specialties to switch over to an in-person format because we are trying to revamp the certification. Was that correct?
DG: Yes, that’s correct. Of the American Board of Medical Specialties, meaning if you look at all the medical boards that are out there, more than half of them have an oral certification process. The majority of those have moved back to an in-person certification process. And the reason that we are still using the virtual format for the next year until 2026 is that we are doing this major revamp of the certifying exam.
MU: What motivated these changes? Were there specific concerns or feedback from the emergency medicine community about certification that influenced this decision to revamp the exam?
DG: Really, it’s a multifactorial answer to that. Part of the reason is that we want an exam that really replicates what you do in the emergency department. There was a lot of contextualization of the virtual oral exam. Normally during oral boards, a candidate will start with “I walk into a room, what do I see, hear, and smell?” Now we can put you in a room that you can see, hear, and smell things instead. Let’s put the scenario into a real life setting so that you can understand and practice within the environment. The whole environment of the new certifying exam should be that you can be in your scrubs with your tennis shoes on, walk out of an emergency department shift, walk into the assessment center, and feel

comfortable. You should feel like you are practicing medicine the way that you practice it at the bedside. The reality and the relevance of the exam were two huge motivating pieces.
We also understand that we’re really at an inflection point in medicine with artificial intelligence (AI) and computer-generated diagnostics and augmented decision making coming into reality for us all. We needed an environment where we could start to implement assessing candidates on their ability to utilize external resources in their decision making. Version 2.0 of the certifying exam will likely start to encompass those things. It’s a surprise to no one that there has been a recent pretty significant growth in the number of emergency medicine training programs out there. And to this date, no specialty, not surgery nor any of the surgical specialties, not medicine, not pediatrics, and not even emergency medicine has done any procedural competency assessments. Emergency medicine will be the first specialty that looks at a candidate’s ability to competently perform a procedure, which is a critical component of clinical competency. These procedures are the same hands-on procedures that we do every day and that are expected of emergency medicine residency graduates. We will also be looking at ultrasound competency as part of this assessment as well. This is all to make the testing environment feel more realistic, so it will be a seamless transition from what you do in the clinical setting to what you will do in the assessment setting. It expands on these topics and really looks at communication skills, procedural skills, and clinical decision making.
MU: I agree. I think procedural competency is crucial to clinical practice. Given how procedure numbers are a residency graduation requirement, it is surprising that we aren’t already evaluated on it. For these assessments, is it going to be another board-certified emergency physician watching you do an arterial or central line? Is it talking through steps or is it watching us run through a simulation on a mannequin?

DG: It will be a combination of all those things. All our onsite examiners are board-certified emergency physicians who have been specially trained on assessment and examination skills. For the procedure station, you will be given a clinical vignette, asked to not only discuss the indications and contraindications of the procedure and any complications you may look for, but you will also be asked to do that procedure in a simulated environment that is very much accessible to all emergency medicine training programs. We’re not bringing in million-dollar simulators for these. They’re what we would call in the simulation environment “low-fidelity” simulators. So you will be asked to secure an airway or to demonstrate how to do any given procedure that’s part and parcel of what we do in emergency medicine. The same with ultrasound. You’ll be given a clinical vignette. There’ll be an ultrasound machine and a patient in the room. You’ll be asked to tell us which ultrasound exams you want to do to gather information on that patient. You’ll be asked to select a probe, obtain images, and interpret those images. Again, very much what you do in the emergency department on a day-by-day basis.
MU: I was just about to say, it sounds exactly like when I’m on shift and have to obtain informed consent before performing the procedure itself. It feels reassuring that the exam will essentially replicate what I’m already doing on a shift.


DG: That’s a true opportunity to show off, right? And this is what you do. This is what you’re good at.
MU: I would hope so! And for the patients, is it going to be manikins? Is it going to be real people, like standardized patients?
DG: Of course for the procedures, we can’t actually ask anybody to undergo 12 or 16 intubations in one day. But there will be simulators involved with the procedures themselves. For ultrasound, at least for the initial phases of ultrasound, there’ll be real patients that you’re asked to obtain images on.
MU: Is it going to be similar to how simulation is often run at residency programs during their didactics?

DG: Yes, but in residency didactics, a simulation can sometimes be a group activity and it can also be on high fidelity simulators meaning a single simulator that has the capability of having multiple procedures completed on it. These are kind of unit task simulators. So, the video example that’s out there for our simulation or for the procedure station is one of an arthrocentesis of the knee. You’ll see in that video that all you’re going to get is a knee and an arthrocentesis kit. And you should be able to talk through how you would do that and then demonstrate how you would do it.
MU: How does ABEM plan on grading the procedures and ultrasounds? Is there going to be differing weights on technique versus anatomy versus indications/contraindications? Is it a checklist scoring sheet?
DG: It is a holistic scoring sheet. As a matter of fact, the examiner has opportunities at the bottom to just state how the candidate did overall. There are assessment points along the way on important parts of procedures such as using sterile technique when required to. There may be assessment points on image acquisition when performing ultrasounds. And I do want to emphasize here that as many residency training programs as there are across the nation, it seems like there are that many different ultrasound machines. You’re not expected to come to the ABEM assessment and know the knobology. The machine will be on. You will have to select a probe. You will have to put that probe on a patient. Then if you want the depth or the gain or the mode adjusted, all you need to do is tell the examiner and they will adjust it for you. You’re going to be looking at the screen and should know the quality of the images that you’re getting. So, there will be granular assessment points on how Continued on page 31 >>




Nick Hakes, Mphil and Mel Ebeling, MD


For most patients, a visit to the emergency department begins not with a stretcher, but with a chair in the waiting room. In a field that prides itself on efficiency and throughput metrics, the waiting room remains both a logistical bottleneck and a powerful psychological space. While interventions to improve emergency care have historically focused on clinical outcomes, mounting evidence suggests that addressing the perception of care—specifically, perceived wait times—may hold untapped potential for improving patient satisfaction without major systemic overhaul.1-5
Operations management distinguishes between two goals: improving objective performance and improving customer experience. The former addresses throughput; the latter targets perception. In emergency medicine, wait times sit at the intersection. A patient who waits 45 minutes but is informed, reassured, and kept engaged may report higher satisfaction than one who waits 20 minutes in silence and uncertainty.
This distinction is captured in the service quality framework developed by Parasuraman, Zeithaml, and Berry, which defines quality as the difference between perceived performance and expectation.6 Expectations are shaped by past experiences, word of mouth, and the urgency of the presenting complaint. If unmet,
From a policy and design perspective, the waiting room should not be viewed as separate from care. It is the beginning of the patient journey.”

they widen “Gap 5,” the critical divergence between expected and perceived service. Addressing this gap does not always require provision of faster care; rather, it necessitates smarter communication.
There are five evidence-based factors that shape how patients perceive time spent in waiting rooms.7,8 These principles are rooted in queuing psychology, which has been applied for decades in retail and hospitality. In healthcare, however, the waiting room is too often treated as a passive holding space, rather than the opening chapter of the patient experience.
• Service environment design. A well-maintained environment reduces anxiety by conveying competence, safety, and respect. Patients often interpret environmental cues like cleanliness, lighting, and seating as signals of overall care quality.8-10 A neglected waiting room may subconsciously erode trust in the clinical care that follows. Actionably, clean the waiting room regularly, prioritize natural light, minimize clutter, and employ simple design elements like plants or art to create a sense of order and care.

• Early interactions during the wait. The first point of contact has an outsized effect on patient perception. According to service psychology, the anchoring effect is a phenomenon where people anchor expectations to initial experiences. A warm greeting, brief orientation, and simple reassurance helps patients feel acknowledged and reduces feelings of abandonment.8-10 Explaining the triage process can also mitigate perceived unfairness in wait order, particularly for low acuity cases.8-10 Actionably, emphasize the importance of a warm greeting to front desk staff and use volunteers or ancillary staff as greeters to explain the emergency department journey, set realistic expectations, and provide updates.
• Occupied versus unoccupied time. Queuing psychology has established that unoccupied time is perceived as longer than occupied time. When patients are engaged—even by low effort tasks like completing registration, medical history, or research forms—their perception of wait duration contracts.8-10 This technique also fosters a sense of progression, converting passive waiting into active participation. Actionably, give patients forms to complete and allow them to fill them out while waiting. Alternatively, provide handouts detailing the emergency department journey, frequently asked questions, or other educational content for patients to read.
• Uncertain versus known wait times. Psychological discomfort increases when people feel a lack of control or clarity. Providing estimated wait times, even if imperfect, reduces anxiety and enhances perceived transparency. Studies show patients prefer some information to complete silence.8-10 Electronic estimated wait time boards in the waiting room are one potential option. With the advent of artificial intelligence, new start-ups offer promising solutions for provision of patient-specific wait times.11
• Early process initiation. Medical interventions like collecting a history, measuring vital signs, or drawing labs are powerful signs that care has begun. This disrupts the perception of “just waiting” and shifts the narrative to “being treated.” Early initiation also gives patients psychological relief that their time is being used efficiently, which may buffer frustration with waiting.8-10 Actionably, adopt the physician-in-triage model to begin care sooner.12,13
Many emergency departments already use queuing theory to optimize patient flow, fast track low-acuity cases, and balance staffing. But the waiting room itself is rarely redesigned with queuing psychology in mind. In other industries, principles such as “occupied time feels shorter than unoccupied time” and “uncertain waits feel longer than known waits” are applied routinely.7 These industries invest heavily in
queue design, real-time updates, and sensory cues to minimize perceived wait burdens. Healthcare, by contrast, rarely applies this science with the same intentionality.
Even small operational changes can have outsized psychological effects. Informing patients how long they are likely to wait, explaining delays, or introducing visual progress indicators can meaningfully shift perceptions.8 These adjustments cost little, demand no regulatory reform, and require no expansion of clinical infrastructure. Yet they are rarely standardized in emergency departments, where attention remains focused on reducing actual door-to-physician times.
emergency department journey and estimated wait time ranges at each step. Patient experience scores improved, even when median wait times remained unchanged. Notably, improvements were not contingent on architectural redesign or additional staffing. The change was cognitive.
If a coffee chain can inform a customer when their latte will be ready, surely an emergency department can offer some queue transparency, even if only to explain delays or outline the steps ahead.”
A case study from Cambridge University Hospitals demonstrated how applying queuing principles and service quality models improved not only efficiency but also satisfaction.14 The intervention included visual wait time boards and proactive communication that framed the waiting period as purposeful rather than passive. For example, Cambridge simplified the signage in the waiting room to the minimum necessary. This included adding a sign with photos of each type of staff member sorted by scrub color so patients could understand who does what as well as a flowchart detailing the
Other countries have built on similar insights. In the Netherlands, patients referred to the emergency department after contacting after-hours primary care services receive detailed instructions before they arrive, reshaping expectations early.15 Meanwhile, some British hospitals have experimented with sensory design such as music, lighting, and visual cues to reduce anxiety in pediatric emergency waiting areas. Also seen in some pediatric emergency departments in the United States, adult emergency departments could benefit from the same design thinking. While these efforts remain underevaluated at scale, they point to a growing understanding: patient satisfaction begins before the encounter starts.
Patients evaluate service quality across multiple dimensions: reliability, responsiveness, assurance, tangibles, and empathy.6 Each can be influenced before the clinical encounter even begins. A reliable check-in process, responsive updates, clear signage, and kind gestures build trust and shape expectations. This matters. According to the United Kingdom’s National Health Service, elements like comfort, kindness, and clarity have as much, if not more, impact on satisfaction than the actual length of wait.7
Operations research reminds us that performance metrics shape behavior: what you get is what you measure.7 While clinical outcomes must remain paramount, patient satisfaction is not peripheral. It plays an active role in care delivery. When patients leave without being seen, become aggressive toward staff, or delay seeking care due to negative past experiences, outcomes suffer. Simple, low-cost interventions that improve perceived wait times and communication can reduce these risks while enhancing trust, safety, and flow. No single metric can
capture the complexity of patient experience. But perception remains one of the most accessible and underutilized levers we have.
From a policy and design perspective, the waiting room should not be viewed as separate from care. It is the beginning of the patient journey. In the same way that physician-in-triage models have shortened clinical delays, psychology-in-triage strategies could mitigate perceptual ones. Training staff in expectation management, scripting updates, and providing
1. Bleustein C, Rothschild DB, Valen A, Valatis E, Schweitzer L, Jones R. Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care. 2014;20(5):393-400.
2. Dansky KH, Miles J. Patient satisfaction with ambulatory healthcare services: waiting time and filling time. Hosp Health Serv Adm. 1997;42(2):165-177.
3. Camacho F, Anderson R, Safrit A, Jones AS, Hoffmann P. The relationship between patient’s perceived waiting time and officebased practice satisfaction. N C Med J. 2006;67(6):409-413.
4. Leddy KM, Kaldenberg DO, Becker BW. Timeliness in ambulatory care treatment. An examination of patient satisfaction and wait times in medical practices and outpatient test and treatment facilities. J Ambul Care Manage. 2003;26(2):138-149. doi:10.1097/00004479200304000-00006
5. Preyde M, Crawford K, Mullins L. Patients’ satisfaction and wait times at Guelph General Hospital Emergency Department before and after implementation of a process improvement project. CJEM. 2012;14(3):157168. doi:10.2310/8000.2012.110590
clear timelines could yield satisfaction gains on par with throughput improvements.
There are also commercial lessons to borrow. Retailers use digital signage, feedback kiosks, and even apps to create perceived control and transparency. If a coffee chain can inform a customer when their latte will be ready, surely an emergency department can offer some queue transparency, even if only to explain delays or outline the steps ahead. While injury acuity will always reshuffle priorities, patients value communication that acknowledges the wait and clarifies what to expect.
6. Parasuraman A, Zeithaml VA, Berry LL. A Conceptual Model of Service Quality and Its Implications for Future Research. Journal of Marketing. 1985;49(4):41-50. doi:10.2307/1251430
7. Davies J. Operations Management Lecture 2. Lecture presented at: Cambridge Judge Business School; May 6, 2025; Cambridge, United Kingdom.
8. Soremekun OA, Takayesu JK, Bohan SJ. Framework for analyzing wait times and other factors that impact patient satisfaction in the emergency department. J Emerg Med. 2011;41(6):686-692. doi:10.1016/j. jemermed.2011.01.018
9. InfoFinders. Leading Practices in Emergency Department Patient Experience. Ontario Hospital Association; 2010/2011. Accessed July 25, 2025. https://www.hqontario.ca/ Portals/0/modals/qi/en/processmap_pdfs/ resources_links/leading%20practices%20 in%20emergency%20department%20 patient%20experience%20from%20oha.pdf
10. Maister DH. Psychology of Waiting Lines. Harvard Business School; 1984.
Emergency medicine has never been just about outcomes—it is about experience in extremis. The waiting room is not ancillary to this mission. It is where first impressions form, where anxiety builds or abates, and where a system’s values become visible. As clinicians and administrators seek to improve patient-centered care, they would do well to remember that satisfaction is not always about speed. Often, it is about trust, clarity, and the perception of being seen.
11. Team V. Enhance patient satisfaction with wait times. Vital. Published 2025. Accessed July 25, 2025. https://vital.io/solutions/wait-times
12. Franklin BJ, Li KY, Somand DM, et al. Emergency department provider in triage: assessing site-specific rationale, operational feasibility, and financial impact. J Am Coll Emerg Physicians Open. 2021;2(3):e12450. doi:10.1002/emp2.12450
13. Sember M, Donley C, Eggleston M. Implementation of a Provider in Triage and Its Effect on Left without Being Seen Rate at a Community Trauma Center. Open Access Emerg Med. 2021;13:137-141. doi:10.2147/ OAEM.S296001
14. Davies J, Scholtes S, Oppenheimer J. Improving Wait Times at the Cambridge University Hospitals’ Accident & Emergency. Cambridge Judge Business School; 2017.
15. Moll van Charante EP, van Steenwijk-Opdam PC, Bindels PJ. Out-of-hours demand for GP care and emergency services: patients’ choices and referrals by general practitioners and ambulance services. BMC Fam Pract. 2007;8:46. doi:10.1186/1471-2296-8-46

Melissa Myers, MD FAAEM, Gary Bhagat, MD FAAEM, and Faith Kelly MD

oint of care ultrasound (POCUS) is an increasingly utilized tool in cardiac arrest resuscitation, both to look for reversible causes and for prognostication. It has become a part of the initial physical exam and an element of resuscitation in a way that is likely to increase in coming years. This shift towards its use is not without reason—POCUS allows us to evaluate for tamponade, right heart strain, and pneumothorax. All potentially reversible causes of cardiac arrest that can be easily and rapidly diagnosed with the aid of ultrasound. Yet, evidence shows that use of ultrasound increases the length of time for pulse checks, and some experts are concerned that the use of POCUS for prognostication may lead to early termination of codes. International guidelines fail to clarify the subject and recommend cautious use. Despite this, POCUS is becoming a standard practice during cardiac arrest. The “cat is out of the bag” on this one—we will continue to see ultrasound used during cardiac arrest. So, what are the safety concerns, and how can we incorporate this so that it benefits rather than harms our patients?
International guidelines show hesitancy overall, without strong recommendations for or against the use of POCUS. The 2020 American Heart Association Advanced Cardiac Life Support Guidelines comment only that there does not appear to be a benefit when used for prognostication, but note “this recommendation does not preclude the use of ultrasound to identify potentially reversible causes of cardiac arrest or detect ROSC.”1 The 2020 ILCOR Consensus Statement on Cardiopulmonary Resuscitation discusses a lack of strong studies, and recommends against the use of ultrasound until “high-certainty” evidence is obtained.2 I can’t argue with a lack of high quality evidence, but do feel obligated to note that there will likely never be high-certainty studies on this topic given the complexity of the arresting patient. We should instead evaluate the evidence we do have and apply sound clinical judgement along
with deliberate practice of POCUS use in a way similar to what we do with ACLS.
The primary safety concern with the use of POCUS is prolonged pulse checks. In 2018, Clattenburg et al found that POCUS use during cardiac arrest was associated with significant prolongation of pulse checks. They reported that pulse checks when POCUS was used had a median length of 17 seconds, significantly longer than the recommended 10 seconds. When the same person directed the resuscitation and performed the POCUS exam, this further increased the pulse check time. Interestingly, ultrasound fellowship trained faculty had shortened pulse check lengths at 13 seconds, suggesting that there are techniques that could be used to shorten pulse length when POCUS is used.3 The same authors then showed that the use of a standardized protocol, the Cardiac Arrest Sonographic Assessment (CASA) protocol decreased the pulse check duration.4 The pulse duration decreased three seconds overall, with the median check decreasing from 19 to 16 seconds. Still too long, but further decreases were again noted with ultrasound fellowship training.
Use of a standardized exam seems like both an evidence-based and intuitive method to decrease pulse check length. There are several other practical steps emergency physicians can take to use POCUS without causing harm.5 Gottlieb and Alerhand described these, recommending the following additional steps:
• Assign appropriate roles: Have the most experienced person do the scan, and avoid having the team leader performing POCUS

• Before stopping: find the window before compressions are stopped and only stop compressions if necessary for the cardiac view (perform other views with compressions ongoing)
• Clip your view: Record the clip, then look and analyze after compressions resume
POCUS offers obvious benefits during cardiac arrest to identify reversible causes, guide resuscitation, and potentially for prognostication. But it must be used responsibly…”
• Don’t forget your timing: Have someone timing your pulse/POCUS check and call out when 10 seconds have elapsed (one technique is to use the “beep” a machine emits when it reaches the end of a six second standard video clip)
• Endpoint: POCUS offers real-time information that can shape resuscitative efforts, but it should not be treated as a diagnostic endpoint. The presence—or absence—of cardiac activity may influence decisions about ongoing efforts, but definitions of “standstill” vary, and misinterpretation can lead to either premature termination or inappropriate continuation.
POCUS offers obvious benefits during cardiac arrest to identify reversible causes, guide resuscitation, and potentially for prognostication. But it must be used responsibly, and should not interfere with proven beneficial interventions, such as high-quality CPR.
Author note: The opinions and assertions expressed herein are those of the author(s) and do not reflect the official policy or position of the Uniformed Services University of the Health Sciences or the Department of Defense.
THE WHOLE PHYSICIAN
Continued from page 10
Dopamine explains, at least in part, why we love the chaos of the ED, and it explains some of why we feel so terrible after work sometimes. There is no shame in post-shift zombification, but post-shift self-care strategies will help us leave work at work so we can more fully engage in home life.
References
1. Bellieni C, et al. Impact of 24 h shifts on urinary catecholamine in emergency physicians: a cross-over randomized trial. [ResearchGate, 2014].
2. Åkerstedt T, Wright KP. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med Clin. 2009.
1. Merchant RM, Topjian AA, Panchal AR, et al. Part 1: Executive summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020;142(16_suppl_2):S337-S357.
2. Nolan JP, Berg RA, Andersen LW, et al. Executive summary: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2020;142(16_suppl_1):S2-S27.
3. Clattenburg EJ, Wroe PC, Brown S, et al. Point-of-care ultrasound use in patients with cardiac arrest is associated with prolonged cardiopulmonary resuscitation pauses: a prospective cohort study. Resuscitation 2018;122:65-68.
4. Clattenburg EJ, Wroe PC, Gardner K, et al. Implementation of the Cardiac Arrest Sonographic Assessment (CASA) protocol for patients with cardiac arrest is associated with shorter CPR pulse checks. Resuscitation. 2018;131:69-73.
5. Gottlieb M, Alerhand S. Managing cardiac arrest using ultrasound. Ann Emerg Med. 2023;81(5):532-542.
Dopamine is our friend. We need it. It fuels learning, motivation, and resilience. And it feels great! The challenge is to harness it without letting it hijack us.
For emergency physicians, understanding the dopamine roller-coaster isn’t just neuroscience trivia, it’s essential to our well-being and longevity in this demanding career. By balancing the
3. Wright KP, et al. Shiftwork-mediated disruptions of circadian rhythms and consequences. Nat Rev Endocrinol. 2013;9:507–516.
4. Killgore WDS. Stimulants in models of shift work and shift work disorder. In: Sleep Deprivation, Stimulant Medications, and Cognition. Cambridge University Press, 2012.
highs and lows, we can reclaim joy in both the drama of work and the quiet of life. And maybe most importantly, we can learn to recognize the “post-shift zombification” for what it really is: a temporary dopamine crash, not a permanent state. With the right strategies, we can come back to life, not just at work, but in the moments that matter most.
5. Reed AC, et al. Research shows human behavior guided by fast changes in dopamine levels. Wake Forest Univ Newsroom. 2023.
Steven Stefancic, MD FACEP FAAEM, Weston Childers, DO, Edwin Leap, MD FAAEM, and Cassandra Saltzer ARP CAP
The mantra of emergency medicine is “be prepared for the unexpected.” This mantra-mindset runs so deep that physicians establish and join specialized groups dedicated to preparing for the unexpected. Fields like prehospital care, wilderness medicine, event medicine, and disaster medicine have emerged from this commitment. These groups focus on unexpected events outside the hospital, but very few focus on internal disasters within our home away from home.
While undergoing a significant, mid-summer expansion project, the unexpected occurred at a regional, rural trauma center. When excavating around buried power lines, earth moving equipment completely severed the power supply to the hospital. An internal disaster was declared.
How the entire hospital team and community responded to this unexpected event was humbling as an emergency medicine physician.
In a situation briefing, staff learned the excavation incident resulted in a catastrophic power failure including both the primary and secondary power supply lines to the main campus hospital. Amazingly, no workers were injured. The facility was required to rely solely on backup generators, and quickly realized additional generators were needed to maintain normal operation in the summer climate.
Hospital disaster plans were enacted, with administration obtaining industrial generators to maintain normal function within hours. Nonclinical departments—including administration, human resources, and finance—played vital roles by providing logistical support to expedite critical tasks and ensure continuous hospital operations around the clock.
Following emergency inspection by engineers, the operating room HVAC was found to be compromised. All surgeries were rescheduled.
In a matter of hours, two mobile operative suites were quickly established in the
“As a physician, witnessing our hospital rise to meet the needs of the community was nothing short of remarkable.”

emergency department resuscitation bays (as one would see in MASH): one for emergent general surgical operations; one for emergent obstetrics procedures (Photograph 1). This occurred with no complaining while trains of equipment were shuffled to maintain readiness.
This resulting response by the hospital and the emergency department was tremendous. ED patient care sections were adjusted to meet the needs of the hospital in the event that a patient would need an emergency procedure. The ED and operative teams saw more of each other in this short time than anyone could remember.
Hospital directors ensured staffing was appropriate with units cared for appropriately, and EMS ensured prehospital patients were routed to appropriate facilities.
The hospital’s mechanical wing was repurposed for emergency power generation, while a refrigerated trailer was deployed on-site to store and prepare patient meals (Photograph 2). Our facility engineering team worked to ensure a temporary, appropriate power supply was available.
In the end, the power supply to the hospital was completely rebuilt within 48 hours by digging a 450 foot by 4 foot trench from the power source to the building. The construction trench is visualized in the center of the construction area (Photograph 2).
As a physician and community member whose family seeks care at this hospital, I was humbled to see how everyone came together in the wake of an internal disaster. A “thank you” is deserved to administration for coordinating a quick response, and to all the team who made the readiness happen. >>

Industrial generators can be visualized with a refrigeration unit for patient meals. A trench is visualized for repairing the power interruption.
THE NETTLE WITCH, MD
Continued from page 12
that served as a spade. The stone, the shape of a human heart, broke in two pieces in my hands. Were my hands that strong? Was my heart that fragile? As I sat by the water, I prayed. I prayed to Mary in her lightness and her darkness.
The river, which had timidly licked the bottoms of my boots on arrival, shoved forward, then back, thrusting around and through my thighs on my return. On the trail, my Wellington boots carried portable puddles, sliding in external mud puddles, into sharp, tangled arms of gorse and hawthorne. Deep red streaked across light blue shirt, a wool shirt that had merged with my skin. I peeled it away along with everything else until dry blanket and warm fire enveloped me. Cold, wet ropes of hair dripped water between my breasts. A handful of scarlet, navy blue, and so black they are purple berries, sweet and tart gently kissed my lips. Salty, heavy miso pushed my spirit back to earth.
I returned centered, connected to my desire, planning to slowly and gracefully make my exit from medicine. Back at home, the most danceable Disney songs rang out. My daughter’s rainbow skirt twirled around and around. I shook my hips and shimmied around the living room. I grabbed my daughter’s hands and swung her between my legs. My daughters and I celebrated my return from Wales.
An envelope on the island caught my eye.
The community typically thinks of a hospital in terms of its doctors and nurses, however there are many needed to make the organization function: administration, emergency staff, surgical teams, housekeeping, logistics, maintenance, human resources, dietary, engineering, and partners like Appalachian Power.
As a physician, witnessing our hospital rise to meet the needs of the community was nothing short of remarkable. A special thank-you goes to the many behind-the-scenes teams who work tirelessly to ensure our resources are ready for our families, friends, and neighbors.
This thanks also extends to the community members who brought food and snacks for patients and staff, your support speaks volumes. It truly takes a village to care for one another, and this week reminded us just how strong our village is.
Dear Dr. Walsh:
This letter is to inform you that a formal complaint has been filed against you with the Minnesota Board of Medical Practice. This letter does not make any claim as to the legitimacy of the complaint. In order for us to investigate…
I asked for a leave of absence because it seemed too drastic, too wild to quit altogether. My boss spoke to me about it.
“Just to be sure,” he said, “are you thinking about hurting yourself?”
I didn’t have the words to explain that putting on my scrubs and mask each day felt like self-harm. I didn’t have the words for how that mask, gown and gloves built a cage. My voice, my touch, my spirit were trapped inside, and no one out there could hear me anymore. How do you explain to someone that has done the same job that you needed something different than they did, that you stayed, but you should have run?
Editor’s Note: To read more of Dr. Walsh’s writing about healthcare and herbalism, please visit The Nettle Witch, MD at thenettlewitchmd.substack.com

Pallavi Malladi, MS4
Diaphragmatic breathing offers known benefits for chronic hypertension, but in the fast-paced emergency department (ED), its role during a hypertensive crisis is often questioned. Can a few deep breaths make a difference when blood pressure (BP) skyrockets? This article reviews the evidence and offers a “common sense” perspective for emergency physicians, acknowledging both conventional and complementary approaches.
Diaphragmatic breathing, or deep abdominal breathing, is a conscious technique derived from ancient yoga practices, characterized by the deliberate use of the diaphragm for prolonged, deep inhalations and exhalations. Different Pranayama methodologies, including alternate nostril breathing, humming bee breathing, cooling breathing, and ocean breathing, have been observed to elicit varied physiological responses in heart rate and BP. A meta-analysis by Gard et al. showed that breathing exercises can reduce SBP by 8-11mmHg and DBP by 3-6mmHg over time if performed consistently and for at least 4 to 12 weeks compared to control groups.1 Other studies show SBP reductions between 4-54mmHg and DBP reductions between 3-17mmHg.2 A study by Mitsungnern et al. found that 55 hypertensive urgency patients (and 55 controls), without acute complications requiring IV antihypertensives (no ACS, stroke, acute HF, ARF, AMS, cardiac arrhythmias, or pregnancy), significantly reduced systolic BP by 28mmHg and diastolic BP by 17mmHg within three hours using pursed-lip breathing (inhaling for two counts, exhaling for four counts while supine).3
Increased sympathetic activity in hypertensive patients, stemming from factors like altered baroreceptor sensitivity and increased pulmonary vascular pressure, is counteracted by slow, diaphragmatic breathing at just six breaths per minute, which engages the parasympathetic nervous system via vagal nerve stimulation.4 This reduces the heart rate by activating cardiopulmonary mechanoreceptors and leading to arteriolar dilation. Prolonged inhalations activate pulmonary afferents, leading to decreased thoracic pressure and pulmonary venous return, leading to decreased cardiac preload and a transient fall in BP. On the other hand, deep exhalations activate arterial baroreceptors, which then increase ventricular preload and, thus, increases BP. We can modulate our BP by changing the frequency of our inhalations and exhalations.
A hypertensive crisis, defined as SBP >180 or DBP >110—whether an urgency or a true emergency with target organ damage—is a vastly different clinical scenario. The clock is ticking, and the primary goal is
The goal is not to eliminate the use of antihypertensives altogether— instead, we should be aiming to mitigate hypertensive urgencies before they become emergencies”
rapid, controlled blood pressure reduction to prevent devastating outcomes such as stroke, encephalopathy, myocardial infarction, or acute renal failure.
The 2017 American College of Cardiology/American Heart Association (ACC/AHA) guidelines are unequivocal: hypertensive emergencies demand immediate pharmacological intervention, often with intravenous antihypertensive agents, to protect target organs.6 In a hypertensive emergency (signs of end-organ damage), immediate administration of appropriate antihypertensive medications according to established guidelines (CCBs, ACEI, ARBs, and hydralazine) is the standard of care and should not be delayed.
While diaphragmatic breathing and other mindful breathing techniques are valuable tools for long-term blood pressure control, stress reduction, and anxiety management, they are not a primary treatment for acute hypertensive emergencies in the ED per the ACC/AHA but may serve as a supportive measure to help calm an anxious patient while pharmacological interventions are being rapidly implemented. Device-guided slow breathing techniques can be added to treatment regimens to augment management of hypertensive urgency while awaiting and during pharmacotherapy, in addition to long-term care. The FDA has approved use of “RESPeRATE,” an over-the-counter electronic device that guides slowpaced breathing to achieve respiratory frequency <10 breaths per minute for stress reduction and as an adjunctive treatment to lower BP.5
Ultimately, while pharmacology remains our critical first response in the storm of a hypertensive crisis, guiding patients towards the sustainable well-being found ‘Beyond the Calm’ of the acute event often begins with empowering them to harness the simple, yet profound, power of their
References
1. Garg P, Mendiratta A, Banga A, Bucharles A, Victoria P, Kamaraj B, Qasba RK, Bansal V, Thimmapuram J, Pargament R, Kashyap R. Effect of breathing exercises on blood pressure and heart rate: A systematic review and meta-analysis. Int J Cardiol Cardiovasc Risk Prev. 2023 Dec 27;20:200232. doi: 10.1016/j.ijcrp.2023.200232. PMID: 38179185; PMCID: PMC10765252.
2. Herawati L, Hariyati RTS, Gayatri D. The Effect of Slow Deep Breathing on Blood Pressure in Hypertension: A Scoping Review. Open Access Macedonian Journal of Medical Sciences. 2023;11(F):229-236.
3. Mitsungnern T, Srimookda N, Imoun S, Wansupong S, Kotruchin P. The effect of pursed-lip breathing combined with number counting on blood pressure and heart rate in hypertensive urgency patients: A randomized controlled trial. J Clin Hypertens (Greenwich). 2021 Mar;23(3):672-679. doi: 10.1111/jch.14168. Epub 2021 Jan 7. PMID: 33410589; PMCID: PMC8029503.
Other references:
1. Ghati N, Killa AK, Sharma G, et al. A randomized trial of the immediate effect of bee-humming breathing exercise on blood pressure and heart rate variability in patients with essential hypertension. Explore (NY). 2021;17(4):312-319. doi:10.1016/j.explore.2020.03.009.
2. Elsheikh S, Elnahas N, Wahab Soliman A, Ismail A. Effect of Bhramari versus Sheetali pranayama on quality of life in hypertensive patients. Adv Rehabil. 2023;37(2):1-8. doi:10.5114/areh.2023.127506.
own breath. Other reasons to support use of diaphragmatic breathing exercises in the ED include its lack of cost, accessibility, and reduction of anxiety. Empowering patients with these self-management tools can foster sustained well-being beyond the acute event.
In summary, diaphragmatic breathing is beneficial for chronic hypertension management but should not replace immediate pharmacological interventions during hypertensive crises, as outlined by the 2017 ACC/AHA guidelines. However, it can definitely be used as an adjunct while the patient is receiving antihypertensives and can also be used in waiting periods prior to medication administration. The goal is not to eliminate the use of antihypertensives altogether—instead, we should be aiming to mitigate hypertensive urgencies before they become emergencies through a combination of approaches. Especially with the 2024 American Heart Associate guidelines that say asymptomatic elevations in BP can be discharged with close follow-up, it is imperative to set up patients with good skills that can be used to reduce BP in the interim alongside other lifestyle and medication regimens.6
4. Joseph CN, Porta C, Casucci G, et al. Slow Breathing Improves Arterial Baroreflex Sensitivity and Decreases Blood Pressure in Essential Hypertension. Hypertension (Dallas, Tex. : 1979). 2005;46(4):714-8. doi:10.1161/01.HYP.0000179581.68566.7d.
5. Cernes R, Zimlichman R. Role of Paced Breathing for Treatment of Hypertension. Current Hypertension Reports. 2017;19(6):45. doi:10.1007/ s11906-017-0742-1.
6. Whelton, Paul K., et al. “2017 ACC/AHA/AAPA/ABC/ACPM/AGS/ APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.” Journal of the American College of Cardiology 71.19 (2018): e127-e248
7. Bress, Adam P., et al. “The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association.” Hypertension 81.8 (2024): e94-e106.
3. Kuppusamy M, Kamaldeen D, Pitani R, Amaldas J, Shanmugam P. Effects of Bhramari Pranayama on health – A systematic review. J Tradit Complement Med. 2017;8(1):11-16. doi:10.1016/j.jtcme.2017.02.003.
4. Mittal, Gauri, et al. “An Exploratory Randomised Trial to Assess the Effect of Nadi Shodhan Pranayama as an Adjunct Versus Standard Non-pharmacological Management in Hypertensives.” Annals of Neurosciences (2025): 09727531251318810.

Kristen Hancock, MD
It’s 2:15am, and a loud noise blares from my nightstand. I reach over, groggy and disoriented, trying to figure out whether it’s my pager—since I’m on ortho call—or my phone alarm, reminding me it’s time to check on my three-month-old and pump. At this point, does it even matter? I had just managed two consecutive hours of sleep—a rare gift—only to be reminded of one of my earliest lessons as both a new mom and a brandnew second-year resident: sleep is a luxury I was not yet able to afford.
When I found out I was pregnant during residency, I knew it would be challenging. However, as a non-traditional student who started medical school in my late 20s, I also felt that time was not on my side. I was told that there is never a good time to have a child in medicine, so I didn’t give much thought to waiting until after the completion of residency to start a family. Additionally, by this early stage in my career, I had already met several women in medicine who had delayed starting their families for the sake of training, only to later face heartbreak when they were unable to grow their families as they had once hoped—for reasons beyond their control. There was the brilliant intensivist who had her first child at the completion of fellowship and hoped to have a second, however by this time, she was 41 years old and had not conceived after two consecutive years of trying. Then there was the successful cardiologist, thriving in her field with a busy small group practice and a months-long waitlist who was approaching her late 30s and just now seriously entering the dating scene. Her advice to me: “Medicine will always be here. Care for yourself, your family, and the moments you can’t get back—because those are what truly matter.”
every two to three hours felt less like a recommendation and more like a fantasy. I struggled to maintain my milk supply, and by the end of my rotation, it was nearly gone. If only I followed the advice I was given by the perspicacious cardiologist. There were days I cried in the call room while trying to pump, hoping a med code was not called, or in the stairwell on my way to see a new consult during my cardiology rotation, feeling like I was failing at both motherhood and medicine.
[T]o the programs training the next generation of doctors—let’s make room for those of us building both a career and a family. We are not asking for easy. We’re asking for possible.”
My residency leadership team and chief residents were, thankfully, supportive. They checked in, gave me the space to speak up when I needed help, though I rarely ever asked and instead tried to figure everything out on my own. They made genuine efforts to support my needs—giving me some holidays off or scheduling me for swing/night shifts when they knew daycare would be closed and daytime child care would be a challenge. They also arranged lighter rotations following my seven week maternity leave after a C-section, postponing the more demanding ones until later in my second year. I was encouraged to take the time I needed to step away and pump. But there are always those who trained “back in the day,” when asking for time to pump was unthinkable and calling out for a sick child was seen as weak or unprofessional. Or those attendings and residents on off-service rotations, particularly surgery subspecialties, that didn’t have to say much— but just a look or a passing comment was enough to make me feel like I was somehow letting the team down.
There was a lingering fear lurking in my subconscious about whether I would be able to handle the rigors of training, the exhaustion of pregnancy, and the never ending job of motherhood, yet there was something simultaneously propelling my husband and I to move forward with expanding our family. I don’t think I fully appreciated just how deeply my roles as an emergency medicine resident and mother would clash. I was warned about the sleep deprivation parents experience with a newborn, however I arrogantly thought, “I’m a resident. I’m already sleep deprived. This will be a piece of cake.” Oh, how I was quickly humbled. During the more grueling rotations, like MICU, ortho, and trauma surgery, pumping
I often found myself torn between two worlds that demanded everything from me. Medicine taught me to sacrifice, to push through, to be there no matter what. Motherhood, on the other hand, was teaching me to be present, gentle, and patient—especially with myself. It’s a constant, imperfect balancing act.
But here’s the thing: I’m not the only one. More and more residents are choosing to start families during training. And while the challenges are real, the support systems we build within our programs, departments, and among each other can make all the difference.
So how can we better support resident parents?
Normalize parenthood in medicine. The more we talk openly about parenting during residency, the less isolated new parents will feel. When senior residents or attendings share their own parenting stories, it helps break the silence and stigma.
Build pumping-friendly environments into the culture. Lactation support isn’t a luxury—it’s a basic need. Programs should proactively provide clean, accessible pumping spaces and ensure protected time is built into the daily workflow, so residents don’t have to ask or feel guilty. For instance, after three consecutive hours of work, residents should be encouraged to step away for 20 minutes to pump, with attendings or co-residents temporarily covering their responsibilities. During my EM and pediatric EM rotations, a few attendings—often women—would check in at the start of a shift to ask if I was still pumping and offer to hold the phone while I stepped away. That simple gesture meant everything. It removed the burden of asking for permission and made me feel supported as both a parent and a physician.
Offer meaningful schedule flexibility. Flexibility is a powerful sign of trust and respect. It can take many forms: arranging lighter rotations postpartum, easing shift swaps for pediatrician visits or sick days, or adapting schedules during pregnancy. One of the most supportive policies in my program was eliminating overnight shifts for pregnant residents in their third trimester. I took on more swing shifts instead, which felt completely manageable—and deeply appreciated. Even more heartening, other residents understood they might take on an extra night shift that month, and many volunteered without hesitation. That kind of community mindset makes all the difference.
Furthermore, how can new parents in residency support and advocate for themselves?
Know Your Rights and Policies. Understand parental leave policies at your institution and from the ACGME. Ask for clarity on pumping accommodations, rotation scheduling flexibility, and any family leave policies. Keep documentation of communications and agreements in case of leadership or administrative changes.
Communicate early and clearly. Let your program leadership know your needs as early as possible, whether it’s maternity/paternity leave, postpartum support, or childcare logistics. Be proactive in suggesting solutions (e.g., proposing specific schedule adjustments) to make it easier for the program to say yes.
Build your village. Identify supportive attendings, co-residents, and staff who can advocate with you or for you when needed. Join or create a resident parent group—even an informal group chat can offer emotional support, practical tips, and shift swaps in a pinch. Connect with faculty or senior residents who have been through it for mentorship and guidance
To anyone walking this same path: You are not alone. You can be a compassionate physician and a present parent.”
Train attendings and senior staff on family-inclusive leadership. Sometimes, the negative feedback comes from those who simply don’t know better, or have not had a similar experience. Programs can offer brief workshops or discussions on supporting resident parents, helping to bridge generational gaps.
Build a buddy system or parenting affinity group. Having a peer who truly understands the unique challenges of parenting during residency is invaluable. Whether it’s someone who doesn’t blink an eye when you mention being up five times overnight or needing to change your scrubs after a diaper blowout, that sense of shared experience provides comfort and solidarity. While my hospital has several active affinity groups, none were focused on parenting—a gap that, if addressed, could offer meaningful connection and support for resident parents.
Protect your basic needs. Be assertive about pumping breaks, postpartum health, and childcare needs. Schedule time for medical appointments for your child and yourself—your health is just as important as your training. Speak up if expectations are becoming unsustainable
GIVE YOURSELF GRACE! Know that you won’t be perfect in either role every day—and that’s okay. Set realistic expectations and prioritize what matters most in the moment—some days it’s your child, others it’s your patients. Don’t be afraid to ask for help
Despite everything, I wouldn’t change my decision to become a parent during residency. My son gave me a renewed sense of purpose, a sharper focus, and a reason to protect my time and boundaries. He reminded me why empathy, patience, and balance matter—not just in my personal life, but in my professional one too.
To anyone walking this same path: You are not alone. You can be a compassionate physician and a present parent. And to the programs training the next generation of doctors—let’s make room for those of us building both a career and a family. We are not asking for easy. We’re asking for possible.
Parting advice:
There will never be a perfect time to start a family, especially in medicine. Don’t wait for the stars to align — wait for your heart to feel ready. Medicine will always be here, but your moments to grow a family are precious and fleeting. It’s okay to hit pause on your career; it doesn’t make you less of a doctor—it makes you whole as a person.

Jack Allan, MD MBA FAAEM
Physician burnout has seen improvements in the last few years, with survey data from the American Medical Association showing improvement in the burnout rate from 48.2% in 2023 to 43.2% in 2024. However, emergency medicine remains at the top of the list for medical specialties with the highest job stress, maintaining the top spot for career burnout in the same survey. The data shows that 51.1% of emergency medicine physicians are experiencing at least one symptom of career burnout. With over half of the emergency medicine physician workforce experiencing burnout, as early career attendings, it is imperative that we invest early in our ourselves to ensure we maintain the job satisfaction that allows for career longevity. This investment starts as more work but grows into a diversification of job roles. The decisions made right out of residency can heavily impact the future of our careers.
For me, the most significant of these decisions was to pursue fellowship training with advanced education. I entered an Emergency Medicine Administrative Fellowship directly out of residency, coupled with enrollment into a Master’s in Business Administration program. While the added responsibilities of the fellowship and time commitment of the night classes were certainly demanding, the outcome has been rewarding. The investment in myself has resulted in advanced knowledge of healthcare systems, proving useful in my ability to perform on my department’s clinical operations team. My degree concentration in health sector management brought me insight into hospital-wide operations, allowing me to successfully navigate various hospital-level clinical committees. Beyond these system roles, as a physician in an academic health system, my skillset allows me to flex into additional roles within the residency education program. As a faculty member with particular interest in departmental and hospital administration content, I can be a key residency educator in these areas. In the few years since I finished residency, I have quickly
transitioned my career into being not just a clinician, but a key player in our department’s operations, a hospital committee chair, and a core faculty member for resident education—each role bringing job satisfaction in different ways.
However, I will note that although my fellowship experience has shaped my early career and will guide my future career, fellowship training is not the only avenue to this career diversification. While the mentorship offered by my fellowship director aided my engagement within my own health system, mentorship can be instrumental even in a less formal format. Seeking out mentorship opportunities in any form can lead to novel roles. Many academic health systems associated with graduate or undergraduate degree programs offer reduced admissions for master’s programs or even ad hoc courses, making additional opportunities for advanced education more feasible. Even if not working within a health system with such access, enrolling in courses through national organizations can create avenues into career niches and offer significant networking opportunities.
I have done many of these steps to build a diverse career but continue to seek new roles. While we all sought out a career in emergency medicine, we must protect ourselves from the burnout inherent to our specialty. Putting in the work early, will pay off in the long run.

In the few years since I finished residency, I have quickly transitioned my career into being not just a clinician, but a key player in our department’s operations, a hospital committee chair, and a core faculty member for resident education—each role bringing job satisfaction in different ways.”
References
1. Berg, S. (2025, May 13). Which physician specialties are seeing a drop in burnout? American Medical Association. https://www.ama-assn.org/practice-management/physician-health/whichphysician-specialties-are-seeing-drop-burnout#:~:text=In%202024%2C%2043.2%25%20of%20 physicians,%25%E2%80%94down%20from%2056.5%25.
Mel Ebeling, MD

It is a quiet Sunday morning. Bright white light streams into my living room through the small cracks in the window shades. I have plopped down into the recliner, ripped open the latch to the footrest. My tachycardia from last night’s shift in the emergency department finally begins to resolve. I just finished my first month of residency.
I reflect on the three expectations set by my program director 30 days ago:
1. Work hard
2. Take care of each other
3. Maintain a positive attitude.
On day one, those expectations were much more reasonable, much more simple, than what I initially thought was going to be placed on me at the time; I had feared and anticipated perfection. However, like with many things in life, simple does not necessarily mean easy. In trying to meet these expectations while shadowed in self-doubt, I soon grappled with having the confidence to believe that my efforts were meaningful, even when consistently imperfect. I struggled to stay positive when I felt like a fraud, an imposter, like my sharpest days were long past.
A month later, I still feel like molasses in the department. I am only a handful of shifts into a career of thousands. I have so much to learn, and with only 47 months left to do it. I still look up antibiotic regimens that I should know by now. And contemplate imaging workups that are probably straightforward. And fumble around the supply closet for the right I&D equipment. And write lackluster MDMs. These things (I hope) will come with experience and dedicated study. Though, I can say that I have walked away from this month having learned the following:
I am only a handful of shifts into a career of thousands. I have so much to learn, and with only 47 months left to do it.”
There is value in taking a moment, though not more than a couple of minutes, to read about a hemodynamically stable patient before going into the room. The complexity of the patient’s past medical history can rarely be relayed adequately during the patient interview, and often, having that information advises a better next step. Antibiotic sensitivities, medication regimens, complex surgical procedures, and time-stamped timelines, for example, provide critical insights into the patient’s history of present illness and overall presentation. While this chart review may seem to impair efficiency on the front end, the information gathered there will likely facilitate a more sophisticated conversation with the patient, preventing trips back to the patient’s room for multiple clarifying questions and saving time. As someone who initially preferred seeing patients blind, I have quickly learned how a pre-interview chart review makes all the difference in efficiency.
A covered body part is masking an important exam finding until proven otherwise. Grabbing a hospital gown and spending extra time helping the patient undress and redress into a gown is not sexy, and it will impact workflow, but it is absolutely critical for the diagnosis and disposition of the patient.
We are grateful to live in an age with an ever-growing supply of clinical decision-making tools and pathways that help us determine patients’ risk for various diagnoses, whether exposing patients to ionizing radiation for images is necessary or worthwhile, etc. These tools were developed to attempt to help us to do right by the patient in the emergency setting, and in some cases, help us do right by the logistical constraints of an emergency department as well. Many are worth committing to memory, many more are worth having electronic access to. Still, they are not perfect and are ultimately not a substitute for clinical judgment. If your clinical reasoning leads you to believe that a particular case is going to keep you up at night, err on the side of being liberal with one’s assessment and work-up. This is part of the art of medicine.
Jake Moore, MS OMS-IV

When private equity enters a healthcare market, it is not good news for patients or the physicians who take care of them.
In 2019, Hahnemann University Hospital in Philadelphia closed its doors not even two years after being acquired by a private equity firm. This closure deprived one of our country’s poorest cities of what had been one of its key safety net hospitals and sent 500 trainees scrambling to find new residency programs, marking my first exposure to the corporate practice of medicine. At that time, I was just a pre-medical student scribing at the county hospital in San Antonio. I was shocked by the news. What would this mean for my community if it happened to our hospital, our residents, and our patients?
Now, one pandemic and six years later, nearly 80% of US physicians are employees. Private equity acquisition of hospitals and medical practices has continued. At least six private equity-owned hospitals have announced or completed closing their doors so far this year: Pennsylvania’s Sharon Regional, Colorado’s Johnstown Heights Behavioral Health, Illinois’ Kindred Sycamore, and Florida’s Rockledge Hospital, Kindred Lakeshore, and Kindred Tampa.1 Even when private equity-owned hospitals remain open, studies have demonstrated that they suffer cuts in staffing and services,2 worsening patient care outcomes,3 and decreased accessibility of healthcare, especially to patients in rural and underserved areas.2
This issue was part of what motivated me to join AAEM/RSA as a second-year medical student two years ago. As I got more involved and realized the scope of AAEM’s advocacy in the fight for patient care and physician autonomy in the face of corporate medicine, I felt proud to be a part of this organization. Seeing the work done by members like Mitch Li, MD FAAEM and Vicki Norton, MD FAAEM, AAEM President-Elect on this issue, I was inspired to take up the fight personally.
It didn’t take long for this inspiration to manifest as action. As my medical school’s SGA President, I had the privilege of serving as a student delegate at the American Osteopathic Association’s House of Delegates. That experience taught me that a well-researched, well-stated, common sense proposal can achieve broad support among reasonable clinicians. With this in mind, I set out to bring the fight against the corporate practice of medicine to the AOA and win some allies to the cause.
I spent the next year and a half seeking guidance from my mentors, working on a resolution draft, and trying to find sponsors to help me bring it to the AOA. The research and writing turned out to be surprisingly simple compared to navigating the process beyond that. I tried bringing my draft to state osteopathic societies, but deadlines, red tape, and concerns about fine-tuning key language proved insurmountable. I eventually won the support of the AOA’s Bureau of Emerging Leaders, who let me bring my draft to their resolution work group. Together we finessed the language and resolved statements over the course of a few meetings.
After months of patience and persistence, our draft found its way to the AOA House of Delegates this summer as Resolution H-633, “Protecting Patient Care: Opposing the Growing Impact of Private Equity and the Corporate Practice of Medicine.” I walked into the House reference committee meeting ready to advocate fiercely for this policy, but found it surprisingly uncontroversial. A few friendly amendments were offered that actually strengthened the resolution, and on Saturday, July 19, 2025, it was adopted by the AOA House of Delegates, making it the AOA’s official policy that:
“To protect patient care, access, and the patient physician relationship, the AOA supports legislative efforts that limit and regulate the corporate practice of medicine, including acquisition of medical practices, hospitals, and other such institutions by private equity firms and publicly traded companies entering healthcare for profit.” >>
After
months of patience and persistence, our draft found its way to the AOA House of Delegates this summer as Resolution H-633, ‘Protecting Patient Care: Opposing the Growing Impact of Private Equity and the Corporate Practice of Medicine.”
By adopting this resolution, the AOA has committed to supporting legislation to limit and regulate private equity acquisitions. This might include bills such as Senator Warren’s Corporate Crimes Against Health Care Act, which if reintroduced and passed would establish criminal violations, civil penalties, and other regulations on common private equity business practices in healthcare.
The fight against the corporate practice of medicine is one of AAEM’s key advocacy issues, and it’s a fight we can’t win alone. Now, as of this summer, we have allies at the AOA.
AAEM/RSA EDITOR’S MESSAGE
Continued from page 27
The transition from medical student to resident necessitates the learning of several new resources, even more if in a new hospital system. You must learn the wider hospital resources: which services are available in-house for consultation, where may patients be referred after discharge, etc. You must also learn your department’s resources: what services are available in the emergency department for assistance with patient treatment and disposition (e.g., pharmacy and social work), when are those resources staffed (e.g., 24/7?), how is communication initiated with them, etc. Then, there are also specialty-specific resources that
1. Private Equity Stakeholder Project (PESP). (2025). PESP Private Equity Hospital Tracker. https://pestakeholder.org/private-equity-hospital-tracker/
2. Brownstein, M. (2024). Private equity’s appetite for hospitals may put patients at risk. https://hsph.harvard.edu/news/private-equitys-appetitefor-hospitals-may-put-patients-at-risk/
3. Kannan, S., Bruch, J. D., & Song, Z. (2023). Changes in Hospital Adverse Events and Patient Outcomes Associated With Private Equity Acquisition. JAMA, 330(24), 2365. https://doi.org/10.1001/jama.2023.23147
must be learned—for example, WikiEM or CorePendium—that can be utilized to assist in formulating assessments and plans. Ancillary resources necessary during residency include those related to being an employee and taking care of one’s physical and mental health. Acquainting oneself with the minutiae of these resources is one of the more challenging and disorienting endeavors of intern year, yet one of the most important. Knowing your toolkit, how to navigate the system (as frustrating as it can be sometimes), is necessary to provide the best care to patients.
Having the mental fortitude to progress through residency requires the dispense of grace. Admittedly, I am still working on learning this one. I probably always will be. You are going to screw up, sometimes too frequent for comfort. For each patient you care for early on, you may have more questions than you ever had answers. And that is okay, at least for right now, at least that is what I tell myself. Growth comes over time. Cracks are slowly filled in. I think I suck less on day 30 than I did on day one.
Here’s to month two.

Tiffany Cagides, Medical Student
When I started medical school, I assumed research would be part of the path. I thought there would be a class, a checklist, maybe even a mentor to walk me through how to write a case report, navigate the IRB process, or understand what makes a good abstract. Instead, I found myself in the same place many students do—entirely on my own.
At my school, like many others, we focus heavily on clinical skills and board prep, but research is not something that’s built into the curriculum. It is something we are expected to “figure out,” usually without much support. For me, that meant a lot of trial and error, hours of watching YouTube videos made by other med students, and feeling like I was always two steps behind everyone else.
It did not help that many of the students I saw thriving in research already seemed to have some structure around them—things like home EM programs, built-in mentorship, or prior research experience. As a first-generation Cuban-American student at an offshore school, I did not have that kind of access. I did not even know what I did not know.
That changed when I reached out to a physician and shared how much I wanted to get involved in academic EM, but did not know where to start. He told me something simple that I will never forget: “You do not have to wait for someone to hand you a project. Start by writing up a case.”
It felt like a light switched on. I did not have a research mentor or a structured program, but I did have a case. And I was willing to put in the work.
I began by reviewing case reports and case series to gain an understanding of what made them effective. I also compiled a calendar of all the upcoming EM events hosted by organizations like AAEM and ACEP, along with their respective abstract submission deadlines. One of the conferences had a deadline just a few days away, and the physician I had spoken with encouraged me to go for it. If an abstract got accepted, I would figure out the rest later, and so I did. I had no idea if I was doing it “right,” but I kept going. Eventually, I submitted my first abstract and was accepted for my first poster presentation.

That one small win completely shifted how I saw research. I realized that even without formal training or significant institutional backing, students like me can still contribute meaningful academic work. However, we should not have to figure it out on our own.
If I could design a more accessible research pathway for medical students interested in EM, it would be simple but structured:
• A virtual research bootcamp that covers the basics—how to write a case report, submit an abstract, or get through an IRB.
• A shared database of open projects, including literature reviews and survey studies, where students can get involved early on.
• And most importantly, monthly office hours with residents or faculty who are willing to guide students through the process, answer questions, and help them stay on track until they have a finished project in hand.
Emergency medicine attracts students who are curious, adaptable, and eager to think critically about complex problems. These are the same qualities that make great researchers. But unless we create space for students—especially those without home EM programs or strong academic support—we risk missing out on a massive pool of talent.
He told me something simple that I will never forget: ‘You do not have to wait for someone to hand you a project. Start by writing up a case.’ It felt like a light switched on.”
I am still learning. I am still cold-emailing attendings and still figuring out how to read a Kaplan-Meier curve without having to Google it every time. But I now know that research is not just for the students who start early or have perfect credentials. It is for anyone willing to learn, take initiative, and ask for help.
So, if you are a student who feels behind or unsure where to start, this is your sign: start with a case. And if you are a resident or attending, know that your mentorship—no matter how informal—could make all the difference for someone like me.
your image acquisition was and other points on how you interpreted your image. Similarly for the procedures, there will be an assessment point on whether you successfully completed the procedure. Did you get the airway? Did you get the joint space fluid? And those may be broken down a little bit further into categories. Overall, an emergency physician who’s trained in procedural competency knows when a resident is competent and comfortable and talented in doing a procedure and knows when they need a little more work.

The second part of the clinical decision-making cases is a prioritization case. And boy, talk about mirroring real life. This should be an exact replica of when you walk into a shift and there are five or six new patients to see. And you, as the senior resident, must decide which of those patients you’re going to see in, in what order, and why. Which of those patients need a stabilizing procedure done right away? So that’s the prioritization type of cases.
MU: It sounds like not only is it just the actual outcome but also the methodology of whether you know the actual techniques. As the new exam is rolling out, how does ABEM plan to monitor the effectiveness of these changes and ensure quality? How does ABEM plan to re-evaluate the exam if these changes do not yield the expected or anticipated results?
DG: Those are great questions. And some of them really get into the psychometrics of the exam. We want to make sure that if you’re looking at a cohort of candidates, that each one of them, if they have a strength in clinical decision-making, that we see that strength carry through all their assessments. If they have a strength in communication, that carries through all their communication cases. So, we are looking at internal benchmarking within one candidate, but we are also looking at benchmarking over one single exam administration within evaluators. How do we make sure that there’s no bias put in the exam? How do we recognize those biases and how do we mitigate them? And that’s when we’re planning on having a subset of examinations that are scored by multiple different individuals. So that we can look at inter-rater reliability and make sure that that’s accurate. We are doing everything that we can internally to make sure that bias does not play a role in candidates’ exam scores.

And finally, the third set of cases are communication cases. You will have a patient-centered communication case. How do you work with that patient to get to an outcome that both you as the physician and the patient can agree on and how do you assure that the patient is going to have success in that pathway that you both determined? How do you explain a diagnosis or discuss diagnostic uncertainty? There will be a ‘difficult conversation’ station, such as delivering bad news like an unexpected loss in the emergency department. This ability to deliver bad news in a clinical setting is a fundamental skill that ABEM expects graduating residents to be able to handle. You also will get a ‘managing conflict’ case. As an EM physician, you have to manage a lot of conflict. We manage conflict with our patients when they don’t agree with the treatment plan. We manage conflict with consultants and with colleagues and with nurses and the list goes on and on. So how do you negotiate? How do you come to the best outcome? Lastly, every candidate will get a reassessment case where either it is a patient that returns to the emergency department or somebody that is partway through their workup and has an unexpected turn. Something happens that the patient decompensates into an unexpected outcome. And how do the candidates identify that? How do they adjust to that situation? And how do they explain it to the patient?
MU: We’ve already discussed a bit about the different structure of this new exam, but how else does the new certification exam differ from previous versions in terms of structure, content, and the overall format?
DG: There are three distinct elements of the new certifying exam. The procedure part that we already talked about, both the kinesthetic procedures and the hands-on procedures that you’re going to do in the ultrasound, that’s one component. There is still a clinical decision-making component, which is like a tabletop exercise where you as a candidate are going to be sitting across from two ABEM examiners. One of them is like the structured interview case where you’re given a case and asked to talk through it. For example, what pertinent information would you gather from the patient, both historically and in a physical exam? Let’s delve into a differential diagnosis and talk about diagnostic studies. Tell us what management steps you may want to do. Again, very similar to when you present patients to your attending physician. The exact same way that you would present them with some kind of guideposts in there to demonstrate you know what to consider and why to consider it. For example, you decided to order a chest X-ray on this patient but elaborate on what you are looking for in the chest X-ray.
MU: That ability to reassess and pivot is a critical skill all EM physicians should be proficient at. It is the ability to realize and recognize when a critical change occurs in a patient that was signed out to you—one that you weren’t primarily taking care of nor primarily worked up. These communications cases with the difficult conversations, managing conflicts, and the reassessments, are these new topics that are being emphasized in this upcoming exam compared to the prior exam?
DG: All the communication cases are new. We’ve always had a portion of the oral exam or the virtual oral exam that’s focused on a simulated conversation between you and a patient or a patient’s family. But this is where you’re going to have a standardized patient in the room with you and you’re going to be delivering that bad news to them in real time. Or they are playing the role of a consultant and you’re going to be managing conflict with them and showcasing how you negotiate and work collaboratively.

MU: Are there other new topics or competencies being emphasized
While a lot of it is communication, some of it is also social determi nants of health and understanding what those limitations may have on the success of patient care. We are really trying to much more holistically look at all the competencies that are needed to practice emergency med icine. And those are not just diagnostic and management competencies. Those are all management with a capital ‘M’ as opposed to a small ‘m’. It’s more than what crystalloid you’re going to give. It’s how you are going to ensure the success of the plan that you’ve come up with.
MU: I’ve heard some conversations amongst the EM community regarding concerns about declining pass rates over the years even though the current exam was shown to not be getting more difficult. Has that been part of the motivation for the new changes? Is there any other insight you can provide into this?
DG: There was not one singular element that prompted this change. It was a conglomeration of opinions that ABEM really sought out about the oral exam. What is the whole process of certification? What does it look like? What are the strengths and weaknesses of certification? What are the opportunities? What areas do we need to lean into that we haven’t leaned into before? ABEM talked to over 4,000 individuals about this through surveys and focus groups. We had a summit. We talked to so many different stakeholders. We talked to the public. We talked to residents. We talked to academic chairs. We talked to contract management groups. We talked to program directors. We talked to every major national emergency medicine organization. We drew together the idea that certification is necessary. We want to maintain really high standards, but we’re not doing enough with the increased number of training programs, with the increased number of candidates coming into the process, with the increased demand for emergency physicians and the scope of practice of emergency medicine. It’s not that you’re with a patient for 20 minutes anymore. It’s that you’re with a patient for, in many cases, hours, if not days, managing their care. And we just weren’t doing enough to replicate that environment in a certification process.
MU: When was the last time that the board exam was reviewed or updated?
DG: Every year the exam gets reviewed and updated. And when you mentioned concerns for pass rates, let me lean into that a little bit. We are not looking for this exam to significantly change pass rates. We’re not looking to raise or lower a bar. We’re looking to maintain excellence. And the definition of excellence for emergency medicine and for ABEM has always been that the passing score for any test is what’s called criterion referenced. So we are not looking for X percentage of passage or X percentage of failures. Nothing is graded on a curve that way. Instead, we take the content material from the exam that is given and we gather together a group of experts in the field. And experts are practicing emergency physicians across the nation. And we ask them, “What would you expect the definition of competency should be? What should a colleague
that you are now working side by side with be expected to do in talking to a patient? Is it delivering bad news, in managing conflict, in doing an ultrasound and interpreting those results, in prioritizing a track board that has eight new patients on it? What is that definition of competency?”


That’s where the passing score is set, from physicians working in the pit. Coming up against these challenges on a day-to-day basis, what do they consider as competency? And that’s where we set the passing score.
MU: It’s reassuring to hear and feel like these changes were some thing that the entire community was pushing for. What has been the initial feedback whether that’s been from candidates themselves, from actual residency program directors, or other stakeholders?

Well, change is hard, Mary, I’ll tell you that. Change is hard no matter what the change is. There were very logistical and pragmatic concerns that the test was going to be in Raleigh, North Carolina, which is not centrally located in the United States. There are pragmatic and lo gistical concerns that Raleigh is a little bit more difficult to get to for some candidates. There are concerns that we are moving from a virtual examination where you can take it truly in your scrubs or your pajamas in your bedroom to an in-person exam and the costs associated with that. Those were the initial concerns that we had from candidates. Now, as we have published more information with lots of videos and granular information on the website, we are starting to hear more concern from program directors regarding how to best prepare their residents. I believe we have been really transparent in saying these are the criteria that we’re using. We’ve listed the citations and references that we’re drawing from to really tell us what best practices are. And there’s a list with every case type that states what a competent candidate will be able to do and what we’re going to be looking for in the examination. As I said, change is hard. But when people dive into the information that’s been provided, I think they will gain a lot of comfort from seeing the volume of information and support provided and how transparent it all is.
MU: As a resident myself—of course there’s nervousness regarding the new exam. I think that happens with any sort of exam in any field. However, when I consider this perspective of aiming to maintain excellence in our standards and ensuring that graduating residents are competent in providing astute evidence-based care, these changes seem fitting. Since we are going to be assessed on skills that any board-certified emergency physician should be able to perform, then it makes sense to return to an in-person format because how much can you truly showcase your knowledge and be accurately evaluated through a virtual format. As you were going through this process of revamping the exam, were residents or the educators consulted during the development of these updates or was it only during the initial process? And if they were consulted, how was their input integrated? For example, was there any beta testing or anything like that?
DG: We’re at the stage now that our first beta test occurred this past spring. We will have another couple of beta tests before the exam goes
live in 2026. Residents and resident organizations, as well as program directors and the Council of Residency Directors (CORD) have been consulted. We have a direct pipeline to them. We have talked to RSA, we’ve talked to EMRA, not only in the development phase, but also in the announcements and the rolling out of all this. And we’ve asked them what more information can we provide? Short of giving you the answers, we want to make you comfortable with the procedures and the practical aspects of the exam such as where you’re going to have a hotel, how do you get connected with the exam, where do you go at what point, what do you wear. For all those kinds of things, we are really trying to get as much information out to the community. That’s another reason why I really appreciate the opportunity to talk to you today because this is one other avenue that we can use to reach out to our community.
MU: I agree. This opportunity to interview you has been invaluable. I am a huge proponent for trying to foster collaboration among multiple groups to ensure that everyone has a fair understanding of what’s going on and what is expected. ABEM is doing their best regarding transparency with this new exam and I’ve appreciated that. You mentioned references and resources that ABEM utilized. Given educators are asking how to best prepare their residents, are these new revised resources available for them and candidates?
DG: It’s all on the website. It’s all the references and citations that we used as guiding principles. They’re all on the website for program directors and candidates alike.

MU: And what advice do you have for candidates who are trying to prepare for the updated certification process?
DG: That’s a great question. And the bottom line is to keep in mind that the standard that we’re setting for this is the standard that is being practiced in emergency medicine right now. So lean into the standards that you have at your fingertips. Lean into your attendings. When you go to deliver bad news, make sure that there’s an attending with you. When you’re having a difficult conversation with a consultant who doesn’t want to see your patient, have your attending critique your performance on that. When you’re going in to see a patient you anticipate may have a difficult disposition, ask the faculty how they would tackle it and what tools would they use to facilitate the best outcome. Have faculty watch you do procedures. Have faculty critique you on your ultrasounds. If you are engaged with your teaching faculty and residency, this is what you are doing on a day-to-day basis. You’re presenting patients. Your faculty should be able to tell you what you’re doing well in the clinical setting and tell you the areas that you need to improve in. And that’s all you need to do.
ultrasound skills, lean into that, ask for more feedback, ask for more practice, ask for more observation of those. If you don’t feel comfortable in your your reassessment skills or your conflict management skills, or if your faculty aren’t routinely looking at your thought process as you go through a tracking board and decide which patients to see first, just ask for that feedback. This is what we do as faculty. This is what we do as attending physicians. And we should be able to convey to you easily what elements you should have confidence in because you’re doing great in them and some areas of opportunity to work on.
MU: Are there challenges that you or the ABEM board is anticipating candidates might face during the new process? And if so, how are you planning to address those?
DG: I think that most of it is going to be a comfort issue. I’m not as concerned about the logistics or the pragmatic aspect of it. And that first group that goes through are going to be the pioneers. So I look at it as an adventure that way. I believe once that first group goes through and the emergency medicine community at large realizes that this is not a ‘gotcha’ moment, that it is just a replication of what we do every day, then a lot of those difficulties are going to go away. We have really tried to do what we call locally “red teaming.” We’ve tried to understand if there may be travel difficulties or potential unforeseen circumstances with a candidate and simulate how we would adjust. What if a candidate comes in with an identified disability? How do we adjust for those in the training process? We’ve really tried to red team the entire process so that nothing unexpected could happen with the process.
MU: You’re allowing a perfect segue into the next question. When ABEM is trying to ensure fairness and accessibility for all candidates, particularly for those who have unique learning or practice circumstances in their residency program or a personal issue like a disability, how is ABEM anticipating trying to address that and ensure that those candidates are also fairly evaluated?

MU: How do you recommend candidates address potential gaps between their training and the updated certification requirements?
DG: Truly it is making sure you know the model clinical practice of emergency medicine and making sure that you’re getting meaningful feedback in your residency program. A lot of the success in any exam is the comfort with the material moving forward. If you don’t feel comfortable with your

DG: ABEM has always had a very active practice of working with candidates when they have an identified disability. We’ve given extra time in training. We’ve given extra time in assessments. You can petition the board to have a disability considered at any point along the way and we really try to adapt the examination as needed. Now, emergency medicine is emergency medicine. There is a critical skill set and you must be able to complete some of the critical skills within that. But if somebody comes to us with a reasonable request for an adapted exam then we always consider that.


MU: Emergency medicine now is so different even just compared to 10 years ago. How do you feel like these changes align with the currently evolving landscape of emergency medicine and the needs of the U.S. healthcare system?
DG: I think that is one of the key reasons that we really had to move away from the old oral examination into this new version. There are a lot of changes that candidates will notice from the old oral exam to the new certifying exam. The new exam is not going to look the same for the next five or 10 years either. There will be opportunities to adjust and adapt this exam to the changing environment in emergency medicine. For example, AI is one of those key areas. Now, AI is not within the current exam that is going live in 2026. But within a couple of years, we’re really going to have to know how do physicians use external resources like AI on the fly to help with their diagnosis and management of patients? So that’ll be something that this new exam could adapt to that the old exam couldn’t.

psychologist graduating from an emergency medicine residency. But we are expecting you to be able to talk and build rapport with patients. Now, over time, I do anticipate that what ABEM is testing and the emphasis that we’re putting on communication will yield changes in the field of emergency medicine. And will yield to patients saying they want to be cared for by a physician because physicians will listen to them and will manage their care well together.

MU: Are there further plans right now for updates or revisions on the certification process or are we going to get our bearings first and then move from there?
DG: Right. I think we’re walking before we can run.
MU: What impact do you anticipate these changes having on the long-term career development of emergency medicine trainees?
DG: I think that residents should be empowered to say “I’m an investment and my faculty and my program directors need to invest in me.” And that means some individual attention during residency and really a shared responsibility for success. That will help residents be less fearful of assessment and more confident in their training with the certifying exam happening.
MU: Do you feel like there’s going to be any impact on the overall trend of emergency medicine in regard to raising standards of care?
DG: I don’t think there’s any question that the Board’s messaging is that we think communication is a uniquely human skill that will not be replaced by machines. Maybe it will be augmented by machines, but it won’t be replaced by machines. And communication is really coming to the forefront of a critical skill that the Board expects out of emergency physicians. And this is where having the public and patients and their families involved in determining what was required from the certification exam was so important—to have their voices heard. And this is one of the potential threats to physicians leading care of patients in the emergency department that we see. There is a perception that non-physician practitioners are better communicators in medicine than our physicians. However, there is no study or rationale to show why that is. Nonetheless, this is a value that patients and families really hold on to. We have to prove that we are good communicators meaning we must increase the amount of learning that we do in communication as well as the assessment that we do on communication. Now it’s important to remember the criterion referencing. We’re not expecting you to suddenly be a social
MU: I feel empathy is such a core tenant and cornerstone of being a physician and especially in the field of emergency medicine, particularly given so much of our practice is about building good rapport in a short time. So, I do agree that it would be important to emphasize that physicians should be effective and competent communicators. I do appreciate that the purpose of all these changes is to improve the overall excellence of physicians and ensure standardization—that no matter what program you come from, when you pass the ABEM exam, you are a certified emergency medicine physician who can manage critical cases regardless of where you practiced or where you are going to practice afterwards.
DG: Right. Exactly. There are certain tenets that no matter where you practice in emergency medicine, you need to be skilled with them. Procedures is one. Communications is one. Critical decision making is one. Prioritization is one. We’ve really tried to draw all those critical practices that are universal across the field of emergency medicine and say these are the important ones to assess.

MU: It sounds like ABEM is working hard to clarify all the revisions and be transparent about the process and references used. For candidates who are still anxious about these changes, what would you say to them?
DG: First, I would say take a deep breath. We are going to be testing what you have been trained to do. The second thing that I would tell them is to really engage your faculty. Make sure that you are getting observed on the majority of what you’re doing in the emergency department and that you’re getting good critical feedback on that. And the third thing that I would say is to truly familiarize yourself in the material that is already out there. We know that there’s about 3,000 residents in training programs right now. We have videos posted. And so far, some of them have gotten less than 100 views. At minimum, go to the website and read the case descriptions. Read what it says about what the competent candidate will be expected to do and know those bullet points. Know what you are going to be assessed on. I’d really encourage you to do that. I’m a person that watches videos at twice the speed. You could do that too. At least start the videos so that you can see the assessment center itself, as all of them are filmed in the center in Raleigh, North Carolina. You can see what a standardized patient looks like. You can gauge what your interaction with them is going to be. I think a lot of the anxiety behind the exam will go away when you see these examples.
MU: That makes sense. As adult learners, we also have a responsibility to make sure to do our due diligence and review the resources available. As president of ABEM, what is your personal vision for the future of emergency medicine certification?
DG: I think that we are taking such a huge step in what we’re doing right now. I want it to be relevant. I want it to be fair. And I want it to be accessible. I want every residency graduate to feel like they got a fair shake. But above all else, I’m an emergency department patient. You are an emergency department patient. Your family are emergency department patients. I want to have the confidence that no matter where my parents, my children, or my loved ones go, that they are going to be delivered care by a physician who has the capacity to deliver care at the most excellent standard. And that’s what ABEM does. It protects us all as public members. We’re all people first ahead of being physicians, right? We all want the best for our loved ones when they go into an emergency department. And this is what I view as the president of ABEM as being our most important mission—to tell the public we are doing everything that we can to make sure that you get the best care possible.
MU: Yeah, I agree with that sentiment. To safeguard the practice of medicine and to make sure that doctors can protect patients and deliver excellent care. Do you have any words of wisdom or encouragement for candidates preparing to navigate this new process and for their careers overall? We went through a lot of really important information, but any final thoughts that you wanted to leave on?

DG: I will say this. And Mary, I know I’m preaching to the choir talking to you, but I would encourage all residents to get involved with organized medicine. Decide that you’re going to make a difference for your patients. But think about making a difference for emergency medicine at large. Think about ways that you can give back to the specialty that you have chosen above any other field as being the most noble and best field out there. And that can be you getting involved yourself or encouraging your

faculty to get involved. If there is nobody in your training program that is involved with ABEM, ask why. We would love to have a representative from every single residency program within our ABEM volunteer rosters. And if your program doesn’t have an ABEM volunteer at it, perhaps suggest it because we would love to have your voice included. We love the diversity of opinion. We love the camaraderie and the comfort that having an ABEM volunteer at a training program really gives the residents of that program.
MU: I completely agree. I got involved in AAEM and RSA as a firstyear medical student when I happened to attend a student symposium. That was really my first experience within organized medicine, specifically within EM. Since then, it has completely changed me and my trajectory. I cannot overstate how pivotal AAEM has been and continues to be in my development as an emergency medicine trainee—clinically, professionally, and personally. It has been monumental in my growth and meaningful to me to feel so invested in by other EM physicians. I don’t even have the words for how big of an impact it has had on me, which is why I’m a huge advocate for it. I tell every medical student and resident who asks me for advice that regardless of whichever specialty you’re choosing, please join their national groups and get involved. It is as simple as just showing up. I think people get nervous about being new or inexperienced or wondering how to network, but it truly is just simply showing up. Especially now, I feel medicine has become so much more than just clinical care. With the privilege and honor that our position holds, I believe we should take ownership of that privilege and recognize that as physicians we are advocates and leaders who can shape how medicine evolves.
DG: Thank you. If we don’t do it, then somebody else is going to do it and we may not like those outcomes.



To place an ad in the Job Bank: Equitable positions consistent with the Mission Statement of the American Academy of Emergency Medicine and absent of restrictive covenants, will be published (upon approval). All ads run for a six month period or until canceled and will appear in the AAEM member magazine Common Sense and online. For pricing and more information visit www.aaem.org/membership/benefits/ job-bank.
Complete a Job Bank registration form, along with the Criteria for Advertising Section, and submit payment. If you are an outside recruiting agent, the Job Bank Criteria for Advertising must be downloaded and completed by a representative from the recruiting hospital/group.
Direct all inquiries to: www.aaem.org/membership/benefits/job-bank or email info@aaem.org.
For further information on a particular listing, please use the contact information listed.
Section I: Positions listed in Section I are in compliance with elements AAEM deems essential to advertising in our job bank. Fairness practices include democratic and equitable work environments, due process, no post contractual restrictions, no lay ownership, and no restrictions on residency training and have been given the AAEM Certificate of Workplace Fairness.
Section II: Positions listed in Section II are in compliance with elements AAEM deems essential to advertising in our job bank. Fairness practices include democratic and equitable work environments, due process, no post contractual restrictions, no lay ownership, and no restrictions on residency training but have not been given the AAEM Certificate of Workplace Fairness.
Section III: Positions listed in Section III are hospital, non-profit or medical school employed positions, military/government employed positions, or an independent contractor position and therefore cannot be in complete compliance with AAEM workplace fairness practices.
SECTION I: POSITIONS RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK CRITERIA AND GIVEN THE AAEM CERTIFICATE OF WORKPLACE FAIRNESS
Southern Colorado Emergency Medical Associates (SCEMA) is hiring full and part time emergency physicians. SCEMA is a democratic group that began in 1979 based in Southern Colorado staffing UCHealth Parkview Medical Center in Pueblo, CO and UCHealth Parkview Pueblo West Hospital in Pueblo West, CO. SCEMA holds an AAEM Certificate of Workplace Fairness and is an AAEM Physician Group member. Come live and work in the beautiful Front Range of Colorado. We offer a superior financial package with a 2-year partnership track and subsequent income as a partner based upon productivity. Receive a competitive hourly pre-partnership rate of $200/ hour. Part time positions also available with time spent eligible to count towards partnership. Partners average annual total compensation is $491k per year including profit sharing, 401k plan, and a SCEMA funded cash balance plan. Benefits include health insurance, CME, malpractice insurance, compensation for licensing examinations and travel, medical and DEA licensing fees, as well as relocation expenses coverage. Full time status is approximately 13-14 shifts per month with 8-10 hour shifts. Must be BE/BC in emergency medicine. Learn more about our group online at www.scema.info. Please email our VP of Recruiting Dr. Mary Russo at mary.russo@uchealth.org if interested in joining us. Also feel free to reach out to our Medical Director Dr. Tyler Keller at tyler.keller@uchealth.org with any further questions. (PA 2160)
Email: mary.russo@uchealth.org
Join Our Democratic Group in St. Petersburg, Florida: A Unique Opportunity for Emergency Physicians We are seeking dedicated Board Eligible/Board Certified Emergency Physicians to join our democratic group in beautiful St. Petersburg, Florida. This is an extraordinary opportunity to be part of a transparent, accountable organization that prioritizes collaboration and excellence. As a member of the American Academy of Emergency Medicine (AAEM), we adhere to the highest standards of accountability and transparency of a Democratic Group, ensuring that our physicians are empowered and supported in their roles. Why Join Us? This is not just another
job; it’s a chance to help shape the future of emergency medicine in our community. You will have the unique opportunity to open a brand new 24-bed community hospital and two freestanding emergency departments in Wesley Chapel, anticipated to begin operations in Spring/Summer 2026. The physicians we hire will form the foundation for the development and growth of the Emergency Department, setting the culture and expectations from day one. Key Highlights of Our Group: - Democratic Structure: Our group operates on democratic principles, fostering an environment where every physician has a voice and is held accountable for our commitment to transparency. Partnership track available after 3 years of employment, working a minimum of 140hrs/month during those 3 years - New Facilities: Be part of a state-of-the-art 24-bed facility with an expected volume of 4045K visits annually, including approximately 10% pediatric cases. - Anticipated to be an accredited Stroke and STEMI centerWork-Life Balance: We emphasize a lifestyle-focused approach, allowing for balanced schedules to ensure you have ample time to enjoy the stunning world-renowned beaches, beautiful weather, and numerous outdoor activities that Tampa/St. Pete has to offer. - Flexible Scheduling: Prior to partnership, full-time hours average 140 hours per month. Once partnered, full-time is approximately 110 hours per month or more if you choose. - Compensation: $230-240/hr with the following breakdown: $200/hour as a W-2 employee along with a comprehensive benefits package that includes health and 401(k) plan with employer match, profit sharing, holiday bonuses, and a CME budget. Partnership includes RVU pay structure, a more robust CME allowance as well as quarterly dividends and meeting compensation. - Supportive Environment: APP coverage will be provided as volume demands. We are a physician heavy group and utilize our APPs primarily in low acuity/fast track. - EMR: Our facilities utilize Epic for EMR, Dragon for dictation, and Shiftadmin.com for scheduling to ensure streamlined operations.
- Hospital Partnership: Our hospital system is a unique partnership with Orlando Health and Florida Medical Clinic, providing robust support and resources. If you are a passionate Emergency Physician looking to join a democratic group that values transparency, accountability, and work-life balance, we
invite you to consider this exceptional opportunity. Help us shape the future of emergency care in our community and be a part of something truly special. Please see our website which offers a link to apply: https://www.epspbayfront.com (PA 2155)
Email: krystal.mendoza@epspbayfront.com Website: https://www.epspbayfront.com/
The Saskatchewan Health Authority (SHA) and the University of Saskatchewan are seeking a full-time or part-time Pediatric Emergency Physician (0.50 FTE - 1.0 FTE) to join their team in Saskatoon. The successful candidate will provide pediatric emergency services at the Jim Pattison Children’s Hospital, a state-of-the-art facility located on the University of Saskatchewan campus. This academic position includes an assistant professorship with the University. Responsibilities include providing clinical care in the Pediatric Emergency Department, teaching trainees, and participating in research with the Department of Pediatrics. There are opportunities for academic and clinical advancement, as well as involvement in research initiatives. Compensation is through an Alternate Payment Plan (APP), with the opportunity for financial benefits as an independent contractor. Physician benefits are the responsibility of the individual. Qualifications: MD degree Pediatric Emergency Medicine Fellowship Certification or Emergency Medicine Certification Eligible for licensure with the College of Physicians and Surgeons of Saskatchewan Benefits: Physician responsibility Location: Saskatoon, Saskatchewan Language of Work: English To Apply: Please submit your letter of interest and CV to Amanda Lee, Specialist Recruitment and Retention, at amanda.lee@saskhealthauthority.ca. Candidates selected for an interview will be asked for three reference letters, including one from the Fellowship Program Director for recent graduates. SHA is committed to diversity and encourages applications from individuals who contribute to the diversity of our community. Priority will be given to Canadian citizens and permanent residents. (PA 2134)
Email: amanda.lee@saskhealthauthority.ca
Website: https://www.saskhealthauthority.ca/
Job Title: Emergency Medicine Physician – Ultrasound Director/ Core Faculty Position Overview: Washington Regional Medical System is seeking a passionate, dedicated, and experienced individual to join our team as an Ultrasound Director and Core Faculty for a newly accredited Emergency Medicine Residency welcoming residents in June 2026. This is an exciting opportunity to make an impact in a community-focused setting while contributing to both patient care and medical education. We invite you to come build the Ultrasound program you have always wanted! The EM Ultrasound Director will play a critical role in the education and training of residents, in the use of point-of-care ultrasound (POCUS) across a variety of specialties and clinical settings. This individual will be responsible for developing, leading, and delivering ultrasound curriculum, advancing ultrasound education, and actively participating in clinical care. Key Responsibilities • Responsibilities include the practice of emergency medicine, and the provision of care to critically ill and injured patients. • Education and mentorship of residents in emergency ultrasound techniques, enhancing overall training • Create effective curricula and provide handson training for students, residents, and attending physicians in POCUS. • Guide residents through clinical cases involving ultrasound, ensuring competence in both technical skills and clinical decision-making. • Participate in the clinical practice of emergency medicine, utilizing ultrasound as a diagnostic and procedural tool. • Provide quality assurance feedback on both patient care and educational POCUS exams. • Participate in ultrasound-related quality improvement projects within the clinical setting to enhance patient care outcomes. • Maintain upto-date knowledge on advancements in ultrasound technology and best practices in education and clinical care. Required Experience and Competencies • MD or DO degree with board certification in Emergency Medicine • Fellowship training in an EUFAC-accredited fellowship program or Advanced Emergency Medicine with Ultrasonography (AEMUS) Focused Practice Designation or Eligibility • Experience in implementation of ED Ultrasound Billing • Strong commitment to education with proven experience teaching medical students, residents, and/or fellows. • Evidence of scholarly activity, including publications and presentations, in the field of ultrasound is highly desirable. • Proficient in ultrasound-guided procedures, diagnostic applications, and advanced imaging techniques. • Strong clinical skills and the ability to perform in a high-pressure emergency setting. • Excellent communication, leadership, and organizational skills. • Experience with curriculum development, ultrasound administration, and education research preferred.
• Licensed or eligible for licensure to practice medicine in Arkansas. Washington Regional Medical Center – Fayetteville, Arkansas • A community and teaching hospital with a 3-year EM Residency Program affiliated with the University of Arkansas Medical Sciences (UAMS) • Our mission has always been to improve the health of people in the communities we serve. In recent years, we’ve worked to fulfill that mission by:
• Being the area’s only Level II Trauma Center • Starting three new residencies to ensure care for the future • Maintaining the area’s only Comprehensive Stroke Center • TJC’s Gold Seal of Approval for Advance Certification in Spine Surgery • TJC’s Gold Seal of Approval for Hip and Knee Replacement
• US News & World Report – Named as the state’s only High Performing Hospital for Maternity Care (PA 2154)
Email: jfarmer@wregional.com
Website: https://www.wregional.com
Emergency Medicine Residency Program Director with Kaiser Permanente in the California Central Valley The Permanente Medical Group, Inc. (TPMG – Kaiser Permanente Northern California) has an opening to lead our 3-year Residency Program comprised of 8 residents/class for a total of 24 residents, while overseeing 3 assistant PDs, multiple fellowship trained faculty, and GME Program support staff. Must be BC in Emergency Medicine with 5 years as a core faculty member in an ACGME-accredited residency program. View salary and apply at: https://northerncalifornia.permanente.org/jobs/title/ emergency-medicine-residency-program-director-in-modestoca/mod-ac-2500168. Or contact: Roy Hernandez at (510) 4105813 or Roy.B.Hernandez@kp.org. We are an EOE/AA/M/F/D/V Employer. VEVRAA Federal Contractor. (PA 2136)
Email: Roy.B.Hernandez@kp.org
Website: https://northerncalifornia.permanente.org/jobs/title/ emergency-medicine-residency-program-director-in-modestoca/mod-ac-2500168
CALIFORNIA
Hello! Eden Emergency Medical Group is a small independent group that staffs a single small hospital in the Bay Area - Eden Medical Center in Castro Valley. Some quick points about our group and hospital below: - We offer resident education: we have a resident from Highland Hospital most days with a single PGY3 or PGY4 resident shift - Comprehensive stroke center - Level 2 trauma center - High acuity patient population - Services on call: Pediatrics, OB/GYN, General Surgery/ Trauma, Orthopedics, Hand, Urology, GI, Cardiology, Neurology, Neurosurgery, ID, Heme/Onc, Renal, Podiatry, Vascular Surgery, ENT, Ophthalmology, Palliative - Hourly rate: $230/hr + $20/hr bonus for overnight shift, +$20/hr bonus for weekend shift - We offer a productivity bonus & holiday bonus - We offer a 2-year Junior Partnership track - We are a collegial and down-to-earth group of doctors, a lot of us close friends outside of work - We have strong queer and women in medicine representation within our group - We have had our contract with our hospital for > 3 decades We are currently looking for either a FT or PT employee at this time. Please reach out if you are interested! (PA 2145) Email: alexei.adan@gmail.com
Full and Part Time Positions Available in Downtown Los Angeles IEMG is a fully democratic, physician-owned emergency medicine group that has been serving the greater Los Angeles Area for over 40 years. We are looking for part time or full time BC/BE EM physicians to help launch our new site in the heart of downtown Los Angeles at PIH Good Samaritan. There are also opportunities to work in our other region in the Whittier/ Downey area at PIH Whittier and PIH Downey. - 50,000 annual volume - Designations: Primary Stroke and STEMI Receiving Center - Shifts: 8–12 hours with 24/7 APP support - Competitive compensation: $250/hr plus generous night differentialMalpractice coverage with tail - A physician-led, collaborative
The San Francisco VA Health Care System (SFVAHCS) is recruiting a Chief for its Emergency Medicine Section at the SFVA Medical Center. This leadership role oversees a team of approximately 12 physicians and 2 advanced practice providers, plays a key role in clinical care, education, and research. The EM section is part of the Department of Medicine and maintains a strong academic affiliation with the University of California, San Francisco (UCSF). Ideal candidates will have a record of clinical excellence, leadership, teaching, and/or scholarship. For more information, apply online: https://apptrkr.com/6162325 Contact: daniel.wheeler@ucsf.edu or josue.zapata@ucsf.edu (PA 2143) Email: daniel.wheeler@ucsf.edu
Website: https://apptrkr.com/6162325
Hawai’i Pacific Health is a not-for-profit health care network with over 70 locations statewide including medical centers, clinics, physicians and other caregivers serving Hawai’i and the Pacific Region with high quality, compassionate care. Its four medical centers - Kapi’olani, Pali Momi, Straub and Wilcox - specialize in innovative programs in women’s health, pediatric care, cardiovascular services, cancer care, bone and joint services and more. Hawai’i Pacific Health is recognized nationally for its excellence in patient care and the use of electronic health records to improve quality and patient safety. Wilcox Medical Center is looking for a dedicated and detail-oriented Emergency Medicine Physician to join our team in a full-time capacity. As a board-certified/board-eligible physician, you’ll play a vital role in our community-based facility, which serves as a Level III trauma
culture - Physician leadership that values clinical excellence and work-life balance - Shift equity with nights, weekends and holidays (PA 2152) Email: iemgcareers@gmail.com
The Department of Emergency Medicine at UCSF Fresno, in conjunction with Inspire Health Medical Group, is seeking qualified candidates in Emergency Medicine with subspecialty expertise. Candidates should be board-certified or board-eligible in the process of obtaining board certification and must have an active California Medical License or be eligible to apply for one. The applicant must have met all requirements by time of hire. Depending on qualifications, leadership positions exist within the spheres of Ultrasound, Pediatrics, EMS, and Research. The UCSF Fresno Emergency Medicine residency program was founded in 1974 and includes 46 EM residents in a PGY14 format, supported by the UCSF and Community Regional Medical Center (CRMC) in Fresno, California. The faculty group consists of 45 full-time residency trained and board-certified emergency physicians, many with additional fellowship training. CRMC has 630 beds and exceeded 120,000 ED visits last year while being amongst the busiest Level One Trauma Centers in California. CRMC serves as the Base Hospital for a four-county comprehensive EMS System and provides medical direction to the National Park Service. Fresno is the fifth largest city in California and is nestled below the foothills of the Sierra Nevada mountains. Fresno is ideally located for convenient getaways to not only the majestic Sierra but also the scenic Central Coast. Fresno is also the only major city in the country with proximity to three national parks: Sequoia, Kings Canyon and Yosemite. In the heart of California’s agricultural region, Fresno is a dynamic, multi-cultural city with a vibrant community and ever-expanding food scene. Locals can enjoy farmer’s markets, festivals and numerous parks around the city. Many sporting opportunities are available for outdoor enthusiasts including great hiking, mountain biking, fishing, kayaking, trail running and cycling. Contact Stephanie Harrison, Director – Physician Recruitment, stephanie.harrison@inspirehealth.org for more information and to apply. (PA 2163) Email: stephanie.harrison@inspirehealth.org Website: http://inspirehealth.org
Raleigh Emergency Medicine Associates (REMA) is recruiting a partnership track EM trained physician to join our outstanding group. REMA is a stable, independent, twenty-nine physician, democratic emergency medicine group that currently employs ten APPs. - UNC Rex Raleigh , 70,000 visits/yr. - UNC Rex Holly Springs, 35,000 visits/yr. REMA offers a competitive hourly rate and RVU productivity bonus with an excellent benefits package including full medical, disability, and retirement funding. Partner physicians enjoy a full fee-for-service reimbursement structure. The area offers a temperate climate, close to beaches and mountains, several major universities/medical centers, cultural activities, college and professional sports. (PA 2148)
Email: Careers@rema-em.com
Website: https://www.rema-em.com/
center and manages approximately 23,000 emergency visits annually. We seek a compassionate team player committed to providing the highest quality care to the people of Hawai‘i, ensuring exceptional patient satisfaction. Founded in 1938, Wilcox Medical Center is a not-for-profit medical center dedicated to providing the Kaua‘i community with accessible quality health care. The largest medical center on Kaua‘i, it is a state-of-theart acute care facility with a full suite of services offering 30 specialties and programs, including cardiology, emergency, family practice, gastroenterology, health management, internal medicine, neurology, OB-GYN, oncology, orthopedics, pediatrics and urology. Its 18-bed emergency department serves as the island’s Primary Stroke Center. The medical center also has four birthing suites, seven intensive care beds and 20 same-day surgery beds. Wilcox is the first American College of Surgeons-
verified Level III Trauma Center in the state of Hawai‘i. Wilcox is part of Hawai‘i Pacific Health, one of the state’s leading health care systems and a not-for-profit health care organization with medical centers, clinics, physicians and other caregivers working together to create a healthier Hawai‘i. (PA 2161)
Email: melisa.garcia@hphmg.org
Website: http://www.hawaiipacifichealth.org
Hawai’i Pacific Health is a not-for-profit health care network with over 70 locations statewide including medical centers, clinics, physicians and other caregivers serving Hawai’i and the Pacific Region with high quality, compassionate care. Its four medical centers - Kapi’olani, Pali Momi, Straub and Wilcox - specialize in innovative programs in women’s health, pediatric care, cardiovascular services, cancer care, bone and joint services and more. Hawai’i Pacific Health is recognized nationally for its excellence in patient care and the use of electronic health records to improve quality and patient safety. Wilcox Memorial Hospital is currently seeking a full-time board certified/board eligible Emergency Medicine Physician to work in its small, stable EM physician group. If you like working in a close-knit community-based facility with 24K annual census, you will love working with our patients! We are looking for a team player with strong attention to detail with a commitment to delivering the highest quality health care to Hawai‘i’s people with excellent patient satisfaction. Founded in 1938, Wilcox Medical Center is a not-for-profit medical center dedicated to providing the Kaua‘i community with accessible quality health care. The largest medical center on Kaua‘i, it is a state-of-theart acute care facility with a full suite of services offering 30 specialties and programs, including cardiology, emergency, family practice, gastroenterology, health management, internal medicine, neurology, OB-GYN, oncology, orthopedics, pediatrics and urology. Its 18-bed emergency department serves as the island’s Primary Stroke Center. The medical center also has four birthing suites, seven intensive care beds and 20 same-day surgery beds. Wilcox is the first American College of Surgeonsverified Level III Trauma Center in the state of Hawai‘i. Wilcox is part of Hawai‘i Pacific Health, one of the state’s leading health care systems and a not-for-profit health care organization with medical centers, clinics, physicians and other caregivers working together to create a healthier Hawai‘i. (PA 2168)
Email: melisa.garcia@wilcoxhealth.org
Website: http://www.hawaiipacifichealth.org
We are honored with the American Psychiatric Association’s Gold Achievement Award and recognized by the National Alliance on Mental Illness for excellence in psychiatric education, top-tier clinical services, and impactful community outreach. About the Role: Primary Responsibilities: Lead as the Medical Director for both Eastern State Hospital and the EmPATH unit, providing high-quality psychiatric care to adult patients. The EmPATH (Emergency Psychiatric Assessment, Treatment, and Healing) unit is a crisis intervention center that offers a therapeutic alternative to emergency departments for behavioral health crises. Clinical & Teaching Excellence: As part of our faculty, you will engage in a robust mix of clinical care, teaching, and research within UKHC’s state-of-the-art facilities. You’ll mentor medical students, residents, and other healthcare professionals,
contributing to the continued growth of our respected psychiatric program. Our Facilities: Eastern State Hospital: A 239-bed facility with a mission of recovery-focused care, delivering inpatient mental health services across 50 counties. EmPATH Unit: A specialized, 24/7 crisis intervention unit with a welcoming environment for behavioral health, providing rapid assessment and stabilization within a dedicated space. Core Requirements: BE/BC Submit your CV and cover letter to: Sonali Patel, Senior Physician Recruiter UK HealthCare sonali.patel@uky.edu 908938-0764 (PA 2138)
Email: sonali.patel@uky.edu
Website: https://www.uky.edu/
Pediatric Emergency Medicine Physician/Faculty Role Join the University of Kentucky Pediatric Emergency Department Are you passionate about providing exceptional emergency care to children? The University of Kentucky Pediatric Emergency Department is a leading referral center for Central and Eastern Kentucky, serving as one of only two tertiary pediatric centers in the state. As a Trauma Center with over 32,000 annual pediatric ED visits, we are committed to delivering top-tier emergency care to children in need. State-of-the-Art Facilities and Comprehensive Support Our 31-bed department, with additional treatment spaces, is set to expand with a brandnew, state-of-the-art Pediatric ED in the coming years. We offer comprehensive support with 24/7 respiratory therapists, pharmacists, social workers, and dedicated Pediatric ED child life specialists. In-person interpreter services ensure that we provide comprehensive, patient-centered care. Submit your CV to: Karen Kuehn, Sr. Physician Recruiter UK Healthcare Karen. Kuehn@uky.edu 859-323-0198 (PA 2149)
Email: karen.kuehn@uky.edu
Website: https://ukhealthcare.uky.edu/kentucky-childrenshospital
Located in beautiful Windsor, Ontario, Canada, our client, Windsor Regional Hospital (WRH), is situated directly across the border from Detroit, Michigan. WRH is the regional provider of advanced care in complex trauma, renal dialysis, cardiac care, stroke and neurosurgery, and intensive care. WRH is seeking full-time or part-time Emergency Medicine Physicians to contribute to the top tier care provided in the Department of Emergency Medicine. Pathway licensure is easily available for US Board Certified Physicians through WRH and the College of Physicians of Ontario without requirement for supervision. Please forward a CV in confidence to: Robb Callaghan, E-mail: rcallaghan@medfall.com (PA 2159)
Email: rcallaghan@medfall.com
Website: https://www.medfall.com/
Penn State Health is a multi-hospital non-profit health system serving patients and communities across 15 counties in central Pennsylvania. We are seeking exceptional BC/BE Emergency Medicine Physician to join our expanding emergency medicine teams at various locations within our health system. Opportunities available for applicants with ultrasound focus, observation experience, or interest in leadership positions. Opportunities available at Penn State Health Milton S. Hershey
Medical Center, the only Level 1 Adult and Pediatric Trauma Center in PA as well as additional opportunities at our stateof-the-art regional medical centers Penn State Health Holy Spirit and Hampden Medical Centers and Penn State Health Lancaster Medical Center - all providing exceptional care to our communities. What We’re Offering: • Competitive Salary & SignOn Bonus • Comprehensive Total Rewards package with robust retirement options • Relocation Assistance & CME • Work among highly qualified, friendly colleagues • Leadership opportunities What We’re Seeking: • MD, DO or foreign equivalent • BE/ BC by ABEM or ABOEM • Completion of ACGME accredited Emergency Medicine Residency Program • Ability to acquire medical license in the state of Pennsylvania • Observation experience or interest in ultrasound a plus What the Area Offers: Located in a safe family-friendly setting, our local neighborhoods boast a reasonable cost of living whether you prefer a more suburban setting or thriving city rich in theater, arts, and culture. Our community is rich in history and offers an abundant range of indoor and outdoor activities, arts, and diverse experiences. We’re conveniently located within a short distance to major cities such as Philadelphia, Pittsburgh, NYC, Baltimore, and Washington DC. Penn State Health is fundamentally committed to the diversity of our faculty and staff. We believe diversity is unapologetically expressing itself through every person’s perspective and lived experiences. We are an equal opportunity and affirmative action employer. All qualified applicants will receive consideration for employment without regard to age, color, disability, gender identity or expression, marital status, national or ethnic origin, political affiliation, race, religion, sex (including pregnancy), sexual orientation, veteran status, and family medical or genetic information. (PA 2128) Email: hpeffley@pennstatehealth.psu.edu Website: http://www.pennstatehealth.org
Baylor Scott & White Health is seeking an ABEM/AOBEM board certified or eligible Emergency Medicine physician to join an outstanding employment model multispecialty group practice providing direct patient care. The ideal candidate is a hard-working team player with a favorable work and/or training history. Location/Facility: Greater Austin Region including 6 sites Specialty/Department/Practice: Emergency Medicine
Shift/Schedule: Fulltime- 132 hours per month As the largest not-for-profit healthcare system in Texas and one of the largest in the United States, Baylor Scott & White Health includes 52 hospitals, more than 1,300 health system care sites, more than 7,200 active physicians, over 57,000 employees and the Scott and White Health Plan. At Baylor Scott & White, you’ll be joining a team that’s committed to better.?Because better never settles. And neither should you.? QUALIFICATIONS: • Doctorate Degree in Medicine • Licensed to Practice Medicine in the state of Texas by the Texas Medical Board • The perspective employee shall be board certified in emergency medicine or demonstrate active pursuit of board certification as defined by the American Board of Emergency Medicine or the American Osteopathic Board of Emergency Medicine. For additional information, contact: Tara Moore, Physician Recruiter, at Tara.Moore@BSWHealth.org (PA 2150)
Email: Tara.Moore@BSWHealth.org
Website: https://jobs.bswhealth.com/us/en/


